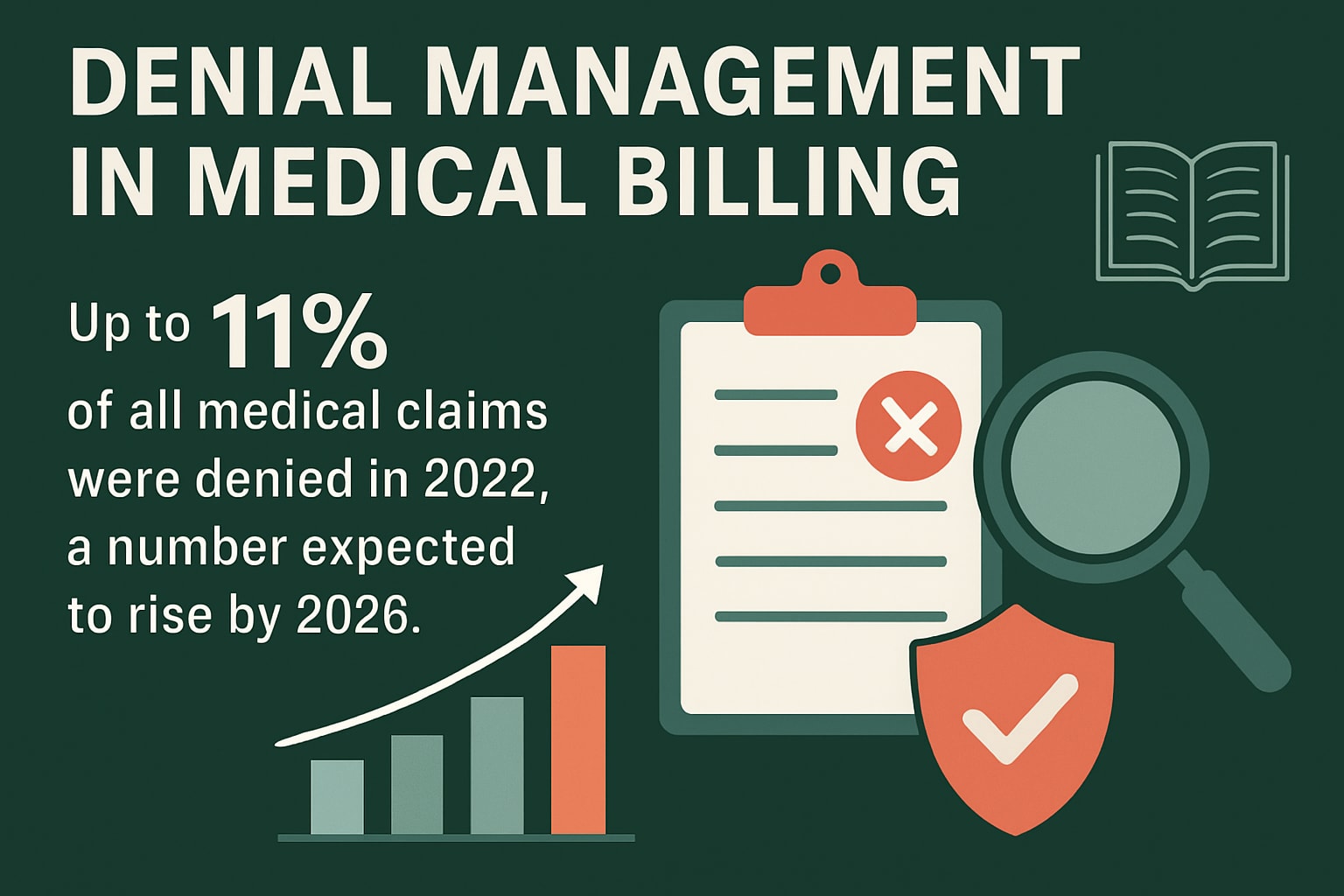
Up to 11% of all medical claims were denied in 2022, and this trend is projected to accelerate by 2026. For healthcare organizations, claim denials directly impact revenue and can disrupt cash flow.
