Medical billing has never been more complex. In 2026, healthcare practices face mounting administrative tasks, shifting payer rules, and a growing risk of costly errors. Studies show that billing inefficiencies cost practices billions each year.
This article explores the top 10 medical billing software designed to simplify operations, maximize revenue, and minimize mistakes. Discover the features, pricing, pros and cons, and best use cases for each solution.
Ready to reduce your administrative burden and improve your bottom line? Explore your options and find the best fit among the top 10 medical billing software available today.
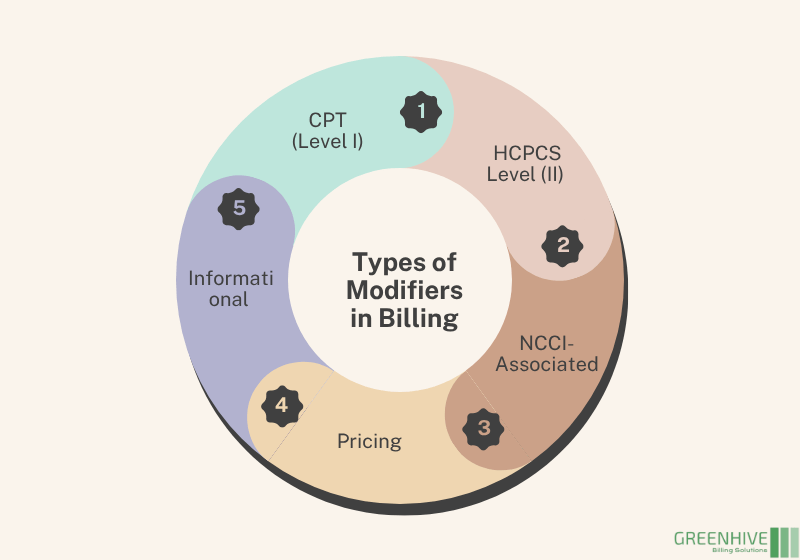
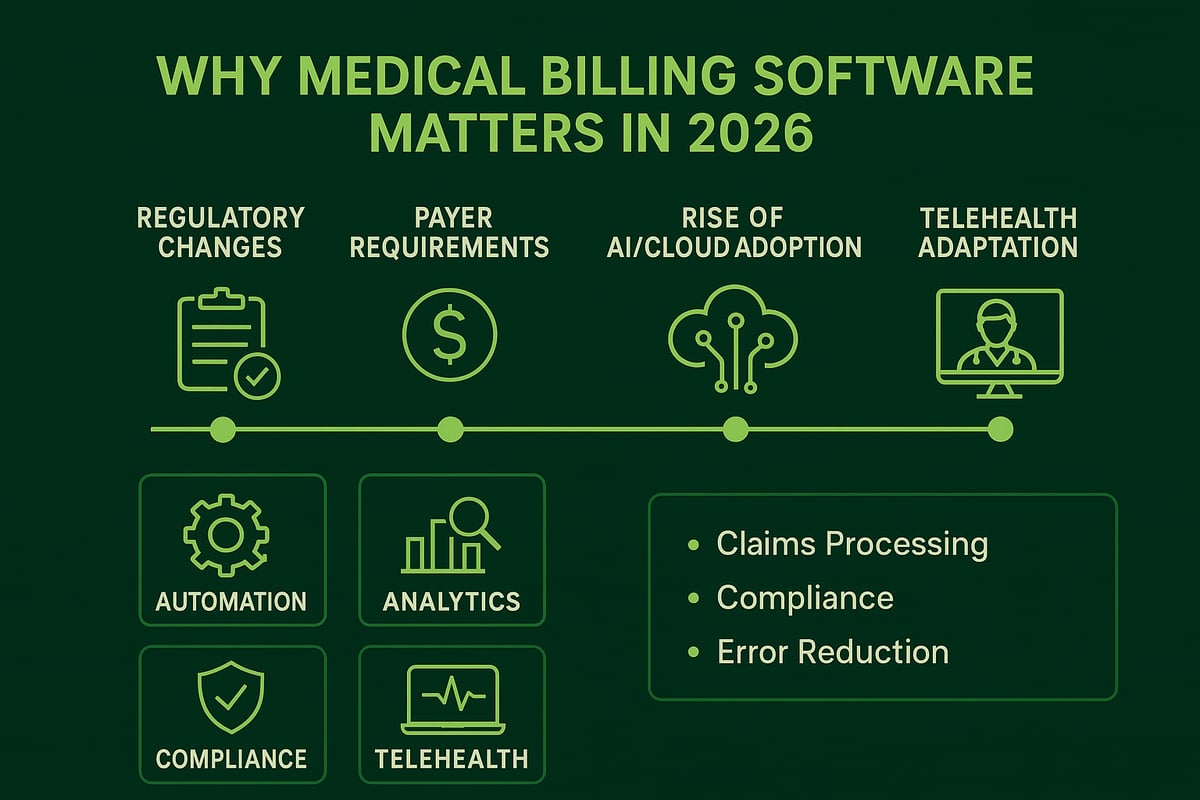
What is Medical Billing Software & Why It Matters in 2026
The healthcare billing landscape is evolving rapidly. New regulations, complex payer requirements, and the ongoing digital transformation are reshaping how practices manage revenue. In 2026, accuracy and speed in claims submission are more crucial than ever. As cloud-based and AI-powered tools gain traction, practices are turning to the top 10 medical billing software solutions to keep pace with industry demands and minimize costly errors.
