Prior Authorization Services
Boosting Healthcare Practice's
Revenue & Patients
What You Get with Our Prior Authorization Services
Complete Prior Auth Management
We manage the full authorization workflow, from documentation to payer follow-up so you get timely approvals and fewer care disruptions.
Approval for Meds and Services
We handle prior auths for medications, labs, imaging, and surgeries, reducing delays and helping patients start treatment without hassle.
Support for Appeals and Denials
If an auth is denied, we investigate, collect missing details, and submit a strong appeal to recover your claim and revenue.

Prior Authorizations Made Easy
Why Healthcare Providers Trust Greenhive Billing Solutions
At Greenhive Billing Solutions, we specialize in prior authorization for medical services, supporting healthcare providers across the USA. Our expert team manages the entire process, from submission to follow-up, ensuring approvals are obtained as quickly as possible.
- Dedicated team that handles every request accurately
- Faster approvals leading to timely patient care
- Reduced claim denials with our management services and revenue leakage
- Compliance with ever-changing payer policies
- Seamless communication with your office and staff
We help you focus on patient care while we handle the paperwork.
Every Step, Managed
Our Complete Prior Authorization Workflow
Greenhive Billing Solutions offers a complete set of solutions to verify health insurance coverage and ensure smooth billing operations:
- Authorization Request Intake
- Verification of Insurance Requirements
- Document Collection and Submission
- Continuous Payer Follow-Up
- Approval Notification to Provider
- Denial Management and Appeals (if necessary)
To make sure approved services convert to revenue, our Medical Billing Services and Claim Submission & Reimbursement teams take over seamlessly.
SERVICES
Delayed Authorizations Are Costing You More Than You Think
Every day your office spends chasing insurance companies for approvals, you lose revenue, staff time, and patient trust. Denied or delayed authorizations do not just create paperwork headaches. They disrupt care, delay treatments, and can cause patients to turn elsewhere. That is why working with professional prior authorization companies like Greenhive Billing Solutions is critical to resolved prior authorization challenges faced by providers.
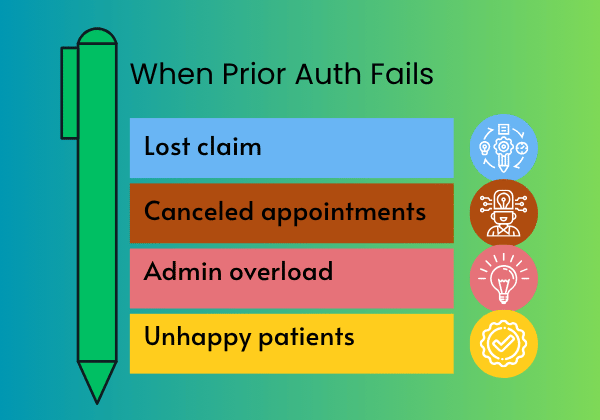
Inefficiency Hurts Payments and Patients
Why Inefficient Prior Authorization Hurts Your Revenue Cycle
For healthcare providers, clinics, and physicians, managing prior authorization for medical services is a growing burden. Insurance requirements are constantly changing. If your staff misses even a minor update, your claims may be denied or delayed, directly affecting your cash flow. Rejected authorizations often lead to:
- Revenue loss from unpaid claims
- Rescheduled or canceled appointments
- Increased administrative workload
- Decreased patient satisfaction
Simplifying Prior Authorization
What Is Prior Authorization and Why Is It So Complex?
Pre authorization services are insurance company requirements where providers must get approval before delivering certain treatments, tests, or medications. Without it, insurance may refuse payment. Each insurer has different rules, timelines, and required documents, making the process complicated and time-consuming.
Our experienced prior authorization department stays current with payer requirements, reducing delays and denials for your practice.
BENEFITS
Benefits of Prior Authorization Services
Fewer Treatment Delays
We help avoid last-minute cancellations caused by pending authorizations.
Lower Claim Denial Rates
By submitting complete & accurate requests , we prevent costly rework & rejected claims.
Less Time Spent on Follow-Ups
Your staff won’t need to call insurers multiple times, we handle the back-and-forth.
Faster Cash Flow
When prior auths are done right the first time, your claims are paid sooner, without interruption.
Medication Prior Authorization: Avoid Costly Delays for Your Patients
Pharmacies and providers often face challenges with medication pre authorization, especially for high-cost drugs. Our experts work directly with payers to ensure patients receive needed medications without unnecessary delays or out-of-pocket expenses. By using our preauthorization healthcare service, you avoid treatment interruptions and keep patients on their care plans.
Pre-Approval Health Insurance Navigation
Navigating pre-approval health insurance rules can be overwhelming. Each insurance company uses different forms, codes, and review times. We relieve your staff of the burden by managing insurer communications, submitting accurate medical coding documentation, and tracking approvals at every stage. If claims are still delayed post-approval, our AR services step in to ensure timely follow-up and collections.
OUTCOMES
We Help You Target the
Right Outcomes

Stop Denials Before They Happen
Take Control of Your Revenue Cycle Today
ANY QUESTIONS?
Frequently Asked Questions
What are prior authorization services?
Why do healthcare providers outsource prior authorization?
How does prior authorization affect revenue?
What is medication pre authorization?
Does Greenhive Billing Solutions handle appeals?
Yes, we manage denial appeals by identifying errors, gathering supporting documents, and resubmitting requests to insurance payers.
WE SUPPORT
Serving Providers Across the USA
Based in Tempe, Arizona, Greenhive Billing Solutions serves providers, clinics, and practices nationwide. Whether you are a small practice or a large healthcare network, our scalable solutions fit your needs and help maximize your revenue.