Effective denial management in medical billing is now essential for sustainable growth. This guide offers a comprehensive roadmap tailored for 2026, covering definitions, denial types, a step-by-step process, best practices, technology solutions, and future trends. Discover actionable strategies to reduce denials and protect your revenue—now is the time to strengthen your approach.
Understanding Denial Management in Medical Billing
Denial management in medical billing is a strategic pillar for any healthcare organization aiming to safeguard revenue in an evolving reimbursement landscape. As claim requirements and payer guidelines shift, an adaptable approach is essential to minimize lost income and maintain operational efficiency. This section unpacks what denial management means, why it is critical in 2026, who drives the process, and what industry benchmarks reveal about today’s challenges.
What Is Denial Management?
Denial management in medical billing is the systematic process of identifying, addressing, and ultimately preventing claim denials throughout the revenue cycle. This ongoing cycle ensures claims are thoroughly reviewed, errors are corrected, and patterns are analyzed for future prevention. The process spans from front-end registration to back-end collections, making it a cornerstone of comprehensive revenue cycle management. As payer requirements evolve, denial management in medical billing must remain dynamic, with continuous updates to protocols and workflows to keep pace with regulatory and industry changes.
Why Denial Management Matters in 2026
Denial management in medical billing directly impacts the financial health of healthcare organizations. Denials can quickly erode revenue, disrupt cash flow, and inflate operational costs if not managed proactively. Over the past five years, industry data shows a 20% surge in denials, mainly due to increasingly complex payer rules and shifting reimbursement models. In 2026, organizations must prioritize denial management in medical billing to maintain profitability and reduce the administrative burden. Proactive strategies, such as advanced analytics and targeted staff training, are more important than ever for sustainable financial performance.
Key Stakeholders and Their Roles
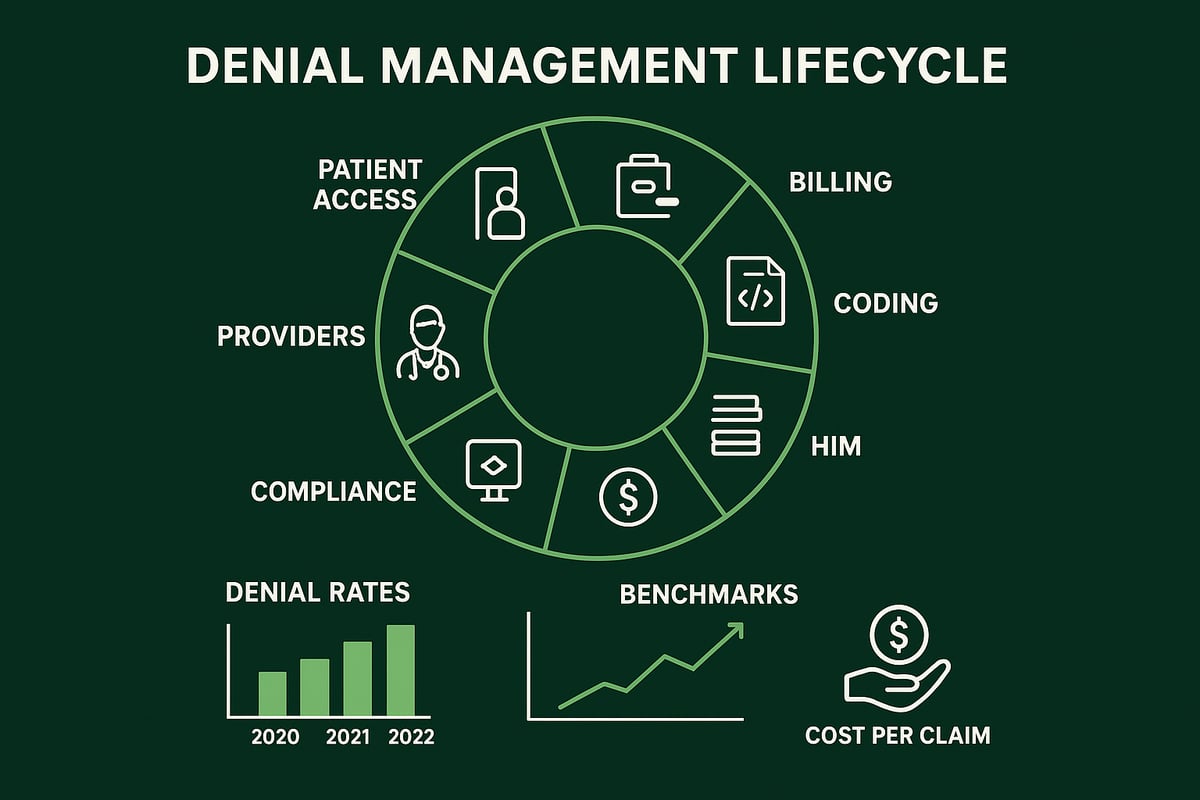
