Medical Credentialing Services
Smarter Credentialing.
Stronger Revenue.
Healthcare Arizona Credentialing Services That Speed Up Onboarding
Complete Credentialing Oversight
Specialty-Focused Credentialing
Faster Approval Timelines
End-to-End Healthcare Credentialing Services for Providers in Arizona

Our Provider Credentialing Services Include:
- Mental health billing and credentialing services for psychologists, psychiatrists, and behavioral health clinics.
- Dental credentialing services for solo dentists and dental practices.
- Physician credentialing services tailored for primary care and specialists.
- Credentialing for therapists including LMFTs, LPCs, LCSWs, and counselors.
- CAQH Profile setup and maintenance
- NPI and DEA registration assistance.
- Medical license verification.
- Ongoing recredentialing and compliance management to ensure continued eligibility.
- Credentialing for physicians, therapists, dentists, and more.
- Support for individual providers, group practices, and multispecialty clinics.
Why Choose Medical Credentialing Services Arizona
Simplifying Medical Credentialing for Providers and Practices
- Payer Network Expansion
- Faster Time-to-Approval
- Error-Free Submissions
- Compliance-First Approach
- Dedicated Credentialing Specialists
What Makes Our Medical Credentialing Services Stand Out
At Greenhive, we combine expert compliance knowledge with process automation to deliver accurate, fast, and stress-free credentialing. We support providers in every U.S. state and tailor our services to your specialty, size, and organizational needs.
Comprehensive Enrollment Preparation: We prepare and manage all documents required for credentialing with Medicare, Medicaid, HMOs, PPOs, and commercial payers, ensuring fewer delays and a smooth start to your practice’s onboarding.
CAQH & Documentation Expertise: We keep your provider documents organized, accurate, and up to date, so the enrollment process moves forward without unnecessary back-and-forth or delays.
Ongoing Compliance & Monitoring: Credentialing is not a one-time task. We track expirations, manage recredentialing, and keep your information up to date to ensure your credentials stay valid and compliant.
Credentialing Powered by Smart Systems: Our secure technology platform automates much of the credentialing process, reducing manual errors and giving your team full visibility into status and timelines, without requiring costly credentialing software.
We’ll walk you through gaps, timelines, and next steps, no obligation.
Why Medical Credentialing is Essential for Your Practice
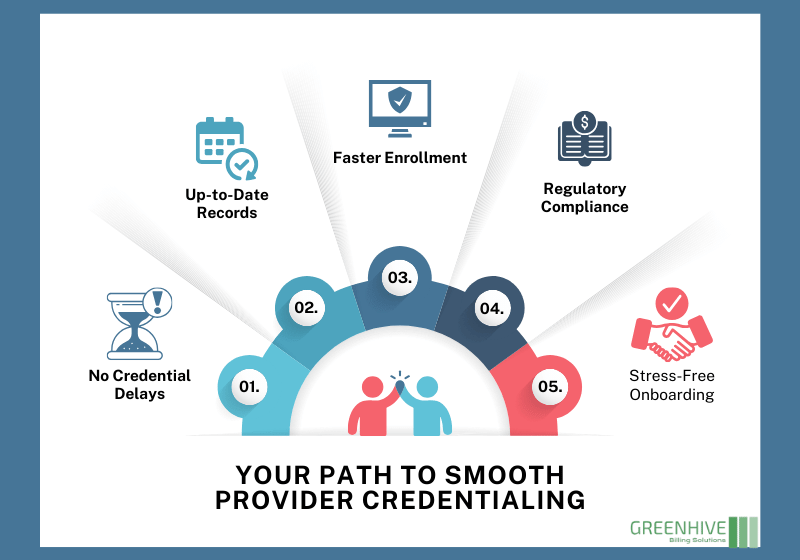
Credentialing lays the foundation for provider onboarding, hospital privileges, and payer enrollment. Our services help your practice:
- Start enrollment processes faster.
- Avoid delays due to missing or invalid credentials.
- Maintain up-to-date CAQH, NPI, and license records.
- Stay compliant with shifting regulatory requirements.
- Eliminate admin stress from onboarding to recredentialing.
Speak with a real expert who understands your specialty and credentialing needs.
Common Credentialing Challenges and How We Solve Them
From missing documentation to slow payer approvals, credentialing can quickly become a frustrating roadblock for healthcare providers. Applications often get rejected due to small errors, and keeping track of renewals or recredentialing deadlines can be overwhelming, especially for practices operating across multiple states or specialties.
Our team eliminates these issues by reviewing every detail before submission, maintaining direct follow-up with payers to speed up timelines, ensuring complete accuracy to prevent rejections, and tracking all renewal dates so nothing slips through the cracks. We make the credentialing process smooth, compliant, and fast, so you can focus on patient care instead of paperwork.
Why Outsourcing Your Credentialing Makes Life Easier
Outsourcing your credentialing isn’t just about saving time, it’s about reducing mistakes and giving your team the freedom to focus on patient care, not paperwork.
Faster Approvals
Our team prepares and submits documents with precision, so there are fewer back-and-forth delays.
Operational Efficiency
Accurate credentialing keeps your onboarding timelines on track and ensures nothing falls through the cracks.
Seamless Integration with Operations
Credentialing fits your systems, getting providers started without workflow disruptions.
Reduced Administrative Workload
We handle the entire credentialing lifecycle, so your staff can focus on patients, not provider forms.
Prevent Delays Before They Happen
When credentialing gets delayed, provider onboarding stalls, and that means lost time and missed opportunities. At Greenhive Billing Solutions, we stay on top of every regulatory update and credentialing requirement, so you never miss a deadline or renewal.
Ongoing Credentialing & Privileging Support
Credentialing doesn’t stop after the initial approval. Our team provides continuous credentialing management to help your practice stay compliant year-round. We track license renewals, certifications, recredentialing schedules, and more, so your credentials remain active and accurate.
We also support privileging for hospital-based and surgical providers, verifying qualifications needed for specific scopes of care.
Results That Speak for Themselves
Incomplete applications delay approvals, but streamlined processes speed success.

High satisfaction is common when the process is efficient, transparent, and supportive.
Take Control of Your Credentialing Today
Fast, Accurate, Compliant
We handle every step to ensure you get approved quickly, avoid costly delays, and stay compliant, so you can focus on patient care, not paperwork.
ANY QUESTIONS?
Frequently Asked Questions
What exactly does medical credentialing involve for healthcare organizations?
How long does provider credentialing take?
Credentialing typically takes between 60 to 120 days. We streamline the process by preparing all required documentation up front and submitting it promptly.
Why do healthcare organizations need both credentialing and enrollment handled properly?
Credentialing confirms a provider’s qualifications for compliance, safety, and quality standards. Enrollment takes that verified information and submits it to payers or facilities, so the provider can officially begin practicing.
If either step is delayed or done incorrectly, it can hold onboarding, impact revenue, and pose compliance risks. That’s why smart organizations treat them as two linked, but distinct, processes managed under one strategy.
Can Greenhive handle hospital credentialing and group practices?
Yes. We specialize in credentialing for hospitals, multi-provider groups, and multi-location clinics.
Do I need to recredential regularly?
Yes. Most organizations and payers require recredentialing every 2 to 3 years. We track all timelines and manage the paperwork, so your credentials stay current.
WE SUPPORT
Who We Serve
We support physicians clinics, hospitals specialty practices and healthcare networks across the USA. No matter the size of your practice our patient eligibility services are designed to fit your specific operational and financial goals.