The Evolving Landscape of Healthcare Billing
Healthcare billing in 2026 faces unprecedented complexity. Regulatory bodies frequently update compliance standards, while payers demand precise, timely documentation. The top 10 medical billing software options help practices navigate this shifting terrain by automating workflows and supporting fast, accurate submissions.
Digital transformation is another driving force. Practices are rapidly adopting cloud-based and AI-driven solutions to streamline billing, reduce manual effort, and ensure security. This shift allows both small clinics and large organizations to stay competitive, respond to regulatory changes, and maintain efficient billing operations.
Core Functions of Medical Billing Software
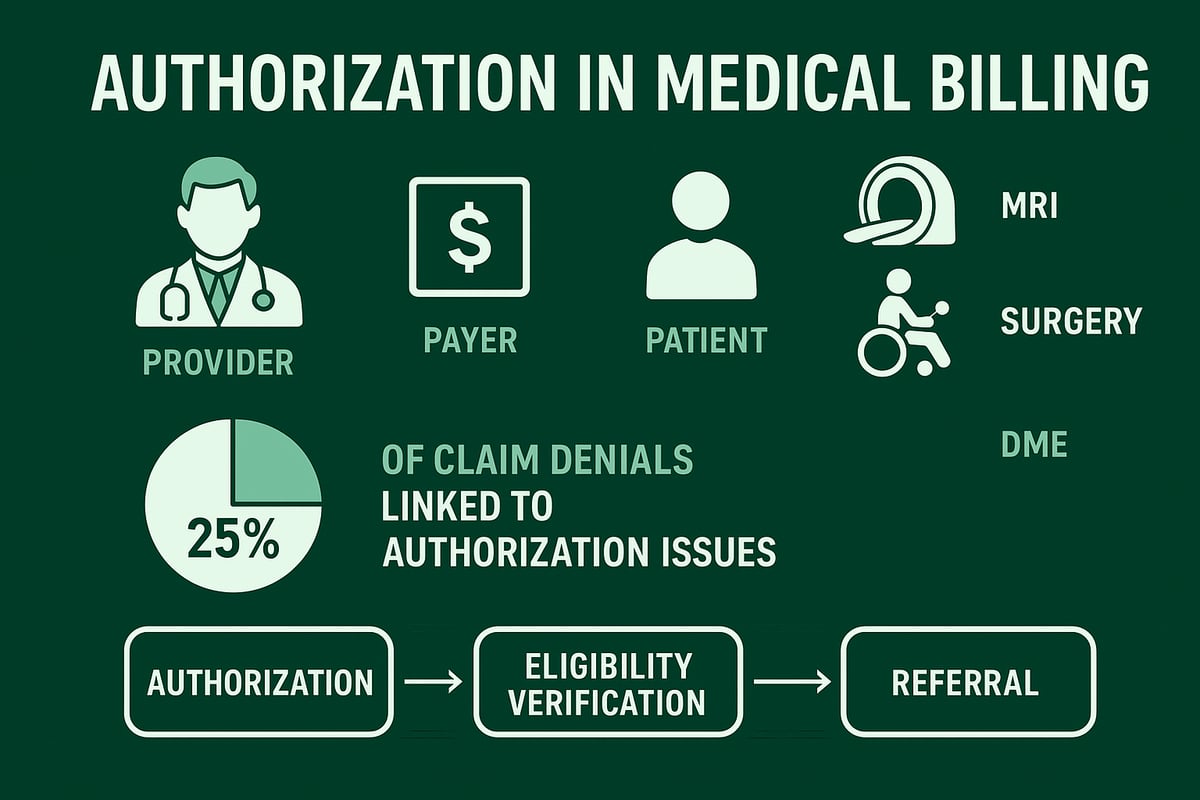
At the heart of every top 10 medical billing software platform are several essential functions. These systems automate the entire claims process, from insurance verification and eligibility checks to payment posting and denial management. Integration with EHR and EMR systems ensures seamless data flow, reducing duplication and errors.