Effective denial management in medical billing requires cross-departmental coordination. Patient access teams capture initial data, billing and coding specialists ensure claim accuracy, HIM oversees documentation, and finance monitors payment outcomes. Compliance and IT departments support regulatory adherence and system integration, while providers supply clinical input. Collaboration across these teams is crucial. For example, an error during patient registration can cascade into a denial, highlighting the importance of seamless communication and shared accountability throughout the denial management in medical billing process.
Common Denial Statistics and Industry Benchmarks
Recent statistics reveal that some payers deny up to 17% of in-network claims, underscoring the scale of the challenge. The average cost to rework a denied claim is $25 for ambulatory settings and $118 for hospitals. Industry benchmarks suggest best-in-class denial rates should remain below 5%, although many organizations report higher figures. For a comprehensive look at current trends and performance standards, the 2024 Revenue Cycle Denials Index offers valuable industry insights. These benchmarks are vital for evaluating and refining denial management in medical billing strategies as we approach 2026.
Types and Causes of Claim Denials
Understanding the many types and causes of claim denials is critical for effective denial management in medical billing. As payer rules become more complex, healthcare organizations must identify, analyze, and prevent denials to protect revenue and maintain operational efficiency.
Classification of Denials
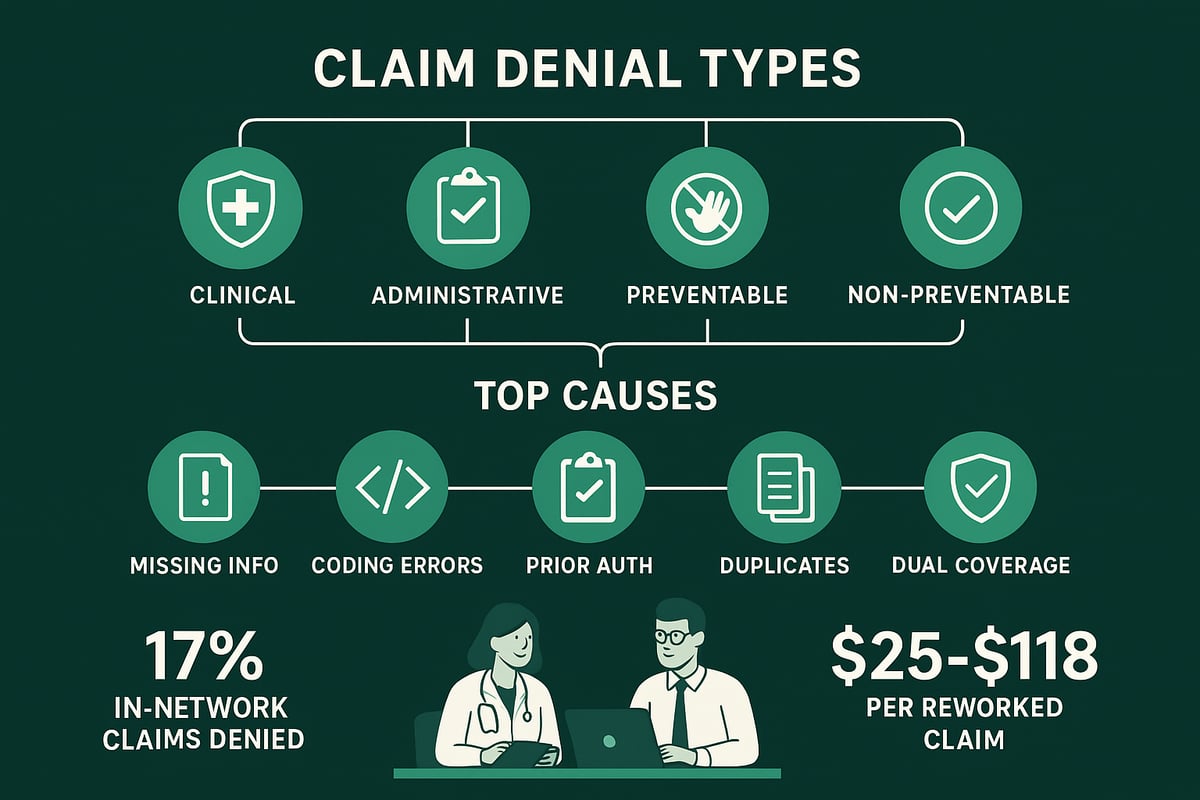
In denial management in medical billing, denials are typically classified as either clinical or administrative/technical. Clinical denials arise from issues like lack of medical necessity or insufficient documentation. Administrative or technical denials stem from errors such as missing patient details or incorrect insurance information.
Another important distinction is between preventable and non-preventable denials. Preventable denials result from errors that could have been avoided, like a missing date of birth. Non-preventable denials may be due to payer policy changes or rare scenarios outside the provider’s control.
