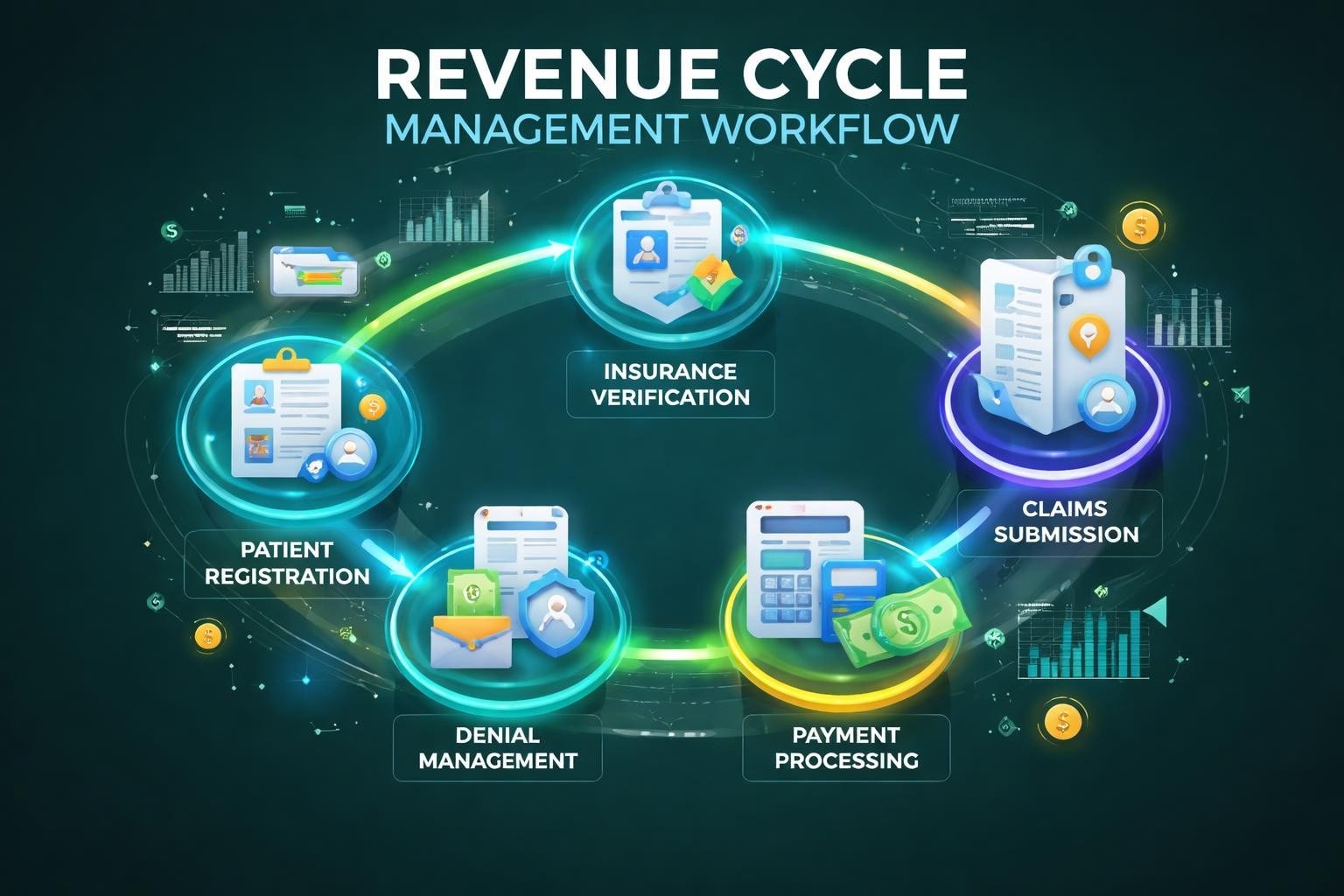
The financial health of any healthcare practice depends on one critical component: an efficient revenue cycle process. This complex system encompasses every administrative and clinical function that contributes to capturing, managing, and collecting patient service revenue. For healthcare providers, understanding each stage of this process is essential for maintaining steady cash flow, reducing claim denials, and ensuring operational sustainability. The revenue cycle process represents the lifeblood of healthcare financial management, connecting patient care delivery directly to practice profitability.
Understanding the Revenue Cycle Process Framework
The revenue cycle process represents a comprehensive sequence of events that begins before a patient walks through the door and continues until the practice receives full payment for services rendered. Unlike retail transactions where payment occurs immediately, healthcare revenue collection involves multiple stakeholders, regulatory requirements, and verification steps that can extend the process over weeks or even months.
Healthcare practices face unique challenges in managing this process. Third-party payers introduce complexity through varying coverage requirements, reimbursement rates, and documentation standards. Regulatory compliance demands meticulous attention to coding accuracy and billing practices. Patient responsibility portions continue to grow, requiring practices to develop effective patient payment strategies alongside traditional insurance billing.
The Financial Impact of Process Efficiency
When practices optimize their revenue cycle process, they experience measurable improvements in key performance indicators. Days in accounts receivable decrease, collection rates improve, and denial rates decline. These improvements translate directly to better cash flow and reduced administrative burden on clinical staff.
Key benefits of an optimized revenue cycle process include:
- Accelerated payment collection timelines
- Reduced claim denial and rejection rates
- Improved patient satisfaction through transparent billing
- Enhanced compliance with payer requirements
- Better financial forecasting and planning capabilities
Organizations that invest in comprehensive denial management services typically see substantial returns through recovered revenue and prevented future denials.
