MEDICAL INSURANCE ELIGIBILITY VERIFICATION SERVICES
Smarter Insurance Checks.
Smoother Payments.

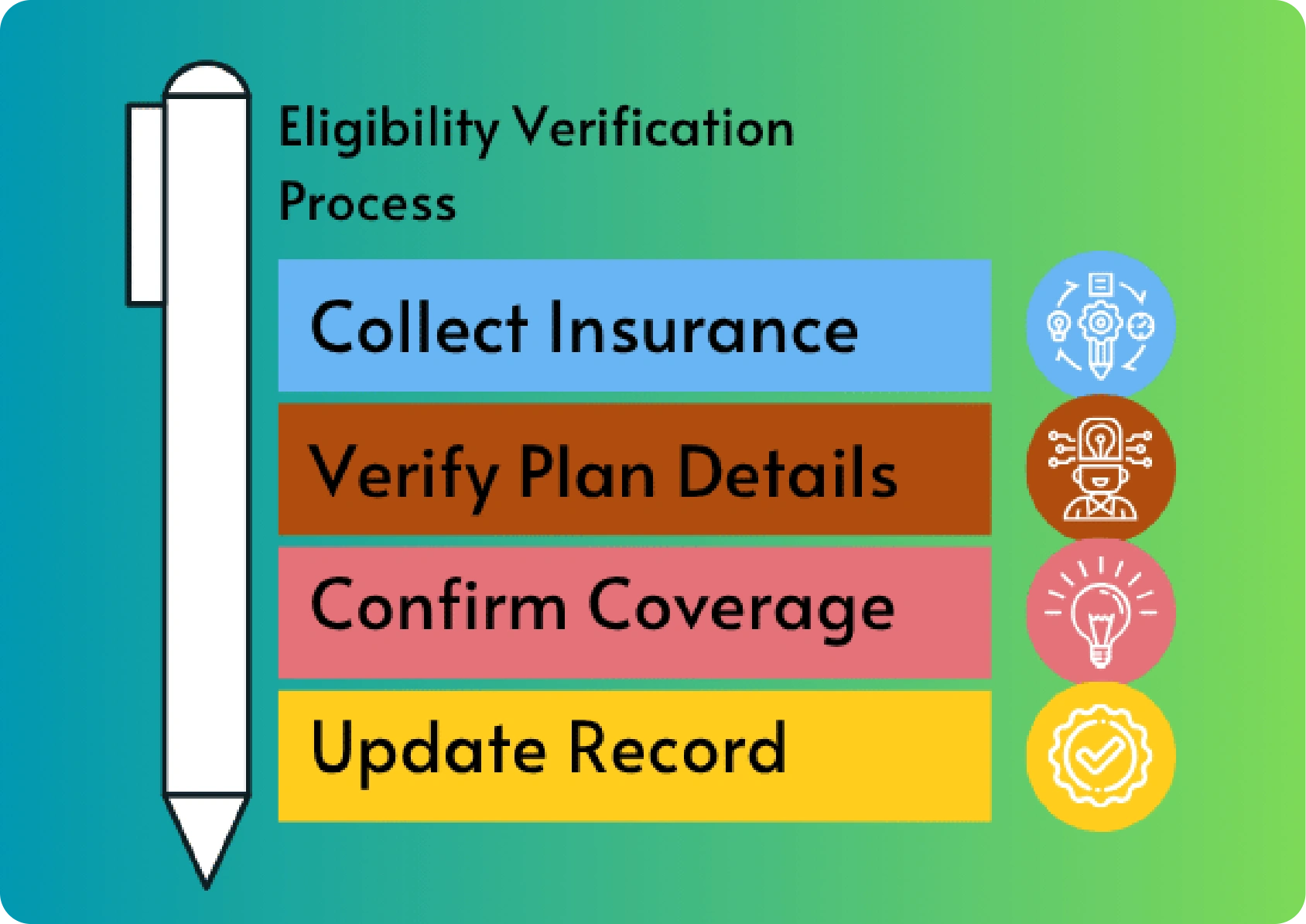
ELIGIBILITY VERIFICATION
Our Full Range of Eligibility Verification Services
As a trusted eligibility verification company, Greenhive Billing Solutions offers a complete set of solutions to verify health insurance coverage and ensure smooth billing operations.