Modern solutions also provide real-time analytics and compliance tracking, empowering practices to make informed decisions. Many platforms offer specialty-specific coding support and automated claim scrubbing to further reduce denials. For a deeper dive into how denial management impacts cash flow, see Denial Management in Medical Billing.
Key Benefits for Modern Practices
Choosing the right top 10 medical billing software brings measurable advantages. Automation reduces manual errors and administrative workload, freeing staff to focus on patient care. Faster reimbursement cycles improve cash flow and financial stability for practices of all sizes.
Advanced platforms enhance compliance with HIPAA and payer policies, reducing audit risks. Scalability is built-in, enabling growing or multi-location practices to expand with confidence. These benefits collectively help practices thrive in a dynamic healthcare environment.
Challenges Solved by Top Solutions
The top 10 medical billing software options tackle persistent industry challenges. Automated claim scrubbing minimizes denials and delays, ensuring cleaner submissions and faster payments. Specialty-specific coding features support unique billing needs across various fields.
Transparent patient billing and clear communication are prioritized, improving patient satisfaction and reducing confusion. Adaptability to telehealth and hybrid care models means practices can offer flexible services without billing obstacles. By addressing these pain points, leading solutions drive operational efficiency and better outcomes for both providers and patients.
Top 10 Medical Billing Software to Streamline Practice 2026
Choosing the right tool from the top 10 medical billing software options can transform a healthcare practice’s revenue cycle, efficiency, and patient satisfaction. With a rapidly evolving regulatory landscape and increasing patient volumes, practices need robust, scalable solutions. Below, we explore each leading platform, highlighting features, pricing, and ideal fit to help you navigate the crowded market and select the best software for your needs.
Greenhive Billing Solutions
Greenhive Billing Solutions stands out among the top 10 medical billing software platforms for its transparent, results-based pricing and comprehensive revenue cycle management. This software is designed for solo providers, small practices, and multi-specialty clinics, delivering HIPAA-compliant processes and encrypted data security.
Key features include seamless EHR and PMS integration, specialty-specific billing, real-time analytics, and access to dedicated account managers. Practices benefit from a clean claims guarantee, nationwide payer expertise, and scalable solutions. Regular audits ensure compliance and data integrity.
- Pros: Maximum transparency, clean claims guarantee, 24/7 U.S.-based support.
- Cons: Outsourced service model may not suit those preferring in-house software.
Ideal for practices seeking end-to-end revenue cycle management with full support and no hidden fees, Greenhive offers a robust choice within the top 10 medical billing software landscape.
DrChrono
DrChrono is a cloud-based, integrated EHR and billing platform, making it a mainstay in any list of top 10 medical billing software for small to medium-sized practices. It offers real-time insurance eligibility checks, denial analysis, and customizable billing profiles.
With subscription pricing starting at $199 per month, DrChrono provides mobile access, robust reporting, and seamless scheduling integration. Its user-friendly interface and strong automation make it popular among providers.
- Pros: Easily scalable, intuitive design, mobile-friendly.
- Cons: Some advanced analytics require add-ons.
Best suited for practices looking for an all-in-one workflow management solution, DrChrono is especially valuable for teams that need mobile access and streamlined operations.