| Denial Type | Example | Preventable? |
|---|---|---|
| Clinical | Medical necessity denied | Sometimes |
| Administrative | Missing patient info | Yes |
Effective denial management in medical billing hinges on understanding these categories and targeting preventable denials first.
Most Common Denial Reasons in 2026
The most frequent causes of claim denials in 2026 include missing or incorrect patient information, such as date of birth or insurance ID. Billing and coding errors, like incorrect CPT or ICD-10 codes, also remain a leading source of denials. Lack of prior authorization, duplicate claim submissions, and dual insurance coverage issues are persistent challenges.
For example, if prior authorization is not secured before a procedure, claims are often rejected. For a deeper dive, see Prior Authorization Services Explained.
Maintaining robust denial management in medical billing processes helps organizations stay ahead of these recurring problems and reduce revenue leakage.
Root Cause Analysis
Root cause analysis is essential for successful denial management in medical billing. By tracking denial codes and identifying patterns, organizations can pinpoint where breakdowns occur most frequently. Analytics tools allow teams to drill down into denials by payer, procedure, or department.
For instance, a spike in denials for a particular service may signal recent changes in payer policies or gaps in staff training. Post-pandemic shifts have also led to new denial trends, making it vital to review denial data regularly.
Organizations that prioritize root cause analysis can prevent future denials and foster a culture of continuous improvement in denial management in medical billing.
Impact of Denials on Healthcare Organizations
Claim denials have a measurable impact on healthcare organizations. Lost revenue, increased administrative workload, and delayed payments are direct consequences. Each denied claim costs an average of $25 to rework in ambulatory settings and $118 in hospitals.
Downstream effects include higher write-offs and patient dissatisfaction, as unresolved denials can lead to unexpected bills or delayed care. Up to 35 percent of hospital executives report denial rates nearing 10 percent, highlighting the urgency for robust denial management in medical billing strategies.
