Denial Management Services for Healthcare Providers
Turn Denied Claims into
Paid Claims, Fast
Why Healthcare Providers Trust Our Denial Management Expertise
Full-Service Denial Recovery
Payer-Specific Expertise
Proactive Denial Prevention

Stop Revenue Leakage
Why Healthcare Providers Trust Our Denial Management Services
Based in Tempe, Arizona and serving clients across the U.S., Greenhive Billing Solutions is a go-to partner for denial recovery and revenue protection. We blend hands-on expertise with automation and personalized support.
- 95%+ denial resolution success rate
- Certified specialists in Medicare , Medicaid , and commercial plans
- Daily tracking and real-time status updates
- Transparent reporting with insights you can act on
- Fully HIPAA-compliant systems
You care for patients, we’ll protect your payments.
From Review to Resolution
Our Proven Denial Management Workflow
Our team seamlessly plugs into your medical billing system with minimal setup:
- Secure access to billing platform or EHR
- Denial review and trend analysis
- Root cause identification
- Appeal preparation and resubmission
- Prevention plan and staff feedback
- Real-time performance reporting
SERVICES
Denied Claims Are Quietly Draining Your Bottom Line
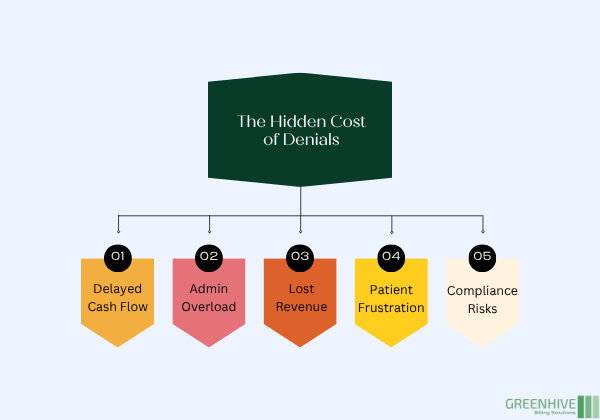
Stop Denials from Costing You
Why Denials Hurt More Than You Think
- Delayed payments and cash flow gaps
- Extra workload for admin teams
- Lost revenue on uncorrected claims
- Patient frustration over billing confusion
- Higher risk of non-compliance
With us, you stop the leak before it turns into a flood. We track, resolve, and prevent denials so your payments stay on track and your team stays focused.
Beyond Fixing Claims
What Is Denial Management and Why It Matters
Denial management isn’t just about fixing claims after they’re rejected. It’s about uncovering what caused the denial in the first place and building long-term systems that stop it from happening again.
At Greenhive Billing Solutions, our team of denial specialists goes deeper than surface-level fixes. We identify patterns, correct workflows, and keep your revenue cycle running smoothly.
- Analyzing payer responses and denial codes
- Identifying trends in medical coding, eligibility verification , and documentation
- Filing strong, timely appeals
- Fixing workflow gaps to prevent repeat denials
- Monitoring performance and catching issues early
BENEFITS
Benefits of Our Denial Management Services
Higher Recovery Rates
We fight for every denied dollar so you don’t have to write off earned revenue.
Less Admin Stress
We take the burden off your front desk and billing team with end-to-end denial handling.
Faster Resolutions
Our systems and experience lets us respond to denials fast, often within days.
Fewer Repeat Denials
We don’t just fix claims. We fix workflows and train your staff to prevent future denials.
Denials Don’t Just Delay Revenue, They Damage Your Practice
Without expert handling, denials stack up fast. Payments stall. Staff gets buried. Patients call confused. We step in with clear processes, proven tools, and a team that knows how to get results.
We Speak the Language of Payers, So You Don’t Have To
Every insurer, from Medicare to private payers, has its own maze of policies and procedures. Our team keeps up with each one, ensuring your claims comply with current rules and get paid faster.
- Denial Codes and payer policies
- Prior Authorization issues
- Coding discrepancies
- Missing or mismatched documentation
- Timely claim resubmissions and appeal deadlines
OUTCOMES
Results That Make a Difference

Let’s Turn Denials into Dollars
Why Strategic Denial Management Pays Off
ANY QUESTIONS?
Frequently Asked Questions
What makes denial management different from billing?
Can denial management really recover lost revenue?
Do you work with small or solo practices?
How quickly can denials be resolved?
How does Greenhive stay current with payer rules?