Healthcare billing is rapidly transforming in 2026, directly shaping the financial health of organizations across the industry. As new regulations and technologies emerge, many leaders find themselves puzzled by the differences between revenue cycle medical billing and traditional billing.
This article aims to clear up the confusion, providing a detailed look at both approaches, their unique processes, and the impact they have on operational success. You will discover clear definitions, step-by-step process breakdowns, the pros and cons of each approach, current technology trends, and real-world outcomes for healthcare organizations.
Gain clarity and confidence as you navigate the evolving billing landscape, and use this knowledge to make informed decisions that strengthen your organization’s financial future.
Defining Revenue Cycle Medical Billing and Traditional Billing
In 2026, clear understanding of revenue cycle medical billing and traditional billing is essential for healthcare organizations navigating a rapidly changing financial environment. The terms are often used interchangeably, but their differences shape how practices manage revenue, compliance, and patient experience.
Key Concepts and Terminology
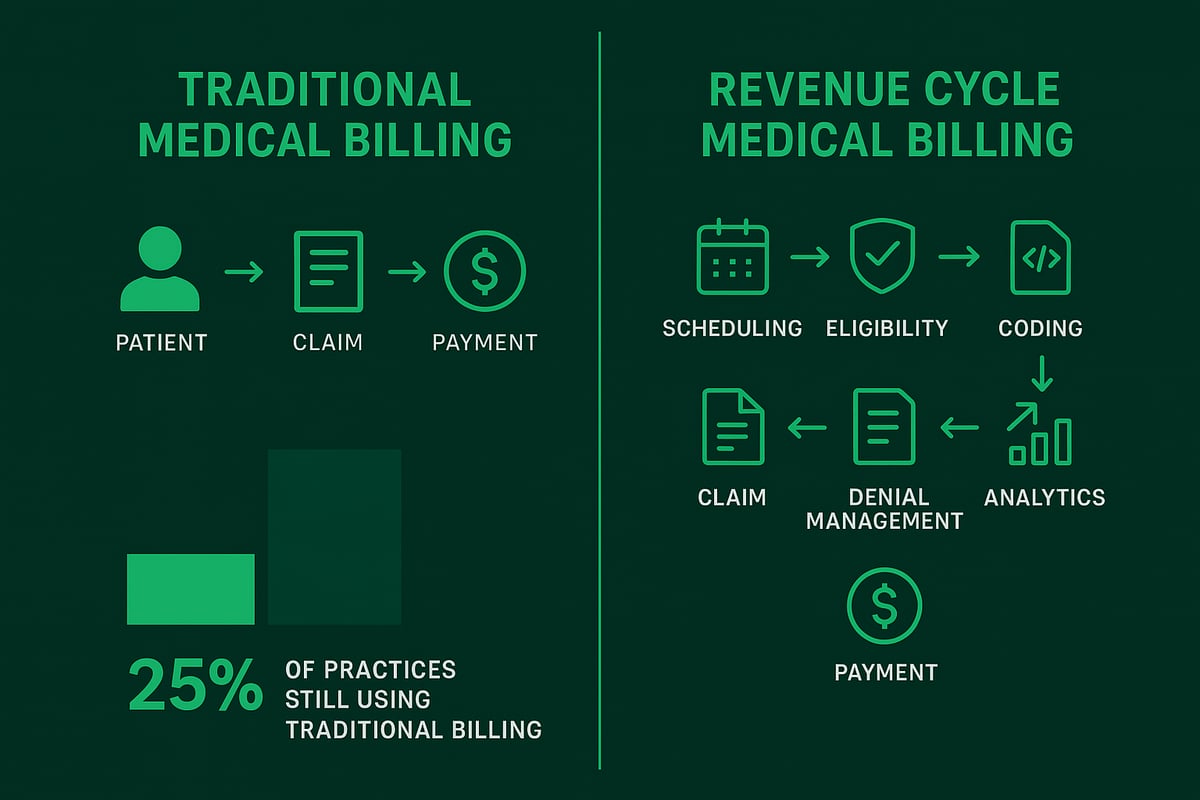
Traditional medical billing refers to the process of creating claims, submitting them to payers, posting payments, and billing patients after care is provided. This approach is transactional, focusing on steps taken after a patient’s visit. It relies heavily on manual work and often addresses issues only after they arise.