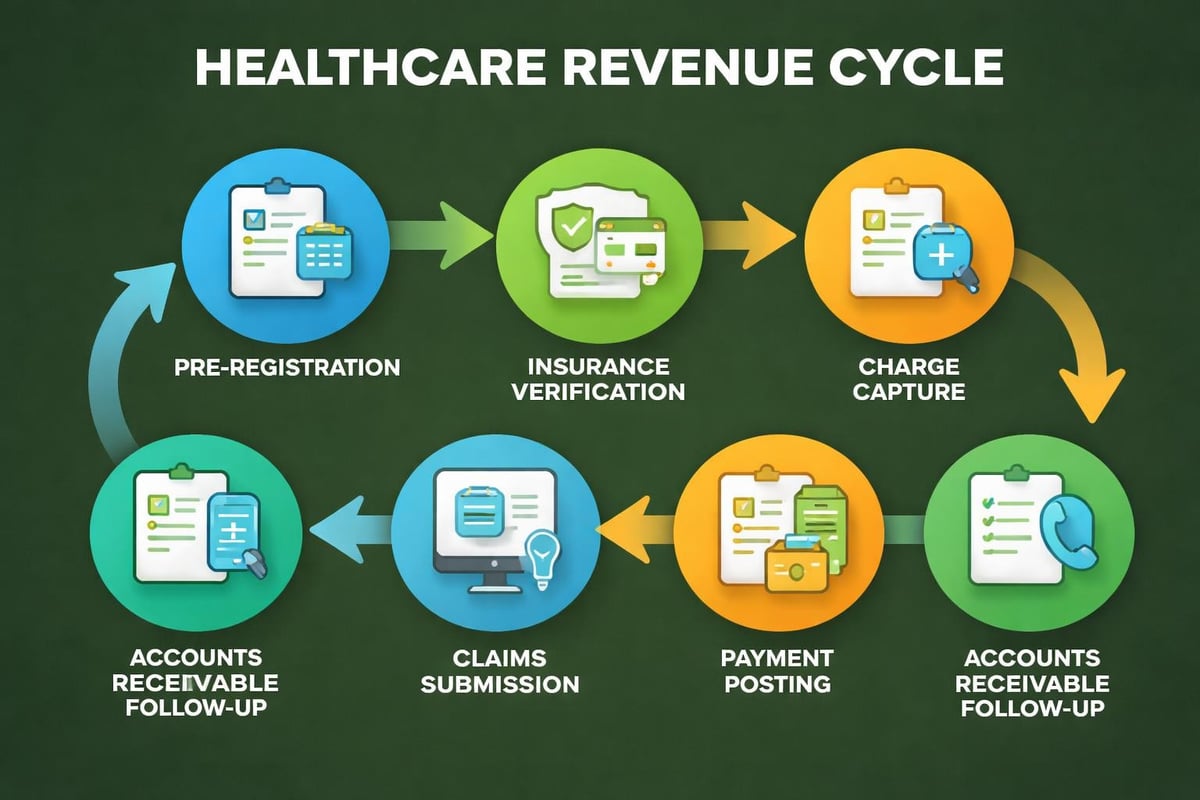
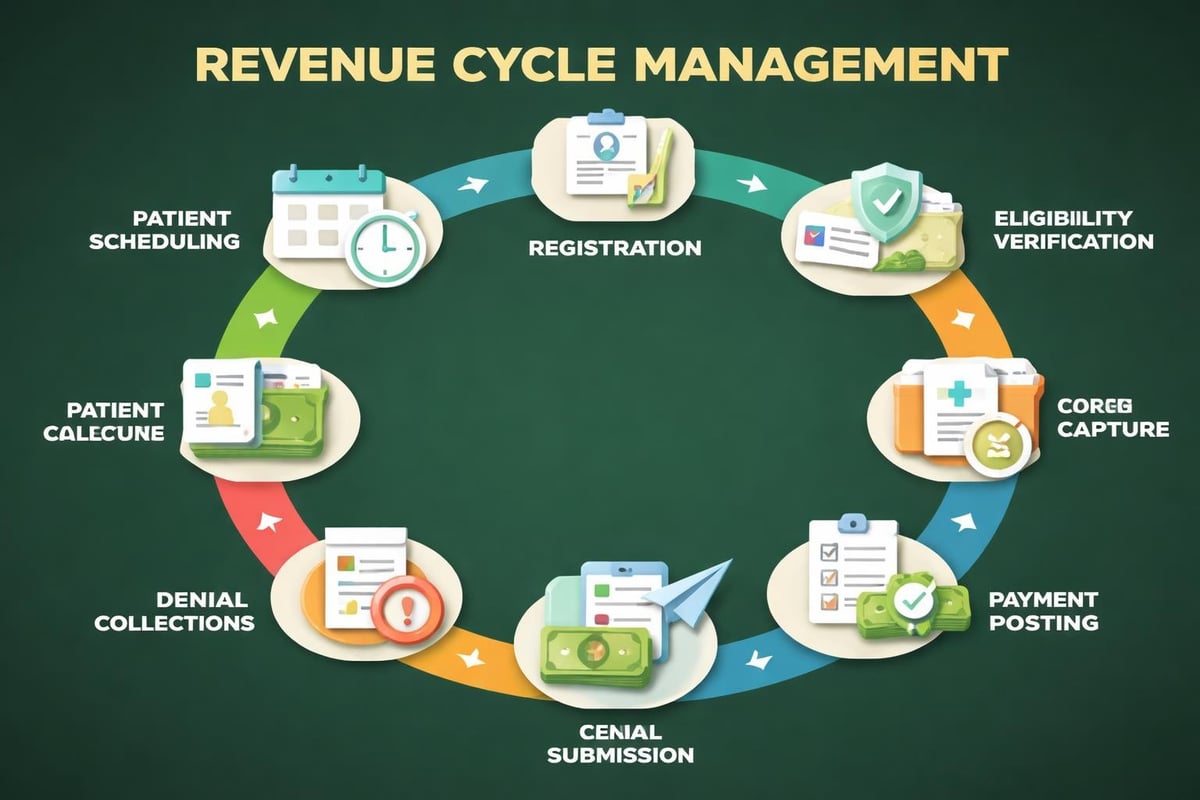
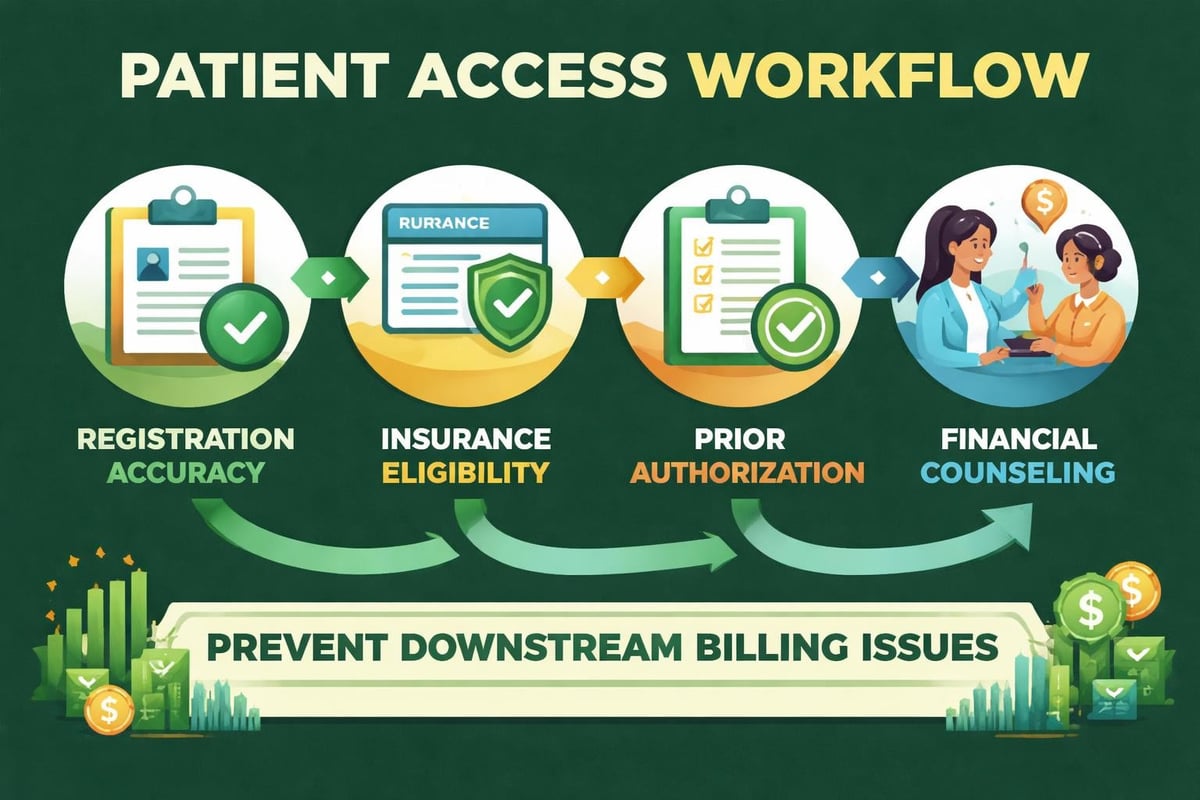
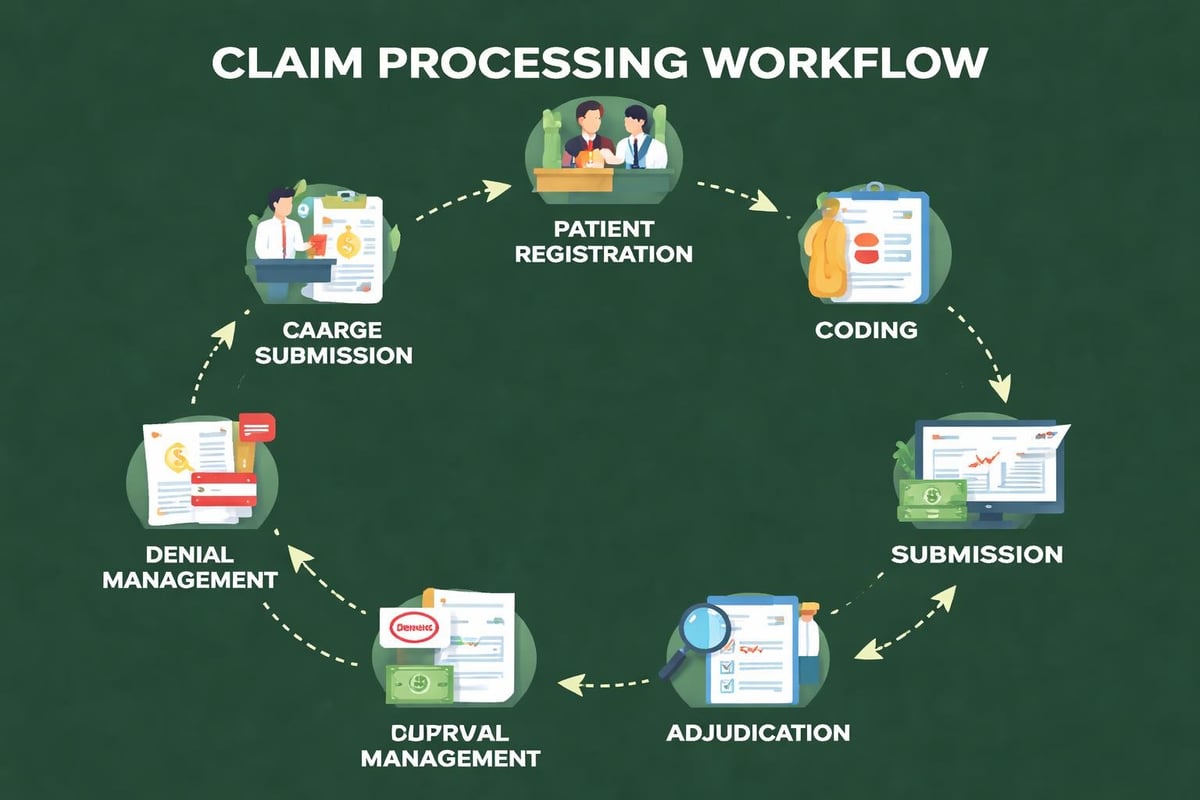
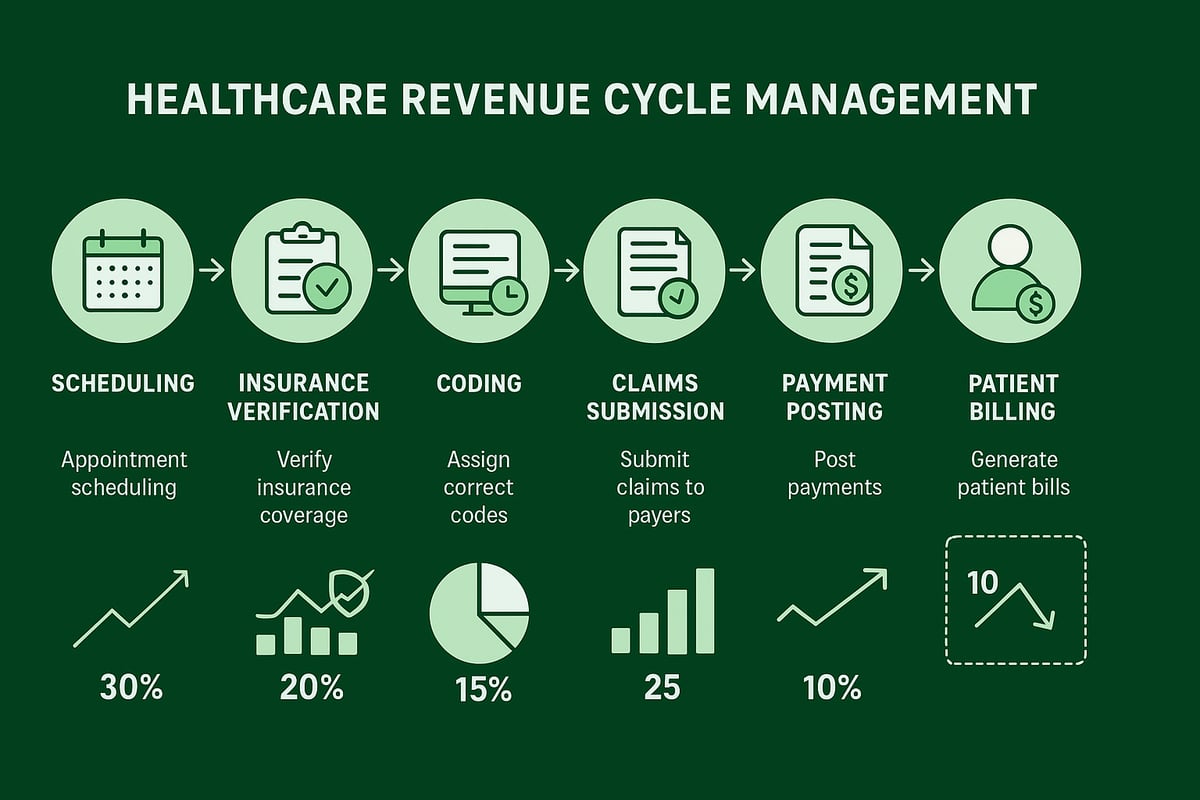
Stage One: Patient Access and Registration
The revenue cycle process begins with patient access, which encompasses all activities from initial appointment scheduling through registration completion. This foundational stage sets the tone for the entire billing process and directly impacts downstream collection success.
During patient scheduling, practices should collect essential demographic information and verify insurance coverage. Front desk efficiency at this stage prevents numerous problems later in the cycle. Staff must confirm patient identity, gather complete contact information, and document insurance details with precision.
Critical Registration Elements
| Registration Component | Purpose | Impact on Revenue |
|---|---|---|
| Demographic Data | Patient identification and communication | Prevents claim rejections due to incorrect information |
| Insurance Information | Coverage verification and billing | Ensures claims route to correct payers |
| Authorization Requirements | Pre-service approval | Prevents claim denials for unauthorized services |
| Financial Policies | Payment expectations | Improves patient payment collection |
Practices utilizing professional eligibility verification services ensure accurate coverage confirmation before services are delivered, significantly reducing claim denials related to eligibility issues.
Stage Two: Insurance Eligibility and Authorization
Insurance verification represents a critical checkpoint in the revenue cycle process. This stage confirms that patients have active coverage, identifies specific plan benefits, and determines patient financial responsibility before services are rendered.