Kareo Billing
Kareo Billing is engineered for independent practices and billing companies, earning its spot in the top 10 medical billing software due to its cloud-driven tools and affordability. Real-time claim tracking, billing analytics, and automated workflows are core strengths.
Pricing starts at $125 per month per provider, making Kareo accessible for smaller practices. The dashboard is intuitive, and the solution simplifies collections and reduces manual tasks.
- Pros: Affordable, excellent support, customizable workflows.
- Cons: Advanced integration options are limited for larger enterprises.
Kareo Billing is ideal for independent providers who want a straightforward, effective medical billing solution without unnecessary complexity.
NextGen Healthcare
NextGen Healthcare’s cloud-based platform is a powerful contender among the top 10 medical billing software, offering user-friendly workflows and integrated clinical and financial tools. The software supports accurate claim submissions, patient payment options, and rapid claims processing.
Custom pricing ensures practices only pay for the features they need. Implementation support and training are included, helping practices reduce denials and maintain compliance.
- Pros: Reduces denials, regulatory compliance, scalable.
- Cons: May have a steeper learning curve for new users.
NextGen Healthcare is best for growing practices that need a scalable, compliant billing system with integrated EHR capabilities.
Practice EHR
Practice EHR is purpose-built for small and medium practices, securing its place among the top 10 medical billing software for 2026. It combines cloud-based EHR, billing, and practice management into a single platform.
Features include automated claims processing, real-time eligibility checks, and transparent billing. Pricing starts at $149 per month per provider, with certified billers and specialty-specific support.
- Pros: Transparent processes, clean claims, flexible service options.
- Cons: Limited customization for very large practices.
Practice EHR is a top pick for practices seeking simplicity, transparency, and expertise in specialty billing.
AdvancedMD
AdvancedMD is a comprehensive cloud-based EHR and billing solution that consistently ranks in the top 10 medical billing software for practices of all sizes. It offers integrated credit card processing, online charge slips, and robust financial analytics.
Pricing is custom, typically starting at $429 per month per provider. AdvancedMD’s workflow automation and scalable modules ensure it meets the needs of multi-provider practices.
- Pros: Highly customizable, strong support, advanced analytics.
- Cons: Higher price point, complex initial setup.
AdvancedMD is perfect for practices needing advanced analytics, customizable workflows, and scalability to grow with their needs.
eClinicalWorks
eClinicalWorks is a leading cloud-based EHR with powerful revenue cycle management tools, making it a staple in the top 10 medical billing software lists. It features automated workflows, claim edit rules, ERA management, and AI-driven insights.
Custom pricing provides flexibility for large practices and multi-specialty clinics. Natural language billing queries and specialty-specific automation set eClinicalWorks apart.
- Pros: Robust automation, scalable, deep customization.
- Cons: Complex interface for beginners.
eClinicalWorks is best for large practices or clinics requiring advanced customization and automation in their billing processes.
CureMD
CureMD delivers cloud-based billing and practice management for a wide range of specialties, earning its spot in the top 10 medical billing software. Features include real-time claim scrubbing, specialty-specific billing, and comprehensive RCM services.
Pricing starts at $195 per month per provider, with strong support for specialties like cardiology, radiology, and neurology. The software minimizes denials and improves billing accuracy.
- Pros: Versatile, accurate, tailored specialty modules.
- Cons: Some advanced features require additional fees.
CureMD is ideal for specialty practices seeking a billing solution tailored to their unique needs.
Practice Fusion
Practice Fusion is a cloud-based EHR and billing system designed for small or independent practices, cementing its place in the top 10 medical billing software for affordability and ease of use. Patient communication tools, insurance AR follow-up, and automated claim scrubbing are included.
The EHR is free, with variable billing costs through integrated partners. Practice Fusion offers easy onboarding, payor compliance tools, and transparent workflows.
- Pros: Low cost, user-friendly, fast implementation.
- Cons: Limited advanced features, relies on third-party billing partners.
Best for small practices and startups needing a cost-effective, simple billing solution.
Epic Systems
Epic Systems is an enterprise-grade EHR with integrated billing and revenue cycle management, making it a heavyweight in the top 10 medical billing software for large organizations. Features include electronic insurance verification, customizable workflows, and advanced analytics.