In contrast, revenue cycle medical billing is a holistic strategy. It spans the entire patient financial journey, starting from appointment scheduling and insurance verification, through clinical documentation, coding, claim submission, payment posting, denial management, and ongoing reporting. By addressing each stage proactively, revenue cycle medical billing aims to minimize denials and optimize revenue from the outset.
Many organizations confuse these terms, but in practice, their scopes are quite different. As the healthcare industry evolves, so does its terminology. In 2026, precise definitions matter more than ever, especially as analytics and compliance demands increase. Practices using only traditional billing may find themselves lagging behind those that adopt a full revenue cycle medical billing solution.
For example, a clinic relying on traditional billing submits claims after patient visits and addresses payment issues as they occur. Meanwhile, a practice using revenue cycle medical billing integrates front-end verification and real-time analytics, preventing issues before they become costly. According to industry estimates, up to 25% of practices still depend on traditional billing workflows, exposing themselves to higher denial rates and slower payments.
Understanding these distinctions is foundational for informed decision-making and financial success. To further explore how analytics support this clarity and transparency, see Healthcare Revenue Cycle Analytics.
Scope and Stakeholders
The scope of revenue cycle medical billing extends far beyond the billing department. In traditional medical billing, stakeholders typically include the billing team, coders, and finance staff, who work in silos. Communication between these groups is often limited, which can create bottlenecks and errors.
Revenue cycle medical billing, on the other hand, requires active involvement from multiple departments. Front desk staff, clinical teams, coders, billing professionals, and finance all collaborate throughout the patient journey. This cross-functional integration ensures accurate data collection and process efficiency at each step.
Consider the impact of missing insurance authorizations during scheduling. In a traditional billing model, this omission may not be discovered until after a claim is denied. In a revenue cycle medical billing environment, real-time checks at the front end prevent such costly errors, leading to smoother downstream processes.
By breaking down departmental silos and promoting collaboration, revenue cycle medical billing improves operational efficiency and financial outcomes. Practices that embrace this approach benefit from fewer denials, faster payments, and better overall performance.
The Revenue Cycle Medical Billing Process: Steps and Best Practices
Navigating the complexities of revenue cycle medical billing requires a clearly defined, end-to-end process. For healthcare organizations in 2026, an optimized workflow not only ensures regulatory compliance but also directly impacts financial performance. Understanding each step, and adopting best practices, can help drive efficiency and profitability.
End-to-End Workflow Breakdown
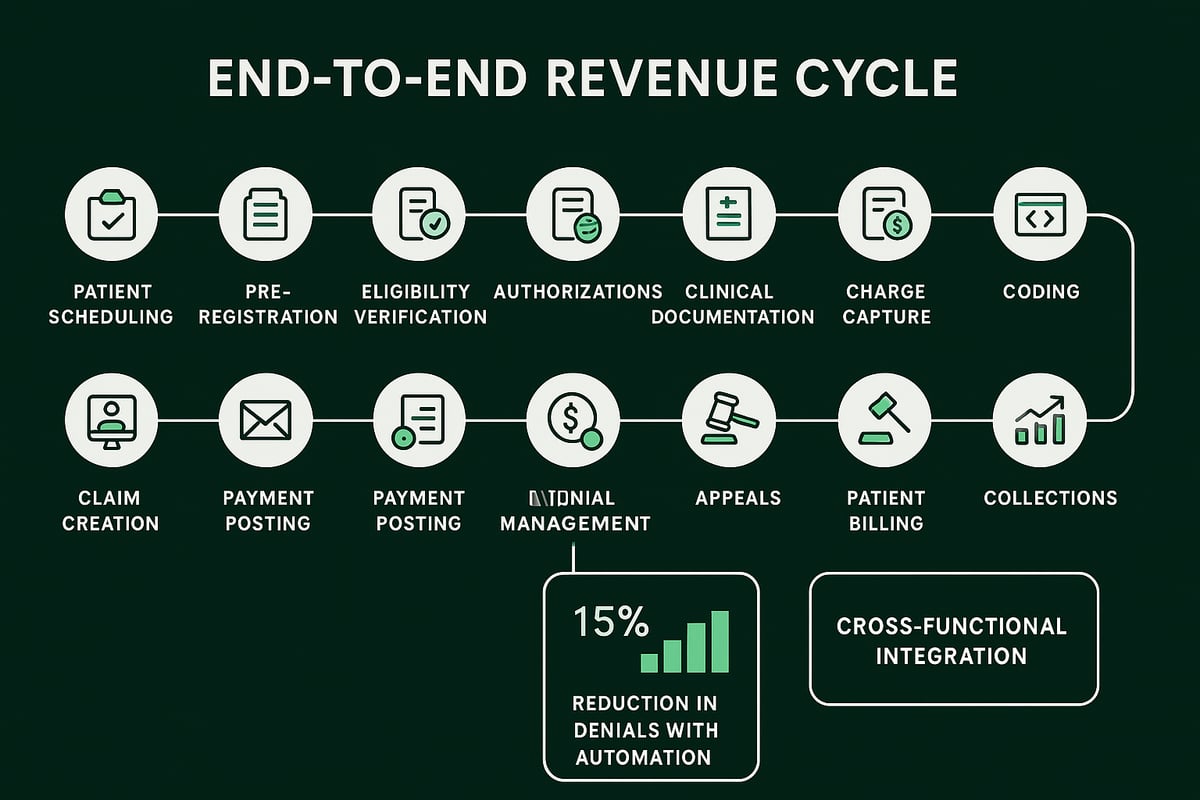
The revenue cycle medical billing process starts well before a patient enters the clinic and extends until every dollar is collected and reconciled. Each stage supports the next, forming a continuous cycle rather than a series of isolated tasks.
