After five years in revenue cycle management, I see the same confusion repeatedly. Providers know medical coding matters but struggle with different systems. You receive claim denials because of coding errors. Your reimbursements suffer from incomplete documentation. Let me walk you through the coding landscape I navigate daily.
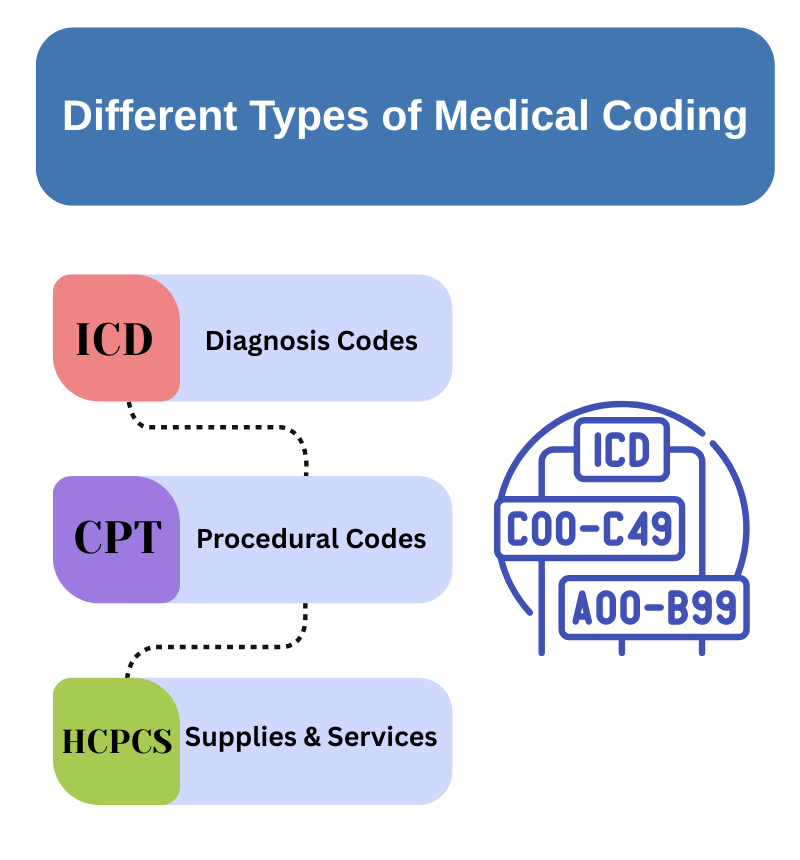
The Reality of Different Types of Medical Coding Systems
You deal with several coding systems because healthcare spans different needs. I work with practices that bill everything from simple office visits to complex surgical procedures. Each situation requires specific codes.
Think about your typical day. You diagnose conditions, perform procedures, order lab tests, and prescribe medications. Each action needs different coding systems. This specialization prevents billing errors and ensures proper reimbursement.
Here’s what I tell my clients: master the basics first, then navigate complexity. You need foundation knowledge before tackling advanced coding scenarios.
ICD Coding: Your Diagnostic Foundation
International Classification of Diseases codes form your diagnostic backbone. I help practices transition from vague documentation to precise coding every week.
ICD-10-CM drives your outpatient billing success. This system contains over 68,000 codes for specific conditions. You transform “patient has back pain” into “M54.5 – low back pain.” This specificity prevents denials and supports medical necessity.
I recently worked with a family practice losing $15,000 monthly to ICD coding errors. We fixed their documentation process. Their clean claim rate jumped from 78% to 94% in three months.
ICD-10-PCS handles inpatient procedures exclusively. Each seven-character code tells a complete story. Character position matters. You specify surgical approach, body system, and technique. This detail supports appropriate DRG assignment and payment.
ICD-11 arrives gradually across healthcare systems. I monitor implementation schedules for my clients. You should prepare for eventual transition while focusing on current ICD-10 mastery.
CPT Coding: Capturing Your Work
Current Procedural Terminology codes represent your professional services. I see practices lose money by under-coding their actual work.
Category I codes generate most of your revenue. These five-digit codes organize by specialty:
- Evaluation and Management: 99202-99499
- Surgery: 10021-69990
- Radiology: 70010-79999
- Pathology and Laboratory: 80047-89398
- Anesthesia: 00100-01999
- Medicine: 90281-99607
You choose codes that reflect the services actually provided. I audit coding accuracy monthly with my clients. Under-coding costs practices 8-12% of potential revenue annually.
Category II codes track quality metrics without payment impact. You use these for MIPS reporting and value-based contracts. Smart practices leverage these codes for quality bonuses.
Category III codes cover emerging procedures. You report experimental treatments while awaiting permanent code assignment. These codes prevent claim rejections for new technologies.
HCPCS: Filling Coverage Gaps
Healthcare Common Procedure Coding System handles items beyond CPT scope. I help practices navigate HCPCS requirements for Medicare compliance.
Level II codes use one letter plus four numbers. You need these for durable medical equipment, prosthetics, and ambulance services. Medicare requires specific HCPCS codes for covered supplies.
Example from last week: A practice billed wheelchairs with incorrect codes. Medicare denied $8,000 in claims. We corrected their HCPCS coding and resubmitted successfully.
DRG Impact on Your Documentation
Diagnosis-Related Groups affect hospital-based providers differently than office-based practices. Your coding choices influence DRG assignment and hospital payments.
I train hospital physicians on documentation impact. Complete coding prevents DRG downgrades costing hospitals thousands per case. Your detailed notes support appropriate payment levels.
Specialized Systems You Encounter
SNOMED CT enhances electronic health record documentation. This system captures clinical detail supporting care coordination. You benefit from standardized terminology across healthcare systems.
LOINC codes standardize laboratory reporting. Your lab orders and results use consistent identifiers. This standardization improves result interpretation and tracking.
NDC codes identify medications precisely. You document specific drugs, strengths, and package sizes. Accurate NDC coding supports pharmaceutical billing and safety monitoring.
What I Recommend for Implementation
Start with documentation improvement at the point of care. I implement workflows capturing coding requirements during patient encounters. Your staff learns connections between clinical notes and code selection.
Conduct monthly coding audits. I review 20-30 charts monthly with each client. This process identifies patterns and prevents future denials. You catch errors before payers do.
Stay current with code updates. Medicare publishes changes annually. I distribute updates to my practices quarterly. You avoid denials from outdated coding practices.
Train your team systematically. I run coding workshops covering common scenarios. Your staff gains confidence selecting appropriate codes. This training reduces coding delays and improves accuracy.
Results You Should Monitor
Track your clean claim rate monthly. I aim for 95% or higher with my clients. You identify coding problems through denial patterns. Clean claims accelerate your cash flow.
Monitor days in accounts receivable. Good coding reduces collection time. You should see AR days decrease as coding accuracy improves.
Review payer feedback regularly. Insurers provide denial reasons revealing coding weaknesses. I analyze these reports monthly with practices. You learn from mistakes and prevent repetition.
Strategies for Better Reimbursement
Focus on ICD-10-CM and CPT Category I codes first. These systems drive most of your revenue. You build expertise through consistent practice and education.
Implement regular coding audits in your practice. Monthly reviews catch problems early. You prevent costly compliance issues through proactive monitoring.
Invest in coding education for your team. I see immediate ROI from staff training programs. Your people become your strongest coding asset.
Medical coding complexity challenges every practice. You succeed by mastering one system at a time. Focus on accuracy over speed initially. Your reimbursement rates will reflect this investment in coding excellence.