Pricing is custom and geared toward hospitals and large health systems. Epic is lauded for seamless interoperability, eligibility confirmation, and robust self-pay options.
- Pros: Highly customizable, trusted by large health systems, robust analytics.
- Cons: Expensive, complex deployment.
Epic Systems is best suited for hospitals and large organizations with complex billing requirements and a need for advanced interoperability.
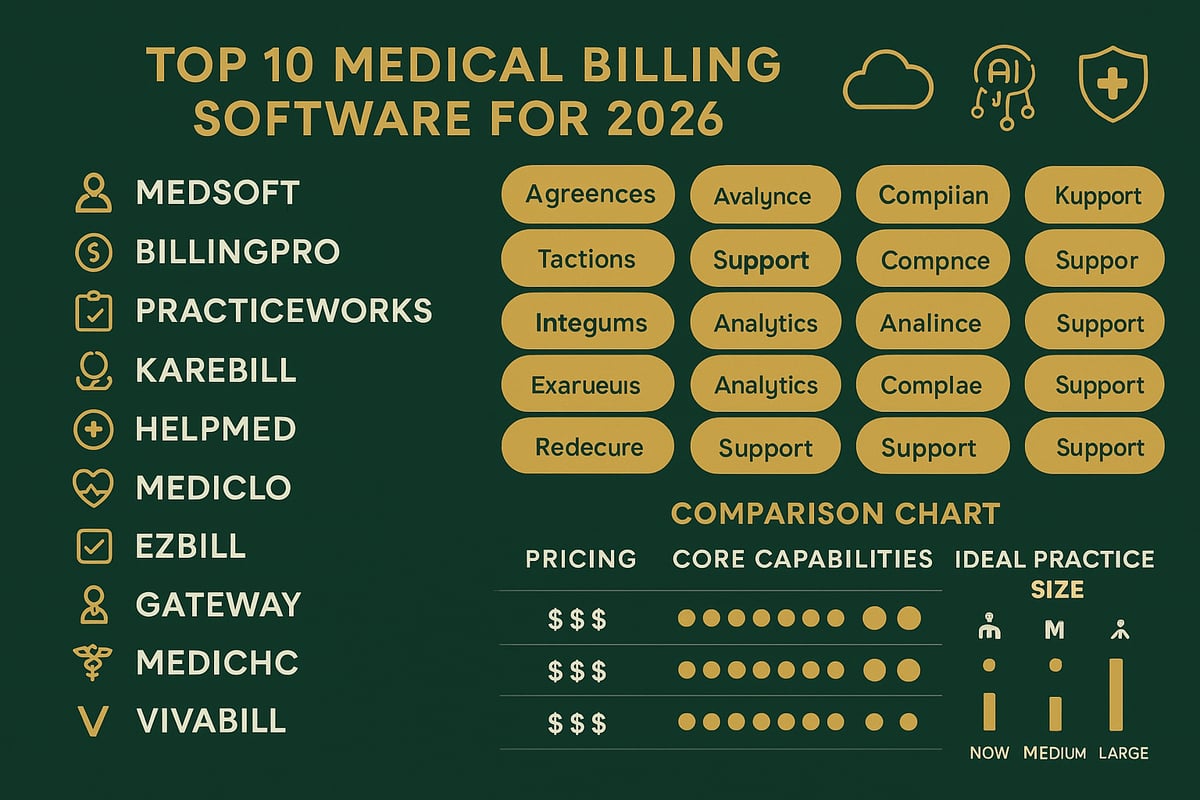
Comparison Table: Top 10 Medical Billing Software at a Glance
| Software | Best For | Starting Price | Key Features | Pros | Cons |
|---|---|---|---|---|---|
| Greenhive Billing | End-to-end RCM, support | Custom | Clean claims, analytics, support | Transparency, guarantee | Outsourced model |
| DrChrono | Mobile, all-in-one | $199/mo | Real-time eligibility, reporting | Scalable, user-friendly | Add-ons needed |
| Kareo Billing | Small practices | $125/mo | Claim tracking, analytics | Affordable, support | Limited integration |
| NextGen Healthcare | Growing practices | Custom | Payment options, compliance | Reduces denials | Learning curve |
| Practice EHR | Simplicity, specialties | $149/mo | Transparency, specialty support | Clean claims, flexibility | Customization limits |
| AdvancedMD | Large, multi-provider | $429+/mo | Financial analytics, automation | Customizable, analytics | Price, setup |
| eClinicalWorks | Large/multi-specialty | Custom | AI insights, ERA management | Automation, customization | Complex interface |
| CureMD | Specialty practices | $195/mo | Claim scrubbing, specialty modules | Versatile, accurate | Extra fees |
| Practice Fusion | Small/startups | Free EHR | Communication, claim scrubbing | Low cost, user-friendly | Limited features |
| Epic Systems | Enterprise/hospitals | Custom | Insurance verification, analytics | Customizable, robust | Expensive, complex |
For further insight into market trends influencing the top 10 medical billing software, see the latest Medical Billing Software Market Growth & Trends report.