Reducing denial rates is not only about financial recovery but also about sustaining trust and operational stability.
Step-by-Step Denial Management Process
An effective denial management in medical billing process is essential for healthcare organizations aiming to reduce lost revenue, streamline workflows, and ensure sustainable growth. Below, we outline six actionable steps, each designed to address the most common pain points and empower your team to take control of denials.

Step 1: Prevention and Front-End Accuracy
The first step in denial management in medical billing focuses on preventing errors before they happen. Accurate patient registration and insurance verification are critical. Even a single typo in a date of birth or insurance ID can trigger downstream denials.
- Use eligibility verification tools to confirm patient coverage in real time.
- Train staff on the importance of precise data entry and validation.
- Automate data validation processes to catch common mistakes early.
For example, automated checks can flag outdated insurance details, reducing preventable denials. By investing in front-end accuracy, organizations lay a solid foundation for the entire denial management in medical billing process.
Step 2: Claims Submission and Coding Compliance
Proper claims submission is the backbone of denial management in medical billing. Ensuring that every claim is coded accurately using ICD-10, CPT, or HCPCS codes helps prevent administrative and clinical denials.
- Employ certified coders and provide ongoing training.
- Schedule regular code audits to catch discrepancies.
- Implement double-check protocols for high-value or complex claims.
For instance, coding for age-appropriate procedures helps avoid mismatches that can lead to denials. This proactive approach strengthens compliance and reduces costly rework related to denial management in medical billing.
Step 3: Monitoring and Tracking Denials
Continuous monitoring is a cornerstone of denial management in medical billing. Real-time tracking systems, dashboards, and analytics tools allow organizations to spot patterns and intervene quickly.
- Set up denial dashboards for instant visibility into claim status.
- Track denial rates by payer, procedure, and department.
- Use analytics to identify trends and prioritize corrective action.
For example, a sudden increase in denials from a specific payer can be flagged immediately. This enables teams to adapt quickly, minimizing revenue loss and refining the overall denial management in medical billing strategy.
Step 4: Denial Analysis and Root Cause Identification
Understanding why denials occur is essential for long-term success in denial management in medical billing. Categorizing denials by type and frequency helps organizations focus on high-impact issues.
- Leverage denial management software or conduct manual reviews.
- Group denials by common causes, such as missing prior authorizations.
- Share findings with all relevant departments for collaborative solutions.
For example, recurring denials due to missing authorizations may indicate a need for improved communication between clinical and billing teams. By targeting root causes, organizations can significantly reduce future denials and improve their denial management in medical billing outcomes.
Step 5: Appeals and Resolution Workflow
A structured appeals process is vital for effective denial management in medical billing. Timely follow-up and standardized templates ensure denials are addressed swiftly and professionally.
- Develop standardized appeal letters and documentation checklists.
- Assign clear responsibility for appeals to specific team members.
- Set internal deadlines (such as one week) for resolution.
For instance, successful appeals for medical necessity denials often rely on detailed clinical documentation and well-crafted arguments. By refining appeals workflows, organizations boost their success rate and optimize their denial management in medical billing process.
Step 6: Feedback and Continuous Improvement
The final step in denial management in medical billing is establishing a culture of continuous improvement. Feedback loops, regular audits, and cross-departmental reviews drive sustained progress.
- Hold quarterly meetings to review denial statistics and trends.
- Update training programs and workflows based on recent findings.
- Regularly audit performance to identify and address lingering issues.
Engaging a professional partner can streamline this process. For a comprehensive overview of how expert support enhances every step, see our Denial Management Services Overview. Ongoing adaptation ensures your denial management in medical billing strategy remains effective as payer rules and industry standards evolve.
Best Practices for Denial Management in 2026
Healthcare organizations in 2026 face mounting challenges with denial management in medical billing. Adopting proven best practices is essential to protect revenue, boost efficiency, and minimize preventable losses.