- Patient insurance eligibility verification
- Verify patient insurance eligibility for all major and minor health plans
- Dependent verification services to confirm family member coverage
- Healthcare insurance eligibility verification services for specialty practices
- Medical insurance verification service for complex policies
- Check patient insurance eligibility for dental vision and specialty benefits
- Online health insurance eligibility check for fast and accurate results
A SMARTER WAY TO MANAGE REVENUE
What Makes Our Eligibility Verification Services Stand Out
Greenhive Billing Solutions combines technology and expertise to deliver reliable patient eligibility services. Our healthcare insurance eligibility verification services are tailored for the unique needs of practices and hospitals throughout the USA.
Comprehensive Coverage Checks
Advanced Systems for Accurate Results
Our eligibility verification company uses secure systems and HIPPA-compliant to check health insurance eligibility online and confirm policy details with insurers. This includes real-time patient eligibility checks and manual follow-ups when needed for complex cases.
Consistent Updates and Compliance
SERVICES
Why Patient Insurance Eligibility Verification is Critical for Your Practice
Every successful claim starts with verifying patient insurance eligibility. Without proper checks your practice risks delayed payments and claim resubmissions, increasing your workload and frustrated patients. Our patient insurance eligibility services ensure that you:
Verify patient insurance eligibility before appointments
Our team checks patient insurance eligibility thoroughly so you can be confident that each patient has active coverage and prior authorization is secured before services are provided.
Understand benefits co-pays and policy limits
Avoid costly errors and revenue loss
Verifying eligibility reduces billing errors and helps prevent claim rejections. If claims still get stuck, we follow up and resolve them. And once payments arrive, our payment posting services make sure everything is recorded accurately and revenue keeps flowing.
BENEFITS
Benefits of Verifying Patient Insurance Eligibility
Imagine a smoother medical billing process with fewer denials and faster reimbursements
Higher claim approval rates
Our patient insurance eligibility verification helps you submit error-free claims.
Stronger revenue cycle management
Accurate health insurance eligibility checks help you maintain predictable cash flow.
Better patient communication
Clear financial expectations reduce confusion and enhance satisfaction.
Reduced administrative workload
With upfront insurance verification, your staff spends less time fixing claim issues and more time focusing on patient care.
OUTCOMES
We Help You Target the
Right Outcomes
Processed from 2024 Date of Service (DOS)

Improve patient satisfaction
PREVENT DENIALS BEFORE THEY HAPPEN.
Take Control of Your Revenue Cycle Today
Eligibility issues account for a large portion of claim denials in healthcare. When you choose to outsource insurance eligibility verification services to Greenhive Billing Solutions, you protect your revenue, ease your administrative load, and create a smoother experience for your patients. Based in Tempe, AZ, our team ensures every patient’s insurance is verified with precision and reliability. Our Revenue Reporting & Analytics service tracks trends and patterns so you can fix problems before they reach payers.
ANY QUESTIONS?
Frequently Asked Questions
What is patient insurance eligibility verification?
Patient insurance eligibility verification is the process of confirming whether a patient’s insurance policy is active and what benefits it includes. This helps healthcare providers ensure that services will be covered by the patient’s health plan.
How do you verify patient insurance eligibility?
Patient insurance eligibility verification is the process of confirming whether a patient’s insurance policy is active and what benefits it includes. This helps healthcare providers ensure that services will be covered by the patient’s health plan.
Why is a patient eligibility check important for providers?
Patient insurance eligibility verification is the process of confirming whether a patient’s insurance policy is active and what benefits it includes. This helps healthcare providers ensure that services will be covered by the patient’s health plan.
Can you provide dependent verification services?
Patient insurance eligibility verification is the process of confirming whether a patient’s insurance policy is active and what benefits it includes. This helps healthcare providers ensure that services will be covered by the patient’s health plan.
How do I check health insurance eligibility online through your service?
Patient insurance eligibility verification is the process of confirming whether a patient’s insurance policy is active and what benefits it includes. This helps healthcare providers ensure that services will be covered by the patient’s health plan.
WE SUPPORT
Who We Serve
We support physicians clinics, hospitals specialty practices and healthcare networks across the USA. No matter the size of your practice our patient eligibility services are designed to fit your specific operational and financial goals.