How to Choose the Right Medical Billing Software for Your Practice
Selecting the right solution from the top 10 medical billing software options can transform your practice’s efficiency and financial health. With so many platforms available in 2026, it is crucial to make an informed decision tailored to your specific needs. Below, we break down a practical approach to evaluating and choosing the best fit for your organization.
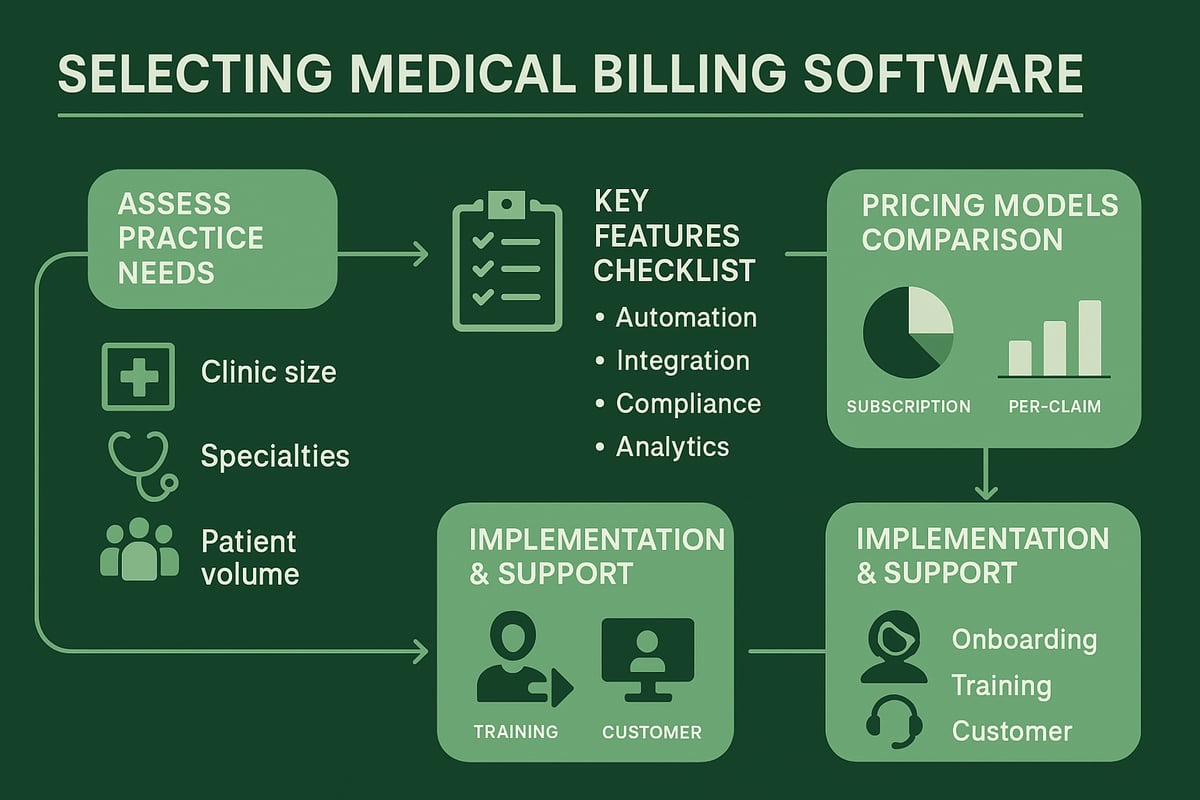
Assessing Your Practice’s Needs
Begin by analyzing your practice’s size, specialty focus, and patient volume. These factors directly influence the complexity of your billing requirements and the features you will need from the top 10 medical billing software solutions.