- Patient Scheduling and Pre-registration: Accurate demographic and insurance data are collected upfront, reducing errors later in the cycle.
- Insurance Eligibility Verification and Authorization: Automated checks confirm coverage and secure necessary approvals, preventing claim denials and delays.
- Clinical Documentation and Charge Capture: Providers document care in detail, and charges are captured in real time for transparency and compliance.
- Medical Coding and Claim Creation: Certified coders assign precise codes using ICD, CPT, and HCPCS standards. For a deeper dive into the coding stage and its impact on revenue cycle medical billing, see Medical Coding Revenue Cycle Management.
- Claim Submission and Payment Posting: Claims are transmitted electronically, payments are posted promptly, and remittances are reconciled for accuracy.
- Denial Management and Appeals: Dedicated teams track denials, identify root causes, and pursue appeals to recover revenue.
- Patient Billing and Collections: Clear, timely billing statements and payment plan options improve collection rates and patient satisfaction.
- Revenue Reporting and Analytics: Real-time dashboards provide actionable insights into cash flow, denials, and overall financial health.
By integrating these steps, revenue cycle medical billing transforms from a reactive process into a proactive strategy. Each stakeholder, from front desk to finance, plays a role in supporting the cycle. This holistic approach reduces silos, minimizes rework, and enables organizations to adapt quickly to payer changes and patient needs.
Best Practices for 2026
Adopting best practices in revenue cycle medical billing is essential for staying competitive and compliant in 2026. Automation leads the way, reducing manual errors and accelerating every phase of the cycle.
- Automation of Manual Tasks: Tasks like eligibility verification, claim scrubbing, and payment posting benefit from automation, leading to fewer errors and faster reimbursement. Practices leveraging automated eligibility verification report a 15% drop in claim denials.
- Integration with EHR/PMS Systems: Seamless data flow between clinical and financial platforms minimizes duplicate data entry and ensures consistency.
- Regular Performance Reviews and KPI Tracking: Monitoring metrics like days in A/R, denial rates, and collection percentages helps organizations target areas for improvement.
- Proactive Denial Management: Identifying trends and root causes of denials enables teams to adjust workflows upstream, reducing recurring issues.
- Transparent Communication: Clear, timely updates to both patients and staff foster trust and streamline the billing experience.
Proactive management is the hallmark of effective revenue cycle medical billing. Organizations that invest in continuous improvement, staff training, and technology integration consistently see shorter days in A/R and healthier cash flow.