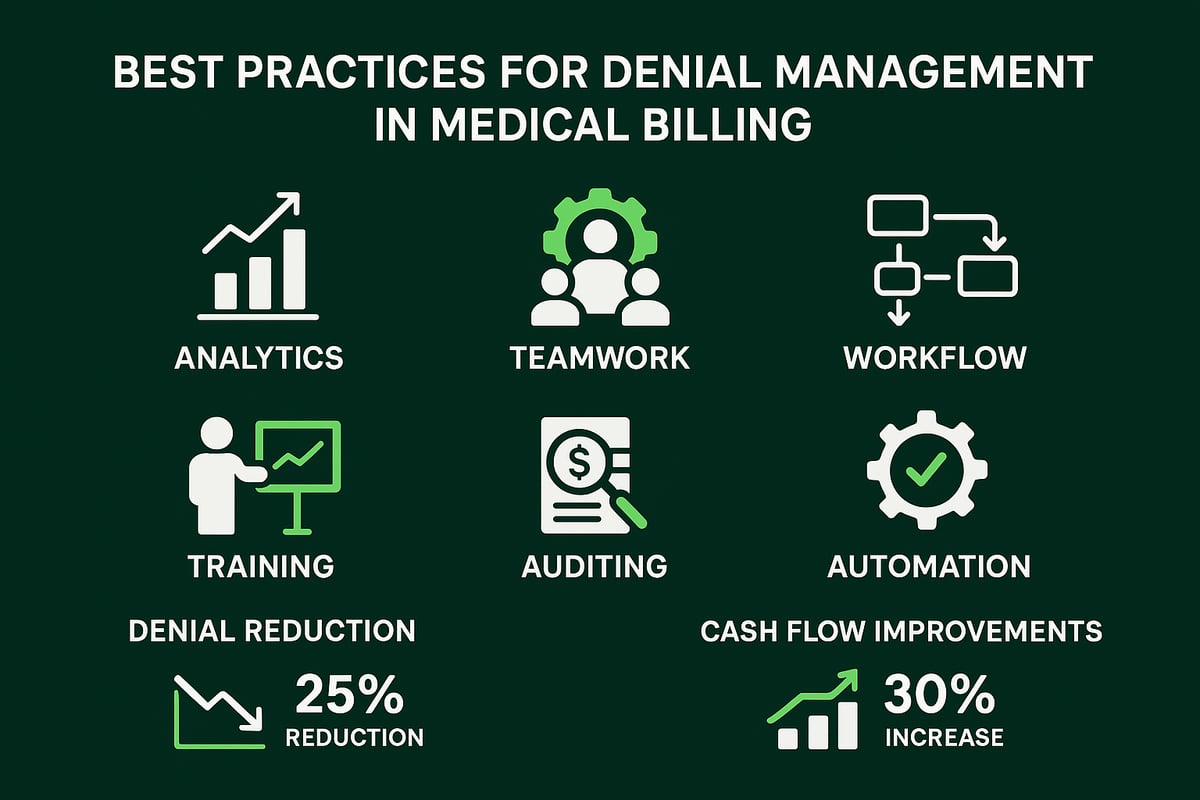
Data-Driven Decision Making
Success with denial management in medical billing starts with data-driven decision making. Organizations must capture, analyze, and act on denial trends using advanced reporting tools. Setting clear KPIs for denial rates and resolution times transforms raw data into actionable insights.
For example, predictive analytics can identify high-risk claims before submission, allowing teams to intervene early. By reviewing denial patterns, B2B healthcare providers can allocate resources more effectively and improve cash flow. To see how analytics directly impact revenue, read How Denial Management Improves Cash Flow.
Regularly updating benchmarks ensures organizations stay ahead of industry changes and payer expectations.
Cross-Departmental Collaboration
A collaborative approach is critical for effective denial management in medical billing. Patient access, health information management, billing, coding, and clinical teams must work in sync. Open communication and joint problem-solving reduce silos and enable faster resolution.
