After five years of helping medical practices reduce claim denials and improve reimbursements, I see the same challenge repeatedly. Healthcare billing departments struggle with manual payment posting, delayed cash flow recognition, and time-consuming administrative tasks. Electronic Remittance Advice (ERA) addresses these pain points while freeing up your team to focus on patient care.
Understanding what ERA in medical billing means transforms how you handle insurance payments. The practices I work with typically see immediate improvements in posting accuracy and staff productivity once they implement ERA processing.
What Is ERA in Medical Billing (ANSI 835)?
ERA delivers payment details from insurance companies in electronic format. Instead of paper documents arriving days after payment processing, you receive standardized data files containing complete claim information. This electronic system replaces the manual workflow that consumes hours of your billing team’s time each week.
An ERA is the electronic equivalent of a paper Explanation of Benefits (EOB), but instead of requiring staff to manually key in data, your billing software automatically imports and posts it.
Insurance companies send ERA files using the ANSI X12 835 transaction standard. These files contain complete payment information for all processed claims. Your practice management system imports this data directly, eliminating the manual entry tasks that create bottlenecks in your revenue cycle.
In my experience working with medical practices, teams processing 200+ claims daily save 10-15 hours per week after implementing ERA. This time savings translates directly into improved cash flow and reduced administrative costs.
ERA vs. EOB: Key Difference
| Aspect | ERA (Electronic Remittance Advice) | EOB (Explanation of Benefits) |
| Format | Digital file (ANSI 835) | Paper or PDF document |
| Delivery | Real-time / same day | 3–5 days by mail |
| Posting | Automatic | Manual entry |
| Error risk | Very low | High (manual keying) |
| Cash flow | Faster recognition | Slower deposits |
Core Elements Inside ERA Files
Every ERA file includes specific data points your billing team needs for accurate posting:
- Payment summary with total amounts and payment dates.
- Individual claim details with patient information.
- Procedure codes and service dates.
- Allowed amounts versus billed amounts.
- Reason codes explaining payment decisions.
- Adjustment details for contractual write-offs.
- Patient responsibility amounts including deductibles.
The 835 format organizes this information in consistent segments. Each segment contains predetermined data elements positioned in specific locations. This structure enables your billing software to process information automatically without human intervention.
From my work with various practice management systems, proper ERA configuration reduces posting errors by 85-90%. Your team spends less time correcting mistakes and more time resolving complex billing issues.
How ERA Improves Your Daily Operations?
ERA eliminates the time-consuming manual tasks that frustrate billing specialists. Your staff no longer types payment information from paper documents while trying to decipher handwritten notes or faded print. The system posts payments and adjustments automatically.
You receive payment information faster through electronic delivery. Paper remittance advice takes 3-5 business days to arrive through mail. ERA files reach you within hours of payment processing. This speed improvement helps practices maintain positive cash flow.
Staff productivity increases significantly when you implement ERA processing. I work with billing specialists who previously spent 4-6 hours daily on manual posting. After ERA implementation, they focus on denial management, patient communication, and complex case resolution.
The practices I advise report 40-50% faster claim issue resolution after implementing ERA. Electronic reason codes provide clear explanations for payment adjustments. Your team identifies patterns in denials and addresses root causes quickly.
Financial Analysis Benefits & Your Healthcare RCM
ERA provides rich data for tracking payer performance across your revenue cycle. You monitor first-pass claim acceptance rates for each insurance company in your patient mix. This information guides your contracting decisions and staff training priorities.
Denial pattern analysis becomes straightforward with ERA data. I help practices identify the top 10 reason codes causing claim rejections. This information guides process improvements that reduce future denials by 25-35%.
Revenue cycle metrics improve dramatically with ERA implementation. You track payment turnaround times, adjustment percentages, and collection rates in real-time. These measurements support strategic decision-making and help you negotiate better contracts with payers.
Compliance Advantages for Your Practice
Electronic records support audit requirements better than paper systems. ERA files provide complete audit trails showing payment posting activities with timestamps and user identification. You retrieve information quickly during compliance reviews or payer audits.
Internal controls strengthen with ERA processing. The system logs all posting activities automatically. This transparency supports regulatory compliance requirements while reducing the documentation burden on your staff.
HIPAA compliance improves through standardized electronic transactions. ERA follows established privacy and security protocols. Electronic processing reduces exposure risks associated with paper handling and storage.
Implementation Steps That Work
Your practice management system must support 835 transaction processing. Most modern systems include this capability, but I recommend verifying specifications before starting implementation. Older platforms may need upgrades or configuration changes.
Staff training becomes essential for successful ERA adoption. I develop training programs that help team members interpret reason codes and handle posting exceptions. Your staff learns to manage cases requiring manual intervention while maintaining productivity levels.
Workflow redesign accompanies ERA implementation. You establish procedures for exception handling and error resolution. Clear processes ensure smooth operations during the transition period and prevent workflow disruptions.
Setting Up ERA Processing for your Healthcare Practice
Contact your insurance partners to enroll in ERA programs. Most major payers offer electronic remittance options at no additional cost. Complete enrollment forms and provide banking information for electronic fund transfers.
Configure your billing system to receive and process ERA files. Set up automated importing schedules and posting rules based on your practice workflows. Test the system with sample files before processing actual transactions.