Identify current challenges, such as frequent claim denials, slow reimbursements, or difficulty managing multi-location workflows. For small clinics or solo providers, consider reviewing Medical Billing Services for Small Practices to see how software and service combinations can address unique needs.
Ask yourself:
- Does your specialty require advanced coding support?
- Are you planning for growth or multi-site expansion?
- What is your current administrative workload?
Defining these parameters will help you focus on solutions best suited for your operational realities.
Key Features to Consider
Not all systems on the top 10 medical billing software list offer the same capabilities. Prioritize platforms that include:
- Automated claims submission and scrubbing
- Seamless integration with EHR/EMR systems
- Built-in compliance updates and alerts
- Real-time analytics and reporting dashboards
Specialty-specific coding, denial management, and robust customer support are also essential. To dive deeper into analytics, explore Reporting and Analytics in Billing for insights on how advanced reporting can drive better financial decisions.
Assess whether the interface is user-friendly and if the software supports telehealth, hybrid care, and transparent patient billing. These features ensure your practice stays compliant and competitive.
Pricing Models & ROI Considerations
Understanding the pricing structure of top 10 medical billing software options is vital for budgeting and long-term planning. Models typically include:
- Subscription-based (monthly/annual per provider)
- Per-claim or transaction fees
- Results-based or percentage of collections
Calculate the total cost of ownership, including setup, integration, training, and ongoing support. Evaluate the return on investment by considering how the software will reduce administrative time, minimize errors, and accelerate cash flow.
Review available add-ons or hidden fees that may affect your budget. A clear understanding of costs versus benefits will help you select a solution that maximizes value for your practice.
Implementation, Training & Support
Successful adoption of top 10 medical billing software depends on effective onboarding and continuous support. Assess the vendor’s implementation process, including data migration, timeline, and dedicated assistance.
Check if the provider offers comprehensive training resources for your staff and if ongoing support is accessible via multiple channels. Responsive customer service can make a significant difference when resolving billing or technical issues.
Prepare your team for the learning curve and ensure regular training sessions to keep up with software updates and regulatory changes. A strong support system will help your practice maintain efficiency and compliance as you scale.
Future Trends in Medical Billing Software (2026 & Beyond)
The landscape of medical billing is evolving rapidly, and the top 10 medical billing software providers are already shaping the future. As we look ahead to 2026 and beyond, practices must prepare for transformative changes in automation, integration, compliance, and analytics. Understanding these trends will help organizations select solutions that remain competitive, efficient, and secure.
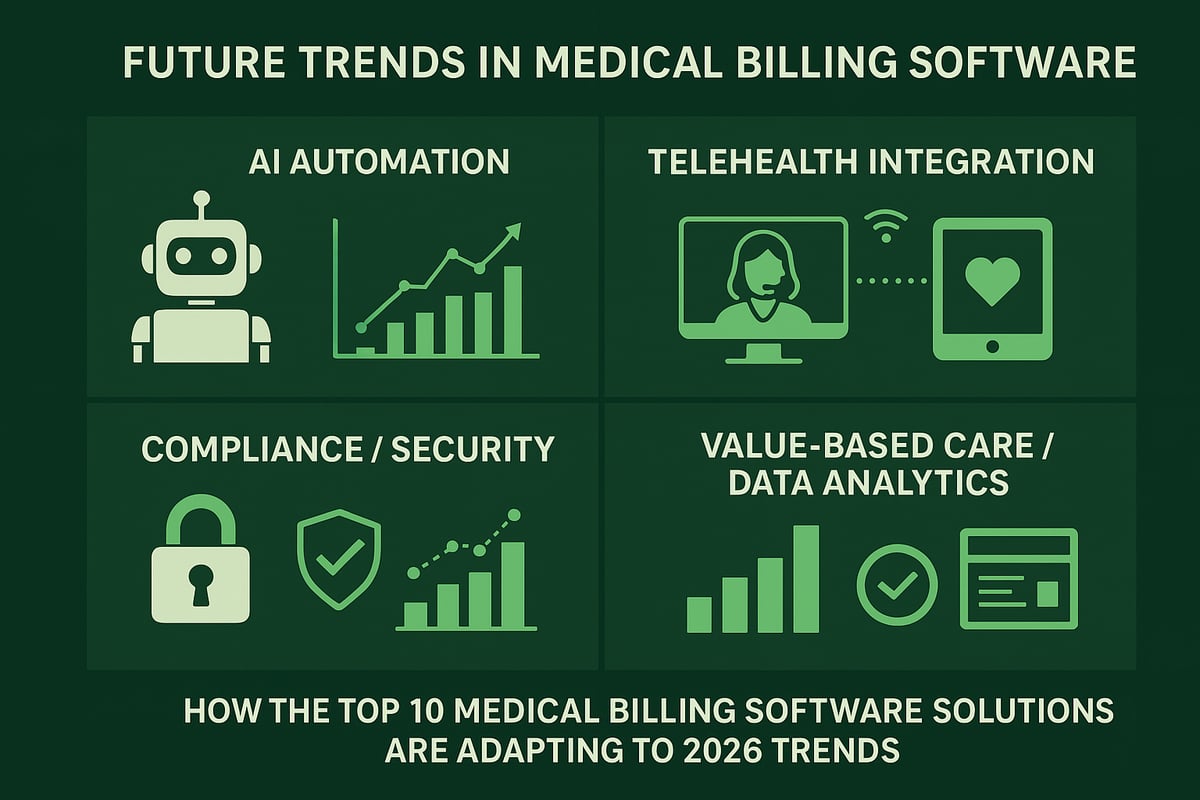
AI & Automation in Revenue Cycle Management