Regular cross-functional meetings help pinpoint process gaps and share best practices. For instance, if registration errors are causing denials, involving patient access staff in analysis ensures targeted improvements. Role-based training and shared accountability foster a culture of ownership.
Building a unified team effort leads to fewer preventable denials and a stronger revenue cycle.
Timely and Organized Denial Follow-Up
Timeliness is everything in denial management in medical billing. Establishing clear workflows for denial follow-up prevents claims from falling through the cracks. Automated tracking systems and reminders help staff prioritize urgent appeals and submissions.
A sample workflow table:
| Step | Owner | Timeline |
|---|---|---|
| Review denial | Billing | 1 business day |
| Prepare appeal | Compliance | 2 business days |
| Submit appeal | Billing | 1 business day |
| Monitor status | Team Lead | Ongoing |
Consistent follow-up reduces days in accounts receivable and maximizes recovery rates. Prioritizing denied claims ensures that revenue is not lost due to missed deadlines or disorganization.
Staff Training and Education
Continuous staff training is at the heart of denial management in medical billing. Payer requirements, coding standards, and compliance rules are always evolving. Providing regular education sessions and resources empowers teams to prevent errors before they happen.
Annual workshops on common denial scenarios, coding updates, and payer policy changes keep staff current. Training should also include hands-on use of analytics and denial management platforms. Investing in education leads to fewer mistakes and greater confidence.
Well-trained teams adapt quickly to industry changes, protecting organizational revenue and reputation.
Regular Audits and Quality Assurance
Routine audits are essential for strong denial management in medical billing. By systematically reviewing claims, remittance advice, and registration data, organizations can spot and correct recurring issues. Quality assurance processes help maintain high standards and minimize compliance risks.
Quarterly reviews of zero-payment claims and write-offs highlight areas needing attention. Audits also provide feedback for process improvement and staff coaching. Maintaining a schedule for internal audits ensures nothing is overlooked.
Proactive auditing supports a continuous improvement culture and reduces the likelihood of costly denials.
Leveraging Automation and Technology
Embracing automation is transforming denial management in medical billing. Industry-standard tools and robotic process automation streamline repetitive tasks like eligibility checks, claim status updates, and denial categorization.
Automated alerts and dashboards give teams real-time visibility into denial trends and workflow bottlenecks. This enables faster response times and improved accuracy. As a B2B service provider, we integrate seamlessly with client-owned platforms, adapting to your existing systems for optimal results.
Using technology strategically reduces manual workload, increases efficiency, and enhances denial prevention across the revenue cycle.
The Role of Technology and Automation in Denial Management
Technology is rapidly transforming denial management in medical billing. Modern tools offer new ways to prevent, identify, and resolve denials, helping healthcare organizations protect revenue and streamline workflows. In 2026, adopting advanced technology and automation is essential for staying competitive and compliant.
Emerging Technologies in 2026
Artificial intelligence, machine learning, and robotic process automation are revolutionizing denial management in medical billing. Predictive analytics can now identify claims at high risk of denial before they are submitted, allowing providers to take action proactively. AI-powered tools review claims data, flag missing information, and recommend corrections, improving first-pass rates. According to Healthcare Denial Trends 2025, the use of AI agents is expected to further reduce manual intervention and speed up denial resolution. By integrating these technologies, RCM service providers deliver measurable improvements in denial prevention and operational efficiency.
Integration with EHR and Practice Management Systems
Seamless integration between EHR, billing, and practice management platforms is crucial for effective denial management in medical billing. Our teams work with client-owned systems, adapting to unique workflows while ensuring data flows smoothly across platforms. Automated data capture from EHRs reduces manual entry errors and ensures that claims are accurate and complete before submission. This results in fewer denials and less time spent on rework. Close collaboration with IT departments and vendors guarantees that integration efforts align with client requirements and industry standards, supporting long-term success.