Real-time eligibility verification has become standard practice for efficient revenue cycle management. Through electronic payer connections, practices can instantly confirm coverage status, deductible amounts, copayment requirements, and coinsurance percentages. This information allows staff to collect accurate patient payments at the time of service.
Authorization Management
Certain procedures and services require prior authorization from insurance companies. Securing these approvals before delivering care is essential for ensuring payment. The authorization process involves submitting clinical documentation that demonstrates medical necessity according to payer criteria.
Practices benefit from implementing systematic prior authorization services that track authorization requirements, submission deadlines, and approval status. According to comprehensive financial management practices, effective authorization management prevents an estimated 30-40% of preventable denials.
- Identify services requiring authorization based on payer policies and CPT codes
- Gather supporting documentation including clinical notes and diagnostic reports
- Submit authorization requests within payer timeframes
- Track approval status and follow up on pending requests
- Document authorization numbers in the patient record for billing reference
Stage Three: Clinical Documentation and Charge Capture
Once patient care is delivered, the revenue cycle process moves to documentation and charge capture. Providers must record all services, procedures, and supplies used during patient encounters. This clinical documentation serves as the foundation for accurate coding and compliant billing.
Complete documentation must support the level of service billed and demonstrate medical necessity for all procedures. Incomplete or ambiguous documentation leads to claim denials, compliance risks, and lost revenue from undercoded services.
Charge Capture Systems
Effective charge capture ensures that all billable services are recorded and submitted for reimbursement. Practices lose significant revenue when services are performed but never charged due to documentation gaps or workflow breakdowns.
Modern charge capture relies on integrated systems that connect clinical documentation directly to billing processes. When providers document services in electronic health records, charge capture systems automatically generate billing entries based on documented procedures and diagnoses.
- Electronic health record integration streamlines charge entry
- Charge description masters standardize service pricing
- Charge reconciliation processes identify missing charges
- Provider education reduces charge capture errors
Stage Four: Medical Coding and Compliance
Medical coding translates clinical documentation into standardized codes used for billing and data analysis. Professional coders assign diagnosis codes (ICD-10), procedure codes (CPT), and supply codes (HCPCS) based on provider documentation. The accuracy of this coding directly impacts claim payment success.
The revenue cycle process depends on coding precision. Upcoding (billing for more complex services than documented) and undercoding (failing to capture the complete service level) both create problems. Upcoding triggers compliance issues and potential audits, while undercoding leaves money on the table.

| Coding Element | Purpose | Common Challenges |
|---|---|---|
| ICD-10 Diagnosis Codes | Document patient conditions | Specificity requirements, combination coding |
| CPT Procedure Codes | Describe services performed | Bundling rules, modifier requirements |
| HCPCS Supply Codes | Identify equipment and supplies | Coverage limitations, medical necessity |
| Modifiers | Clarify special circumstances | Proper selection and sequencing |
Organizations investing in professional medical coding services ensure experienced coders handle this critical function using current coding guidelines and payer-specific requirements.
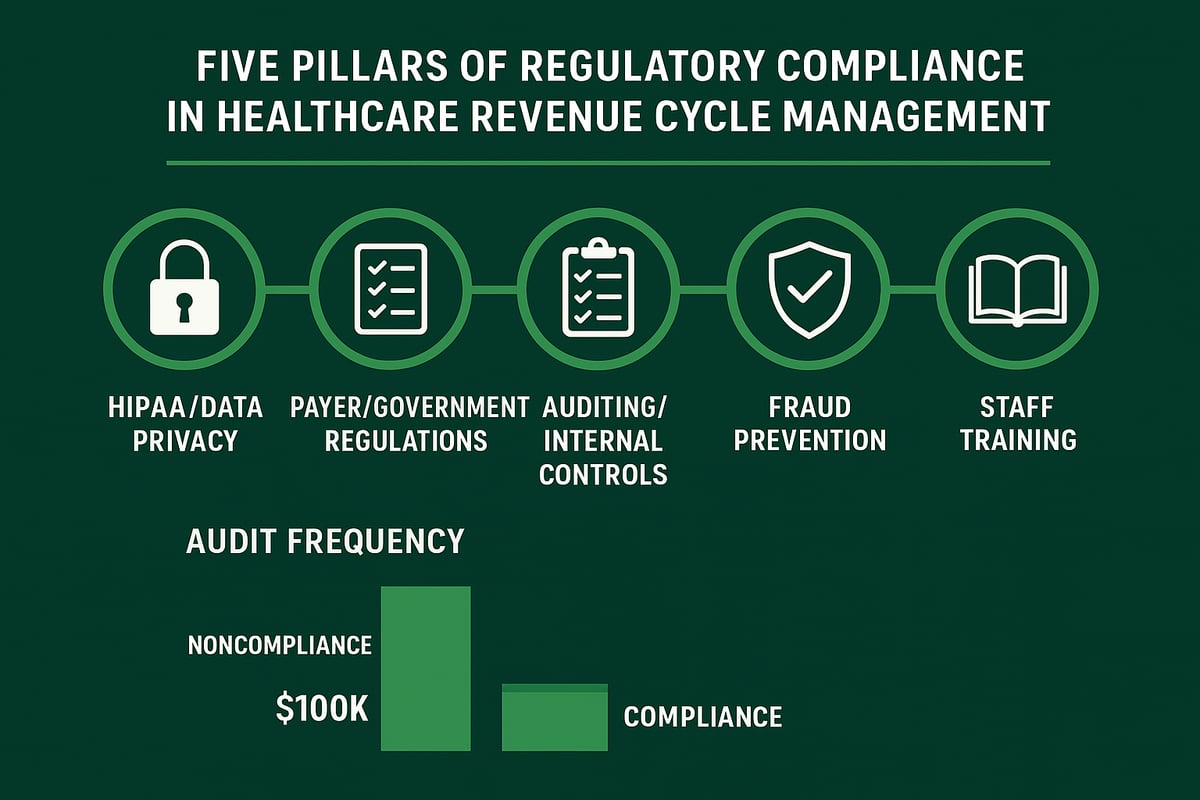
Coding Compliance and Audit Prevention
Regular coding audits identify patterns of errors and opportunities for coder education. Best practices include reviewing a random sample of coded encounters monthly, comparing coding patterns against national benchmarks, and addressing identified issues through targeted training.
Stage Five: Claims Submission and Management
Claims submission represents the formal request for payment sent to insurance companies. The revenue cycle process reaches a critical milestone at this stage, as properly prepared claims move smoothly through payer adjudication while problematic claims face rejection or denial.
Clean claims contain accurate patient demographics, valid insurance information, appropriate codes, and complete supporting documentation. Industry benchmarks suggest practices should achieve clean claim rates of 95% or higher on initial submission.
Before transmission, claims undergo scrubbing processes that identify common errors like invalid code combinations, missing modifiers, or demographic mismatches. Automated scrubbing software checks claims against thousands of payer-specific edits, catching errors before submission.
Electronic vs. Paper Claim Submission
Electronic claims submission has become the standard in healthcare billing, offering faster processing, reduced errors, and improved tracking capabilities. Electronic claims typically process in 7-14 days compared to 30-45 days for paper claims.
Professional medical claim submission services manage the technical requirements of electronic submission across hundreds of payers, ensuring claims reach the right destination in the correct format.