Traditional Medical Billing: Approach, Challenges, and Limitations
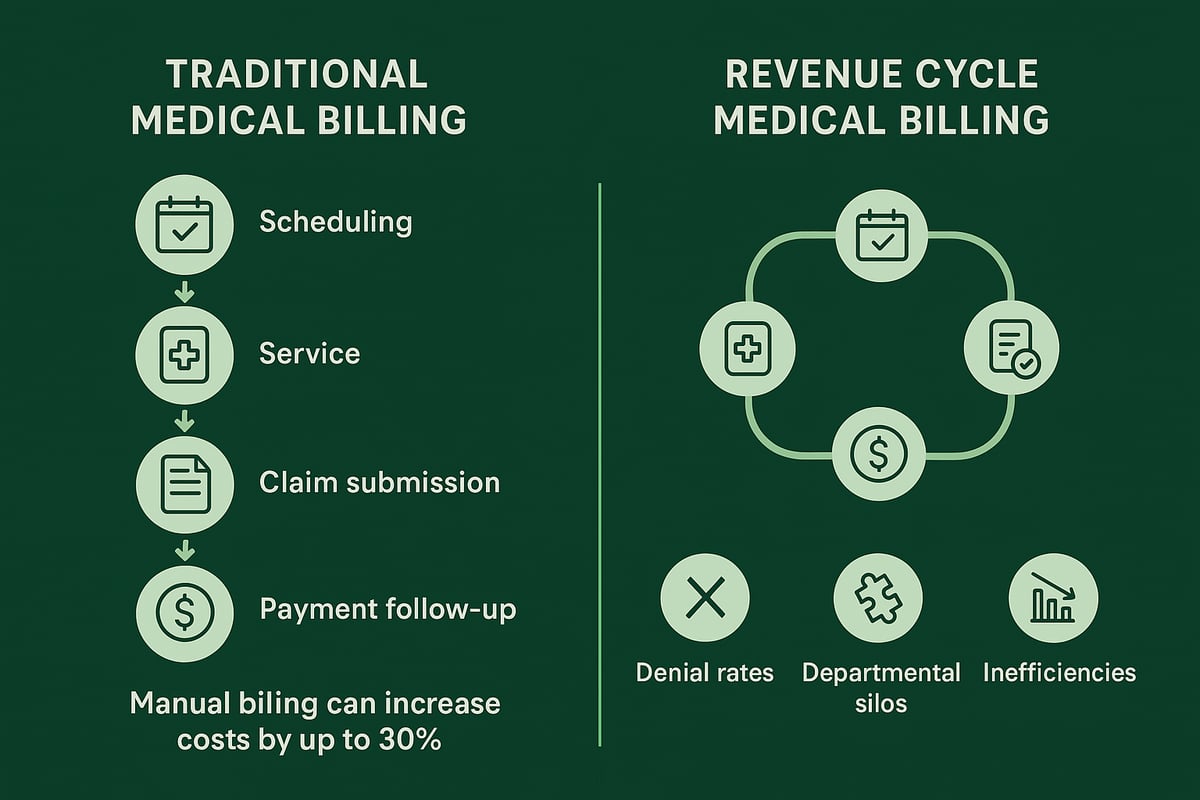
Traditional medical billing remains a common approach in many healthcare organizations, especially smaller practices. Unlike the holistic, cross-functional strategies found in revenue cycle medical billing, traditional methods focus on a narrow, transactional sequence of tasks. This often leads to missed opportunities for process improvement and financial optimization.
The Transactional Nature of Traditional Billing
At its core, traditional medical billing is a reactive process. The workflow typically begins after a patient visit is complete. Front desk staff hand off patient information to billing teams, who then create and submit claims to payers. Payment posting and patient invoicing follow, often days or weeks after care is delivered.
This approach rarely addresses upstream steps such as insurance eligibility verification or pre-authorization. As a result, issues like missing authorizations or inaccurate patient data are only discovered after the claim is denied. In contrast, revenue cycle medical billing integrates these processes from the outset, ensuring smoother financial outcomes.
For example, a billing team in a traditional setup may only realize a claim lacks necessary documentation once a denial is received. This triggers a time-consuming cycle of corrections and resubmissions. The lack of proactive intervention highlights a key difference from revenue cycle medical billing, where potential problems are identified and resolved early.
Common Challenges and Pitfalls
Traditional billing faces several recurring challenges that can undermine a practice’s financial health. High denial rates are a frequent consequence of missing or inaccurate data, since upstream verification is often overlooked. Payment delays are common due to manual entry, paper-based processes, and the absence of automation.
Operational costs can rise significantly. Industry data suggest manual billing workflows can increase expenses by up to 30 percent. Siloed communication between departments further compounds these issues, leading to repeated rework and lost productivity. Without integrated processes, each team focuses solely on its own tasks, missing opportunities for collaboration.
Perhaps most critically, denial management is largely reactive in traditional billing models. Teams spend substantial time addressing denials after they occur, rather than preventing them. To learn more about strategic approaches, visit Denial Management in Medical Billing. As healthcare organizations scale, these pitfalls become harder to manage, making revenue cycle medical billing a more sustainable option.