AI-powered tools are redefining how the top 10 medical billing software platforms handle revenue cycle management. Predictive analytics now forecast claim approvals and denials with remarkable accuracy, reducing costly rework and delays. Automation extends to coding, where advanced algorithms identify potential errors before submission.
For example, leading solutions use machine learning to flag anomalies and optimize claim edits in real time. Automated denial management speeds up appeals and ensures faster reimbursements. This trend is expected to accelerate, with AI and Automation in Medical Billing playing a vital role in reducing administrative burdens and improving financial outcomes.
Integration with Telehealth & Patient Engagement
As telehealth becomes a standard care model, the top 10 medical billing software offerings are prioritizing unified billing for both virtual and in-person visits. Seamless integration with telehealth platforms ensures accurate charge capture and eligibility verification, regardless of care setting.
Enhanced patient payment portals are another key development. Patients can easily review statements, manage balances, and communicate with billing teams online. Improved transparency leads to higher satisfaction and faster collections. These advancements support the growing demand for flexible, patient-centric billing experiences.
Compliance, Security & Regulatory Updates
Compliance requirements are evolving, and the top 10 medical billing software vendors are enhancing their platforms to meet new standards. Practices must adapt to changing HIPAA, CMS, and payer regulations, which increasingly mandate advanced encryption and real-time compliance monitoring.
Modern solutions provide detailed audit trails and automated alerts for potential breaches. Security features, such as multi-factor authentication and role-based access, protect sensitive patient data. Staying ahead of regulatory changes is essential for practices to avoid penalties and maintain trust.
The Rise of Value-Based Care & Data Analytics
Value-based care is transforming reimbursement, and the top 10 medical billing software systems are responding with robust analytics. These platforms support quality metrics tracking, enabling practices to demonstrate performance and maximize value-based payments.
Sophisticated dashboards deliver actionable insights into operational and financial trends. By leveraging data, practices make informed decisions that drive growth and compliance. For a deeper look at upcoming innovations, see Emerging Medical Billing Trends in 2026, which highlights how analytics and automation are shaping the industry.
If you’re feeling overwhelmed by the fast-changing demands of medical billing in 2026, you’re not alone. Choosing the right software can make all the difference in streamlining your workflows and boosting your bottom line—whether you manage a solo practice or a multi-specialty clinic. At Greenhive Billing Solutions, I understand how essential it is to get tailored support, transparent communication, and proven results. If you’re ready to explore the best-fit option for your unique needs or have questions about optimizing your revenue cycle, I invite you to Book Your Free Consultation. Let’s work together to strengthen your practice’s financial future.