- Generate clean claims from coded encounters with complete documentation
- Run claim scrubbing software to identify errors before submission
- Transmit claims electronically through clearinghouse connections
- Monitor submission acknowledgments confirming payer receipt
- Track claim status through adjudication and payment
Stage Six: Payment Posting and Reconciliation
When payers process claims, they generate remittance advice documents explaining payment decisions. Payment posting involves recording these payments, adjustments, and denials in the practice management system. Accurate posting is essential for maintaining current account balances and identifying issues requiring follow-up.
The revenue cycle process includes both electronic remittance advice (ERA) and explanation of benefits (EOB) documents. ERAs provide structured data that can be automatically posted, while paper EOBs require manual data entry. Understanding what ERAs are in medical billing helps practices improve posting efficiency.
Contractual Adjustments and Patient Responsibility
Insurance payments typically include contractual adjustments representing the difference between billed charges and contracted rates. These adjustments must be posted accurately to maintain correct account balances. Following insurance payments, remaining balances transfer to patient responsibility.
Payment posting best practices include:
- Daily posting of all payments and adjustments
- Separate posting of insurance and patient payments
- Verification of posted amounts against remittance documents
- Investigation of unexpected denials or adjustments
- Transfer of remaining balances to appropriate responsibility party
Organizations utilizing payment posting services ensure timely and accurate payment application, accelerating cash flow and improving financial reporting accuracy.
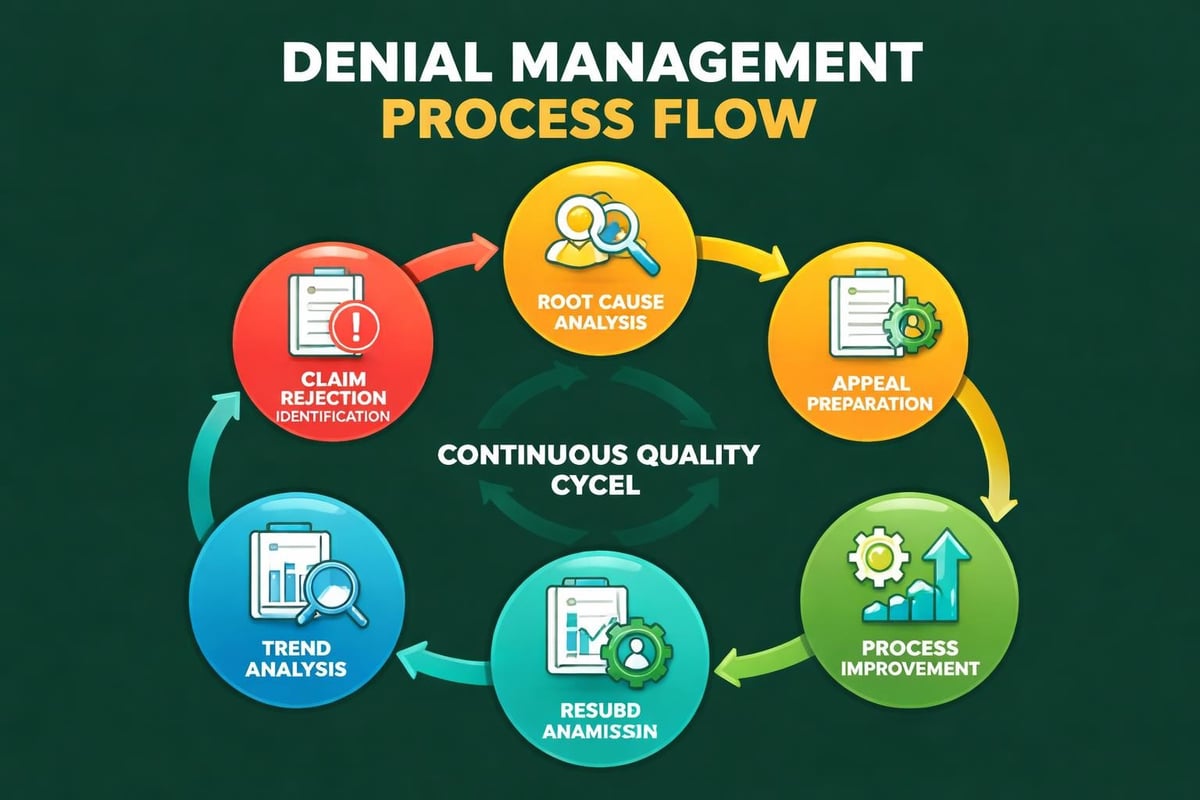
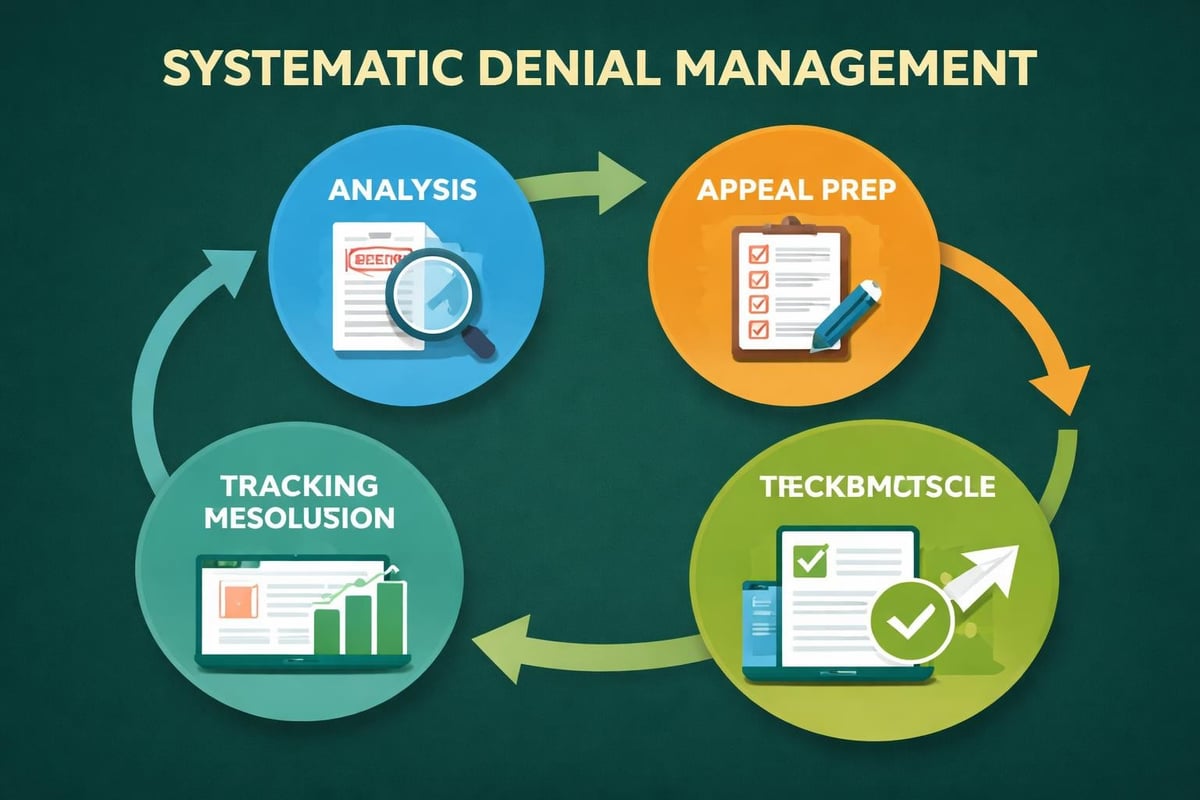
Stage Seven: Denial Management and Appeals
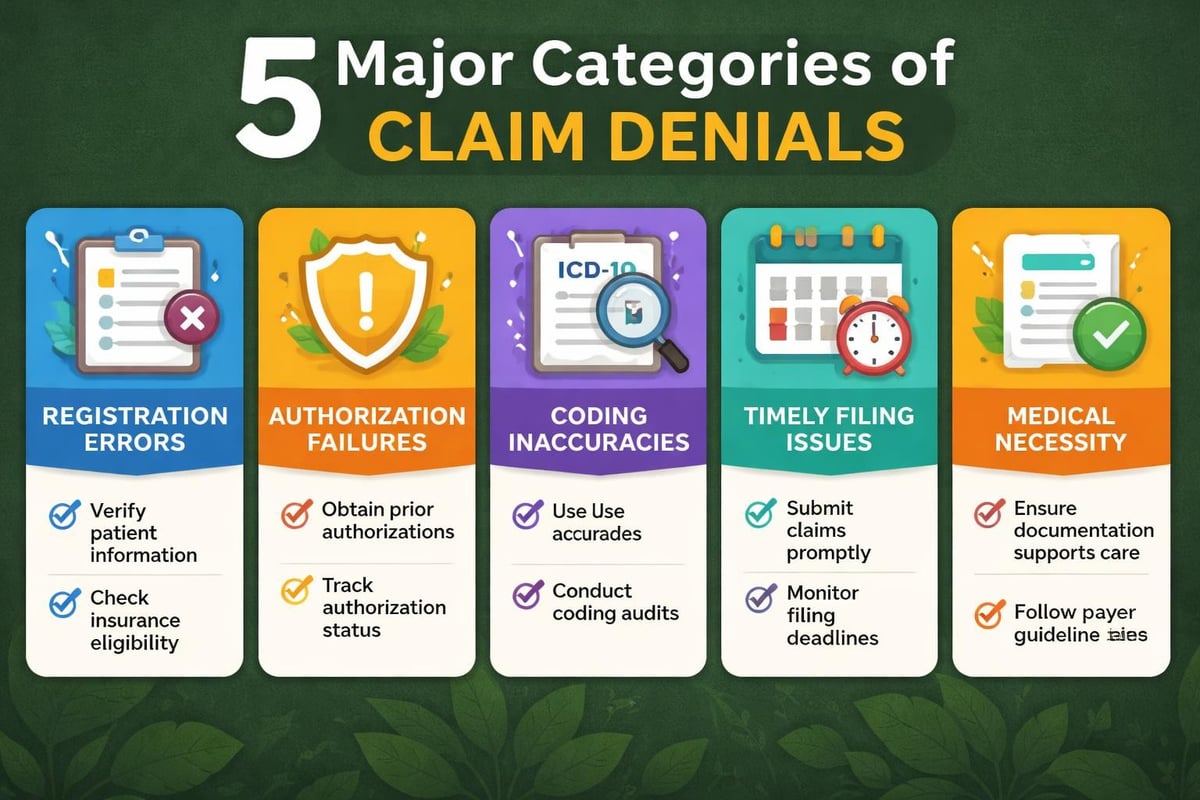
Not all claims result in immediate payment. Payers deny claims for numerous reasons including eligibility issues, coding errors, lack of medical necessity, or missing authorization. The revenue cycle process must include systematic denial management to recover this revenue.
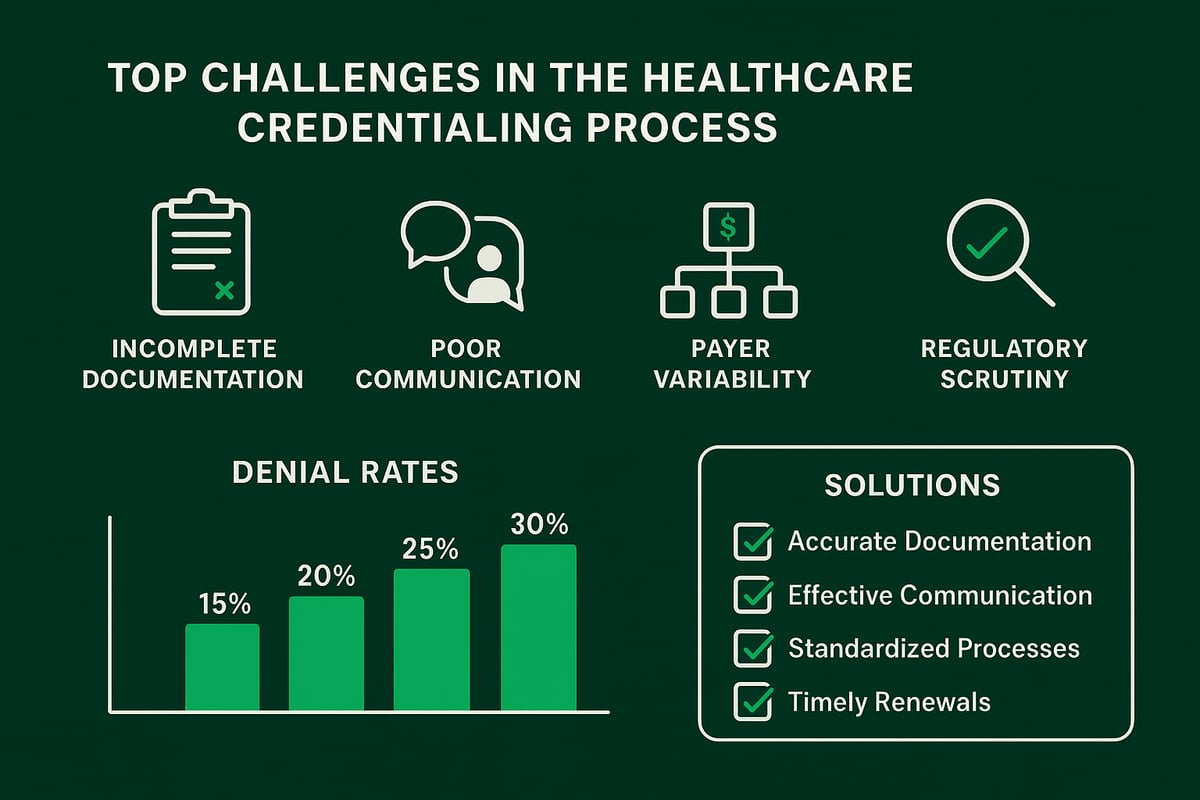
Denial rates vary by specialty and payer but typically range from 5-15% of submitted claims. The best practices for streamlining revenue cycle management emphasize the importance of tracking denial patterns and addressing root causes.