Impact on Practice Performance
The cumulative effect of these challenges is significant. Recurring denials and underpayments directly reduce profitability. Practices relying on traditional billing often struggle with inconsistent cash flow and limited financial transparency.
A lack of robust reporting tools makes it difficult to identify root causes of revenue leakage. For instance, repeated claim denials may stem from errors during patient registration or authorization, yet these issues persist because they are not addressed upstream. As organizations grow, the limitations of traditional billing can hinder both operational efficiency and long-term success, reinforcing the advantages of revenue cycle medical billing.
Comparative Analysis: Revenue Cycle Medical Billing vs. Traditional Billing
Understanding the differences between revenue cycle medical billing and traditional billing is critical for healthcare organizations seeking operational and financial excellence in 2026. By comparing these two approaches side by side, decision-makers can align their billing strategy with growth goals, compliance needs, and patient expectations.
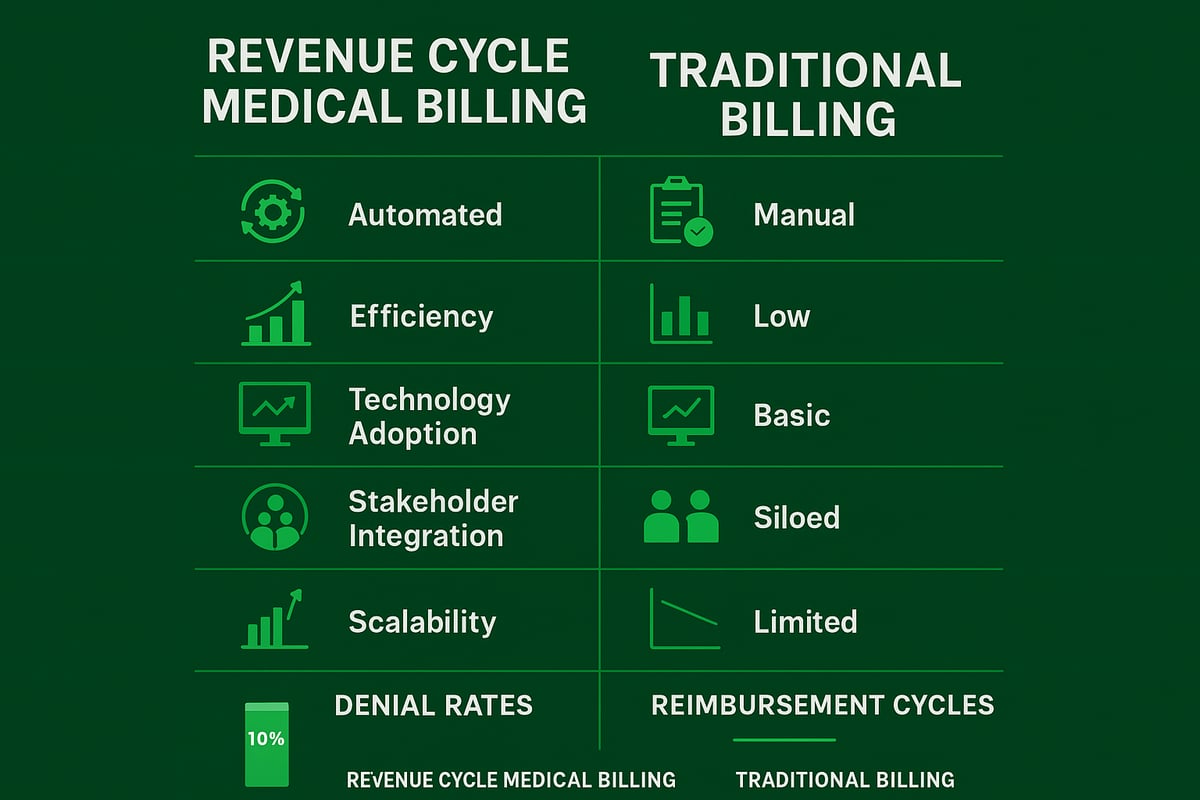
Scope and Strategic Focus
Revenue cycle medical billing offers a comprehensive, end-to-end solution, while traditional billing remains transactional and reactive. The scope of revenue cycle medical billing extends from patient scheduling through final payment, integrating every financial touchpoint. Traditional billing, in contrast, focuses mainly on claim submission after care is delivered.