Real-Time Reporting and Analytics
Real-time dashboards and analytics are now standard in denial management in medical billing. These tools provide instant visibility into denial trends, resolution times, and payer performance. Customizable reports can be tailored for billing, finance, or compliance teams, supporting data-driven decisions. Automated alerts notify teams of spikes in specific denial types, enabling rapid response. For a deeper dive into reporting tools and their impact, visit Reporting and Analytics in Medical Billing. Leveraging these capabilities, organizations can benchmark performance and target areas for improvement.
Security, Compliance, and HIPAA Considerations
With increased automation, maintaining security and compliance is non-negotiable for denial management in medical billing. All processes must be HIPAA-compliant, with robust data encryption, access controls, and audit trails in place. Our teams prioritize secure workflows, especially when handling sensitive patient data or working with outsourced denial management services. Regular audits and compliance checks ensure that all activities meet regulatory requirements and client expectations. A strong focus on security not only protects data but also builds trust with healthcare partners.
Future Trends and Strategic Recommendations for Denial Management
Healthcare organizations face a rapidly shifting environment as we approach 2026. To maximize revenue and minimize risk, prioritizing effective denial management in medical billing is essential. Strategic planning, technology adoption, and a commitment to continuous improvement will set leaders apart in the evolving landscape.
Anticipated Regulatory Changes and Payer Policies
Regulatory requirements for denial management in medical billing continue to evolve. CMS and commercial payers regularly update guidelines for documentation, coding, and prior authorizations. New mandates, such as expanded telehealth billing rules or stricter prior authorization protocols, are becoming more common.
Staying ahead of these changes is critical. Organizations must monitor payer bulletins, adapt workflows, and educate staff on updated standards. For example, new rules may require more detailed clinical documentation or unique codes for virtual care. Reviewing industry data, such as ACA Insurers’ Claim Denial Rates, helps benchmark performance and identify trends in denial management in medical billing.
The Growing Importance of Outsourced Denial Management Services
Outsourcing denial management in medical billing is gaining traction among healthcare providers. Specialized revenue cycle management partners deliver expertise, scalability, and cost efficiency, especially for small and mid-sized organizations.
Certified professionals can handle complex appeals, root cause analysis, and ongoing process improvement. Outsourcing also allows internal teams to focus on patient care while experts address denials and compliance. Many organizations report lower denial rates, faster resolutions, and fewer write-offs after partnering with dedicated denial management service providers.
Focus on Patient Experience and Transparency
Patient expectations around billing clarity and communication are rising. Effective denial management in medical billing now extends beyond revenue recovery to include proactive patient engagement. Clear explanations, upfront financial clearance, and timely notifications about claim denials help build trust and satisfaction.
Patient portals and digital messaging tools offer transparency and empower patients to resolve issues quickly. When patients understand their benefits and the status of their claims, they are less likely to be frustrated by denials. This focus on transparency not only improves collections but also strengthens provider-patient relationships.
Continuous Improvement and Adaptation
The most successful organizations treat denial management in medical billing as a dynamic, ongoing process. Regular audits, staff training, and workflow updates are essential for staying ahead. Agile teams review denial trends, update policies, and implement new strategies to address emerging challenges.
Leveraging best practices and industry benchmarks, such as those outlined in Denial Management Best Practices, supports continuous improvement. By fostering a culture of adaptation and data-driven decision-making, healthcare providers can proactively minimize denials and optimize revenue.
As you consider the rising denial rates and the increasing complexity of payer requirements, it’s clear that proactive denial management is more important than ever. You don’t have to navigate these challenges alone—our team at Greenhive Billing Solutions is dedicated to helping healthcare providers like you improve financial performance and streamline revenue cycle operations. If you’re looking to secure maximum reimbursements and ensure long-term success for your practice, let’s take the next step together.
Book Your Free Consultation
and find out how we can tailor our solutions to your unique needs.