Denial Categories and Response Strategies
| Denial Type | Common Causes | Resolution Approach |
|---|---|---|
| Technical Denials | Missing information, invalid codes | Correct errors and resubmit |
| Clinical Denials | Medical necessity, authorization | Submit clinical documentation and appeal |
| Eligibility Denials | Coverage termination, incorrect policy | Verify coverage and rebill correct payer |
| Timely Filing Denials | Late submission | Request filing extension or write off |
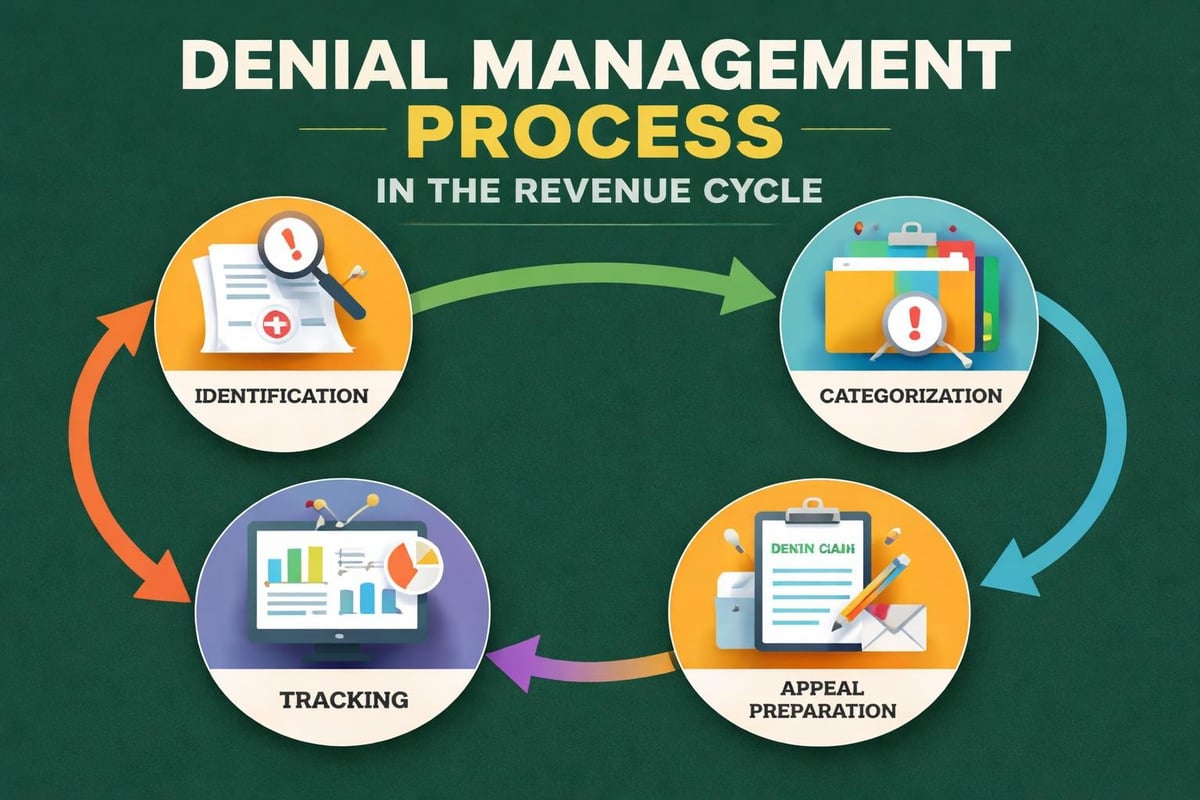
Effective denial management includes identifying denials immediately upon receipt, categorizing them by type and reason, prioritizing high-value denials for appeal, and tracking appeal outcomes. Many practices find that partnering with specialists in denial management significantly improves recovery rates.
Stage Eight: Patient Collections and Communication
Patient financial responsibility continues to grow as high-deductible health plans become more common. The revenue cycle process must include patient collection strategies that balance revenue recovery with patient satisfaction.
Upfront collections at the time of service prove most effective for securing patient payments. When staff collect copayments, deductibles, and previous balances before services are rendered, collection rates exceed 90%. Post-service collection rates typically fall below 50%.
Patient Payment Plans and Financial Policies
Clear financial policies help patients understand their obligations and available payment options. Practices should communicate these policies during scheduling, confirm them at check-in, and provide written documentation.
For patients facing difficulty paying their balances, payment plans offer a viable solution. Structured payment arrangements allow patients to meet their obligations over time while ensuring practices receive payment. Best practices suggest requiring initial down payments of 20-30% with monthly installments completing payment within 6-12 months.
- Estimate patient responsibility before service delivery using verified benefits
- Collect copayments and deductibles at the time of service
- Send timely patient statements for remaining balances after insurance payment
- Offer payment plan options for patients unable to pay in full
- Maintain consistent collection follow-up through calls and letters
Stage Nine: Accounts Receivable Management
Outstanding claims and patient balances require systematic follow-up to ensure timely collection. Accounts receivable (AR) management represents the final stage of the revenue cycle process, focusing on aging claims and unpaid balances.
Industry benchmarks suggest that accounts receivable over 90 days old should represent less than 15% of total AR. Claims aging beyond this threshold become increasingly difficult to collect, with recovery rates declining sharply after 120 days.
AR Prioritization Strategies
Effective AR management prioritizes follow-up efforts based on claim value, aging category, and collection probability. High-dollar claims receive immediate attention, while small-balance accounts may be batched for efficient processing.
Many practices track essential revenue cycle management metrics to monitor AR performance and identify improvement opportunities. Key metrics include days in AR, AR aging percentages, and collection ratios.
Critical AR management activities include:
- Weekly review of aging reports identifying claims requiring action
- Payer follow-up on unpaid claims beyond standard processing timeframes
- Patient outreach on overdue balances through calls and statements
- Account resolution through payment, appeal, or write-off decisions
- Documentation of all collection activities and outcomes
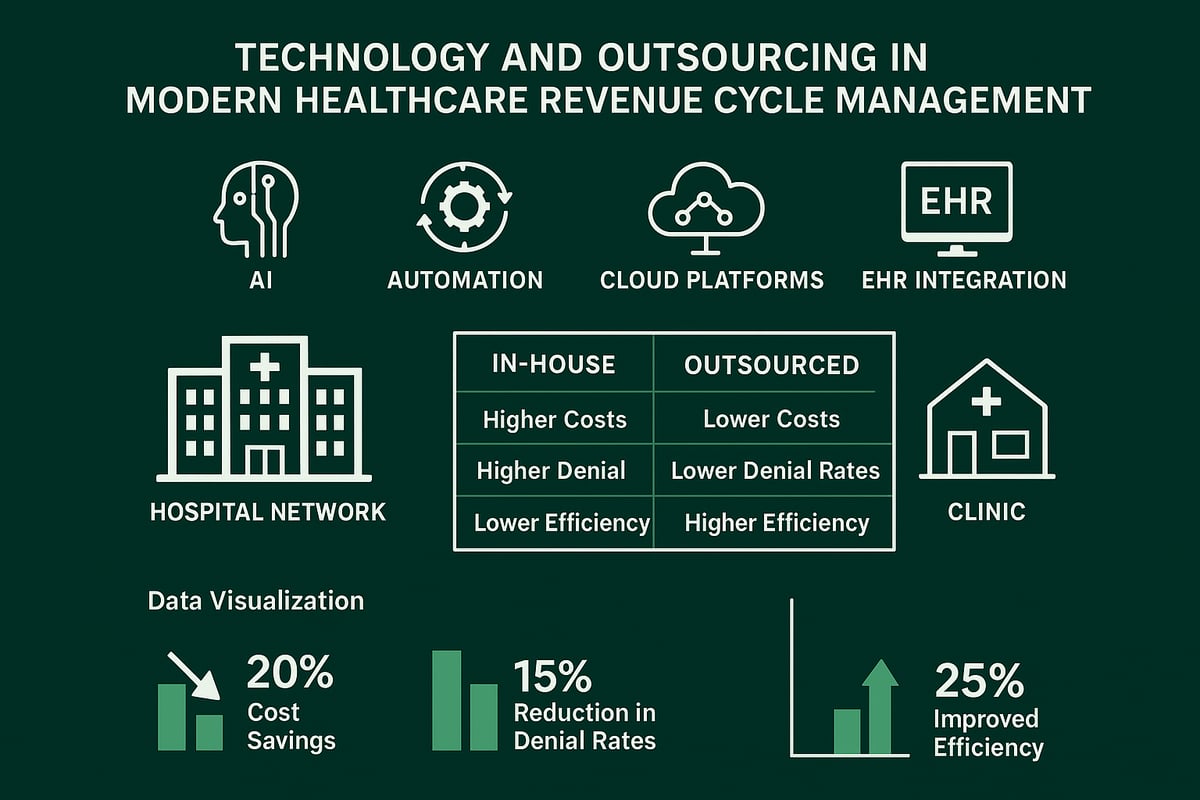
Technology and Automation in the Revenue Cycle Process
Modern revenue cycle management relies heavily on technology platforms that automate repetitive tasks, reduce errors, and provide actionable insights. While the fundamental revenue cycle process remains consistent, technology dramatically improves efficiency and accuracy.