Comparison Table:
| Step/Feature | Revenue Cycle Medical Billing | Traditional Billing |
|---|---|---|
| Patient Scheduling | ✔ | |
| Eligibility & Authorization | ✔ | Limited |
| Charge Capture & Coding | ✔ | ✔ |
| Claim Submission & Payment | ✔ | ✔ |
| Denial Management | ✔ | Limited |
| Patient Collections | ✔ | ✔ |
| Analytics & Reporting | ✔ | Limited |
This wider scope enables organizations using revenue cycle medical billing to proactively manage financial performance, while traditional billing often leads to missed revenue opportunities. In 2026, clarity on these scopes is vital for strategic planning and informed investments.
Operational Efficiency and Financial Outcomes
Revenue cycle medical billing consistently delivers higher operational efficiency. By integrating upstream processes like eligibility verification and authorization, it reduces claim denials and shortens days in accounts receivable. Practices that implement revenue cycle medical billing typically see up to 20% faster reimbursement cycles compared to those relying on traditional billing.
Traditional billing, with its manual workflows, is more prone to errors, delays, and increased operational costs. The lack of automation and siloed communication can lead to recurring denials and inconsistent cash flow. Healthcare organizations committed to revenue cycle medical billing benefit from streamlined operations and more predictable financial outcomes.
Stakeholder Coordination and Accountability
A key advantage of revenue cycle medical billing is its cross-functional integration. Stakeholders from front desk, coding, clinical, finance, and billing teams collaborate through shared data and unified workflows. This coordinated approach ensures accountability across the patient financial journey.
In traditional billing, departments often operate in silos. Billing teams handle claims post-service, rarely interacting with scheduling or clinical staff. This separation can cause issues such as missing authorizations or incorrect patient information, which negatively impact downstream billing and collections. Revenue cycle medical billing bridges these gaps and fosters a culture of shared responsibility.
Technology and Automation
Technology is a driving force behind the effectiveness of revenue cycle medical billing. Integrated platforms, automation, and real-time analytics reduce human error and administrative burden. For example, automated eligibility checks and denial management tools help prevent revenue leakage.
Traditional billing often depends on manual data entry and paper-based processes, which slow down reimbursement and increase the risk of costly mistakes. As highlighted in AI and Automation in Medical Billing, the adoption of AI and automation in revenue cycle medical billing enhances efficiency and accuracy, giving organizations a competitive edge in 2026.
Scalability and Adaptability
Revenue cycle medical billing is built for growth and adaptability. As healthcare organizations scale, expand services, or respond to regulatory changes, this approach supports evolving needs. The integrated workflows and analytics within revenue cycle medical billing make it easier to adjust processes and maintain compliance.
Traditional billing struggles to keep pace with increasing payer complexity and patient financial responsibility. Its limited scope and lack of adaptability can hinder expansion and expose organizations to compliance risks. For any practice planning for the future, revenue cycle medical billing offers a foundation for sustainable success.
Technology Trends Shaping Medical Billing and RCM in 2026
The landscape of revenue cycle medical billing is evolving rapidly as technology reshapes every aspect of healthcare finance. In 2026, practices and organizations are embracing digital tools to streamline workflows, reduce errors, and improve financial outcomes. Understanding these trends is essential for maintaining a competitive edge and optimizing your billing operations.
Automation and Artificial Intelligence
Automation and AI are transforming revenue cycle medical billing by eliminating repetitive manual tasks and minimizing human error. AI-driven eligibility checks, coding assistance, and denial prediction tools are now standard, allowing billing teams to focus on complex cases rather than routine data entry.
Practices leveraging automation see faster reimbursement cycles and fewer claim denials. For example, automated eligibility verification can reduce denials by up to 15 percent, directly impacting the bottom line. As a result, organizations adopting these solutions experience improved cash flow and operational efficiency.
Integration with EHR and Practice Management Systems
Seamless integration between revenue cycle medical billing processes and EHR or practice management systems is a major trend. Real-time data exchange ensures accurate patient information, eligibility status, and charge capture, all without manual re-entry.
This level of integration supports coordinated workflows and reduces the risk of billing errors. For a deeper look at how these systems are shaping the future, see EHR and Medical Billing Trends 2026, which explores user experience and analytics advancements.