Monitor ERA processing during initial implementation. Review posting accuracy and identify any system issues early. Make adjustments to posting rules based on your specific payer mix and billing requirements.
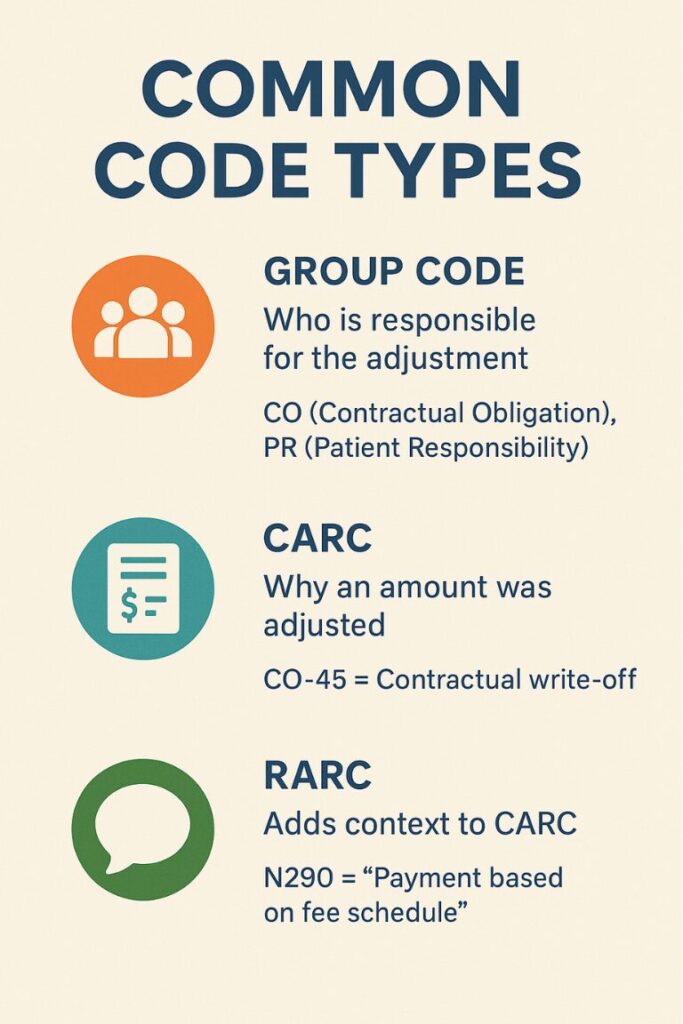
Common Code Types
| Code Type | Purpose | Example |
| Group Code | Who is responsible for the adjustment | CO (Contractual Obligation), PR (Patient Responsibility) |
| CARC | Why an amount was adjusted | CO-45 = Contractual write-off |
| RARC | Adds context to CARC | N290 = “Payment based on fee schedule” |
Example ERA Segment
CLP*12345*1*200*160*40*12*PAT12345*11~
CAS*PR*1*40~
NM1*QC*1*DOE*JANE****MI*ABC123456789~
SVC*HC:99213*200*160**1*20250905~
CAS*CO*45*40~
Interpretation:
- Claim paid $160 on a $200 bill
- Patient deductible = $40 (PR-1)
- Contractual write-off = $40 (CO-45)
Benchmark Your ERA Implementation
Track key performance indicators after ERA implementation. Measure posting accuracy rates, processing time reductions, and staff productivity gains. These metrics demonstrate return on investment and operational improvements to practice leadership.
Compare denial resolution times before and after ERA adoption. The practices I work with typically see 45 to 60% faster resolution cycles. Electronic processing enables quicker claim corrections and improved collection rates.
Monitor cash flow improvements resulting from ERA processing. Electronic payment notification accelerates deposit recognition and account reconciliation. This speed translates into better financial planning and cash management for your practice.
ERA transforms medical billing operations from manual processes to automated workflows. You gain speed, accuracy, and analytical capabilities while reducing administrative costs. Understanding what ERA in medical billing accomplishes helps your practice focus resources on patient care while maintaining financial health.
The revenue cycle improvements I see from ERA implementation consistently exceed expectations. Your billing team operates more efficiently, cash flow improves, and administrative burden decreases. These benefits create the operational foundation needed for sustainable practice growth.
Frequently Asked Questions
1. Is ERA the same as EOB?
No. An EOB is paper; ERA (ANSI 835) is electronic and enables auto-posting.
2. Do I need both ERA and EFT?
Yes — ERA gives you the payment details; EFT delivers the funds. Together, they create seamless reconciliation.
3. What if my payer doesn’t offer ERA?
Maintain manual posting for those payers and periodically re-check enrollment options.
4. Can ERA reduce denials?
Indirectly, yes — by exposing denial reason trends (CARC/RARC) so you can fix root causes faster.
5. How do I handle errors in ERA files?
Use your system’s exception queue, fix mappings, and re-import corrected files.
Conclusion
Electronic Remittance Advice isn’t just about speed, it’s about accuracy, compliance, and control. By adopting ERA + EFT, mapping codes carefully, and tracking key metrics, healthcare practices can reduce costs, accelerate cash flow, and free staff for higher-value work.
The result: a healthier, data-driven Revenue Cycle Management (RCM) process.