Practice management systems serve as the central hub for revenue cycle activities, storing patient demographics, insurance information, charge data, and payment history. Integration with electronic health records eliminates duplicate data entry and ensures coding accuracy through documentation access.
Revenue Cycle Analytics and Reporting
Data analytics transform raw billing information into actionable intelligence. Comprehensive revenue cycle reports help practices identify bottlenecks, monitor key performance indicators, and make informed decisions about process improvements.
Advanced analytics identify patterns invisible to manual review, such as specific payers with consistently high denial rates, particular procedure codes with frequent coding errors, or individual providers with documentation deficiencies.
Organizations implementing reporting and analytics capabilities gain visibility into their revenue cycle performance and can proactively address emerging issues before they significantly impact cash flow.
Optimizing Your Revenue Cycle Process
Continuous improvement represents the hallmark of successful revenue cycle management. Practices should regularly assess their performance against industry benchmarks and implement targeted improvements to address identified gaps.
Performance improvement begins with measurement. Establishing baseline metrics for key performance indicators allows practices to track improvement over time and quantify the impact of process changes. Essential metrics include clean claim rates, days in accounts receivable, collection rates, and denial percentages.
Following the seven steps of revenue cycle management provides a structured framework for optimization efforts. These steps guide practices through systematic assessment, planning, implementation, and monitoring of revenue cycle improvements.
Staff Training and Development
Well-trained staff execute revenue cycle processes more effectively and adapt more readily to changing payer requirements. Regular training on coding updates, payer policy changes, and system enhancements keeps teams current and competent.
Cross-training staff across multiple revenue cycle functions improves operational flexibility and provides backup coverage during absences. When registration staff understand downstream impacts of incomplete information, they capture more complete data upfront.
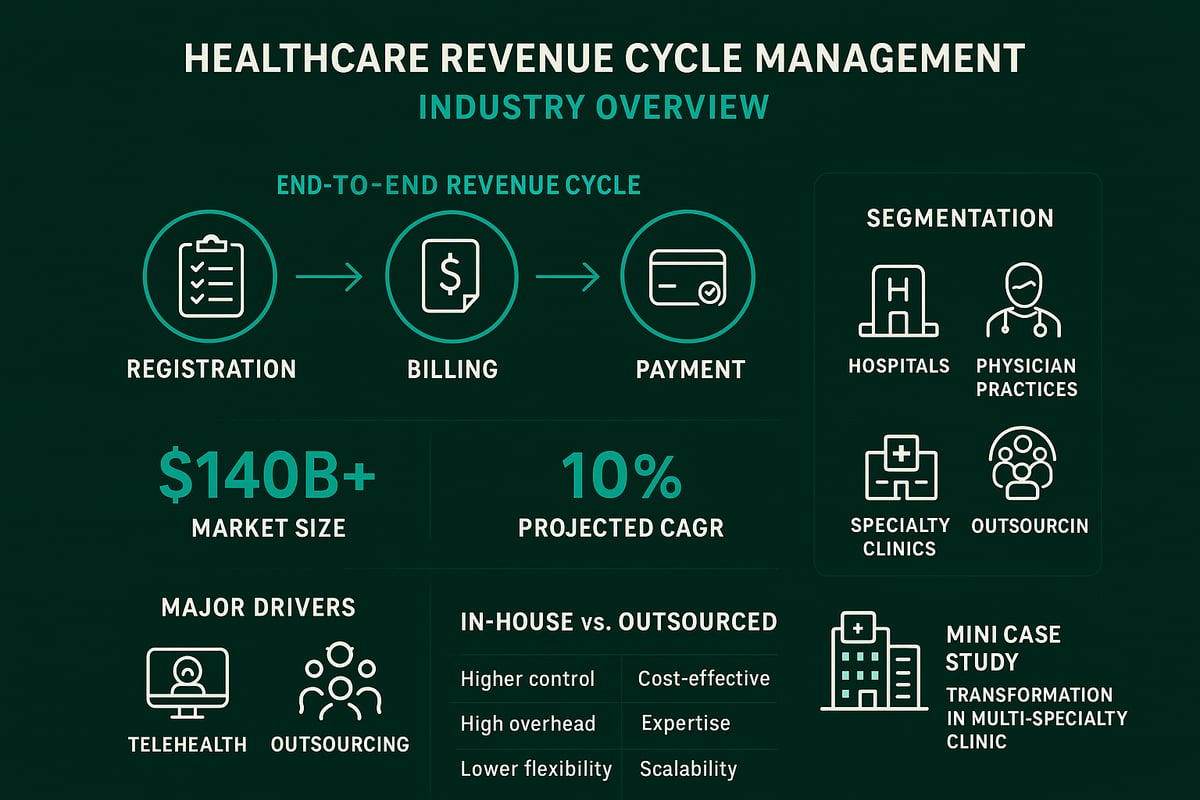
Outsourcing Considerations in Revenue Cycle Management
Many healthcare practices partner with specialized revenue cycle management companies to improve performance while allowing clinical staff to focus on patient care. Outsourcing decisions should consider practice size, current performance levels, available internal resources, and strategic priorities.
Specialized service providers bring expertise, technology, and dedicated staff focused exclusively on revenue cycle functions. They maintain current knowledge of payer requirements across hundreds of insurance companies, invest in sophisticated billing platforms, and employ experienced coders and billers.
Practices may outsource the entire revenue cycle process or specific functions like coding, claims submission, or denial management. Hybrid approaches allow practices to maintain control over patient-facing functions while outsourcing back-office technical processes.
When evaluating potential partners, practices should assess experience in their specialty, technology capabilities, reporting transparency, and cultural fit with practice values.
Mastering the revenue cycle process requires attention to detail at every stage, from initial patient contact through final payment collection. By understanding each component and implementing best practices throughout the cycle, healthcare practices can significantly improve their financial performance. Greenhive Billing Solutions specializes in comprehensive revenue cycle management services that help healthcare providers optimize every stage of this critical process, from insurance verification and claims processing to denial management and AR follow-up. Our experienced team works seamlessly with your existing systems to enhance efficiency, reduce denials, and maximize reimbursements while ensuring complete HIPAA compliance.