Data Analytics and Financial Transparency
Data analytics tools are central to modern revenue cycle medical billing. Dashboards offer real-time visibility into key performance indicators such as denial rates, days in accounts receivable, and collection efficiency.
Predictive analytics now help practices forecast cash flow and identify problem areas before they impact revenue. This transparency enables proactive decision-making and supports continuous improvement across the organization.
Regulatory Compliance and Security
Compliance and data security remain top priorities as regulations evolve. Automated audit trails and secure data transmission are now expected features of any robust revenue cycle medical billing service.
Emerging technologies like blockchain and AI are enhancing data security and privacy. For organizations interested in the technical side, the Integration of Blockchain and AI in Healthcare provides insights into how these innovations are protecting sensitive financial and patient information.
Industry Adoption Rates
By 2026, over 70 percent of mid-sized healthcare practices are projected to use integrated RCM platforms. This widespread adoption reflects a shift toward smarter, more connected, and secure revenue cycle medical billing processes.
Organizations that embrace these trends will be better positioned to adapt to payer complexity, regulatory change, and evolving patient expectations.
Practical Outcomes: How the Right Approach Impacts Healthcare Organizations
Healthcare organizations in 2026 face unprecedented financial and operational pressures. The choice between traditional billing and revenue cycle medical billing directly shapes their success. Understanding the practical outcomes of each approach empowers decision-makers to drive profitability, enhance patient trust, and future-proof their business.
Financial Health and Revenue Optimization
Revenue cycle medical billing is designed to maximize reimbursement and reduce revenue leakage. By managing every step of the revenue process, from eligibility verification to payment posting, practices can capture more of what they earn and reduce costly write-offs.
Organizations that prioritize accurate coding, timely claim submission, and proactive denial management see measurable improvements in cash flow. For instance, understanding what are revenue codes in medical billing ensures claims are paid correctly the first time, reducing rework and underpayments.
In contrast, traditional billing often leaves money on the table due to missed charges and delayed follow-up.
Patient Experience and Satisfaction
Revenue cycle medical billing directly impacts how patients feel about their healthcare provider. With RCM, patients benefit from clear, upfront communication about costs, faster claim resolution, and flexible payment options.
Transparency in the billing process builds trust and reduces confusion. Patients are more likely to pay their bills promptly when they understand their financial responsibility and have access to convenient payment portals.
Traditional billing, with its reactive nature, can lead to surprise bills, frustration, and decreased patient loyalty.
Staff Productivity and Morale
Revenue cycle medical billing streamlines workflows and reduces manual tasks for administrative and clinical staff. Automation eliminates repetitive data entry, allowing teams to focus on higher-value work.
RCM service providers also offer cross-functional training and clear accountability, fostering a collaborative culture. This reduces burnout and increases job satisfaction across departments.
In a traditional billing environment, staff often face bottlenecks, rework, and siloed communication, which can erode morale and slow down operations.
Risk Management and Compliance
Revenue cycle medical billing proactively addresses regulatory and payer requirements. With built-in compliance checks, audit trails, and up-to-date coding standards, organizations lower their risk of costly penalties and audits.
Regular monitoring ensures billing practices stay aligned with HIPAA and other regulations. By contrast, traditional billing methods may miss critical compliance steps, exposing practices to financial and reputational risk.
A strong RCM framework means organizations are always prepared for regulatory changes and payer audits.
Case Example
Consider two similar-sized practices: one using traditional billing, the other embracing revenue cycle medical billing. The RCM-enabled practice saw denial rates drop by 18 percent, days in accounts receivable reduced by 25 percent, and patient satisfaction scores rise significantly.
Staff reported fewer administrative headaches and more time for patient care. Leadership noted improved financial visibility and easier adaptation to new payer rules. According to the medical billing outsourcing market overview, practices that invest in RCM services are better positioned to scale and remain competitive in a rapidly changing environment.
Making the shift to revenue cycle medical billing delivers tangible, strategic results for healthcare organizations.
If you’re weighing the benefits of revenue cycle medical billing versus traditional billing, you’re not alone—many healthcare leaders are looking for clarity as 2026 approaches. We’ve explored how the right approach can streamline workflows, improve cash flow, and support your team’s productivity. If you’re ready to see how these insights apply to your own practice or want expert guidance tailored to your needs, let’s take the next step together. You can Book Your Free Consultation to discover opportunities for growth, efficiency, and peace of mind in your billing processes.