Healthcare organizations today face rising complexity and mounting financial pressures. Shifting reimbursement models, regulatory demands, and evolving patient expectations create constant challenges for providers.
Effective revenue management is now more critical than ever. Without the right approach, organizations risk revenue leakage and operational setbacks. This guide explores the essentials of revenue management solutions healthcare leaders need to navigate this changing landscape.
We will examine current industry challenges, outline the core components of successful solutions, highlight key technology trends, and provide actionable steps for implementation. Our goal is to help you improve operational efficiency, boost financial performance, and future-proof your practice.
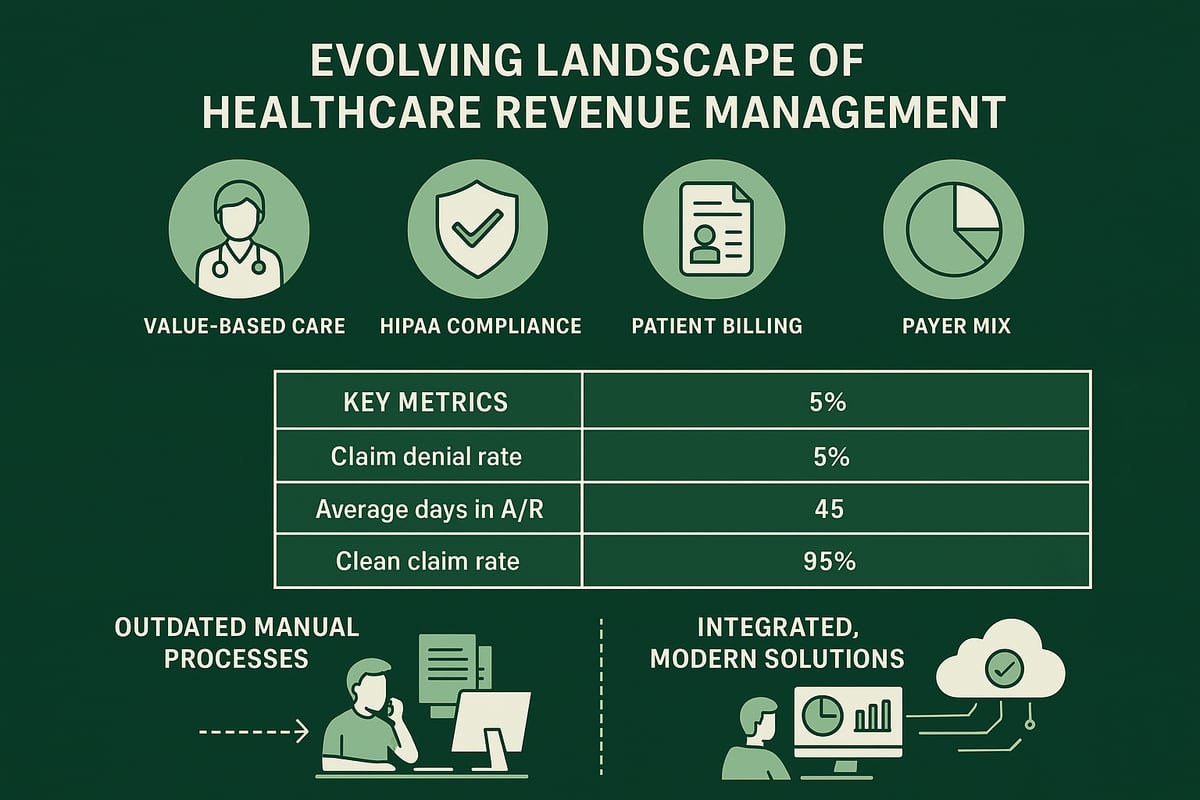
The Evolving Landscape of Healthcare Revenue Management
Healthcare organizations are navigating a landscape defined by rapid change and increasing complexity. Shifts toward value-based care and bundled payment models challenge the traditional fee-for-service approach. Providers must now demonstrate outcomes and efficiency, not just volume, to secure reimbursements.
Regulatory demands continue to rise. HIPAA compliance, price transparency rules, and evolving payer requirements require constant attention. Patient consumerism is also reshaping financial interactions. With higher deductibles and co-pays, patients now shoulder a greater share of costs, making clear communication and flexible payment options essential.
Payer mix variability and intricate insurance plans add another layer of difficulty. The result? Growing rates of claim denials and longer average days in accounts receivable. Consider these telling statistics:
| Key Metric | Industry Average |
|---|---|
| Claim Denial Rate | 6–13% |
| Average Days in A/R | 30–50 days |
| Clean Claim Rate (best-practice) | 95%+ |
Outdated manual workflows can cause revenue leakage. For example, missing eligibility checks or coding errors often lead to rework, delayed payments, or lost revenue. This makes it critical for organizations to adopt integrated, adaptable revenue management solutions healthcare teams can rely on for accuracy and efficiency.
To address these challenges, many practices are turning to streamlined processes and expert support. For a detailed overview of each step and best practices, see the Revenue cycle process in healthcare.
Staying ahead requires more than just incremental fixes. Healthcare organizations need flexible revenue management solutions healthcare professionals can trust to keep pace with regulatory shifts, evolving payer expectations, and changing patient needs.
Core Components of Revenue Management Solutions
A robust approach to revenue management solutions healthcare starts with understanding its essential building blocks. Each component works together to minimize revenue leakage, enhance compliance, and ensure sustainable financial health for healthcare organizations.
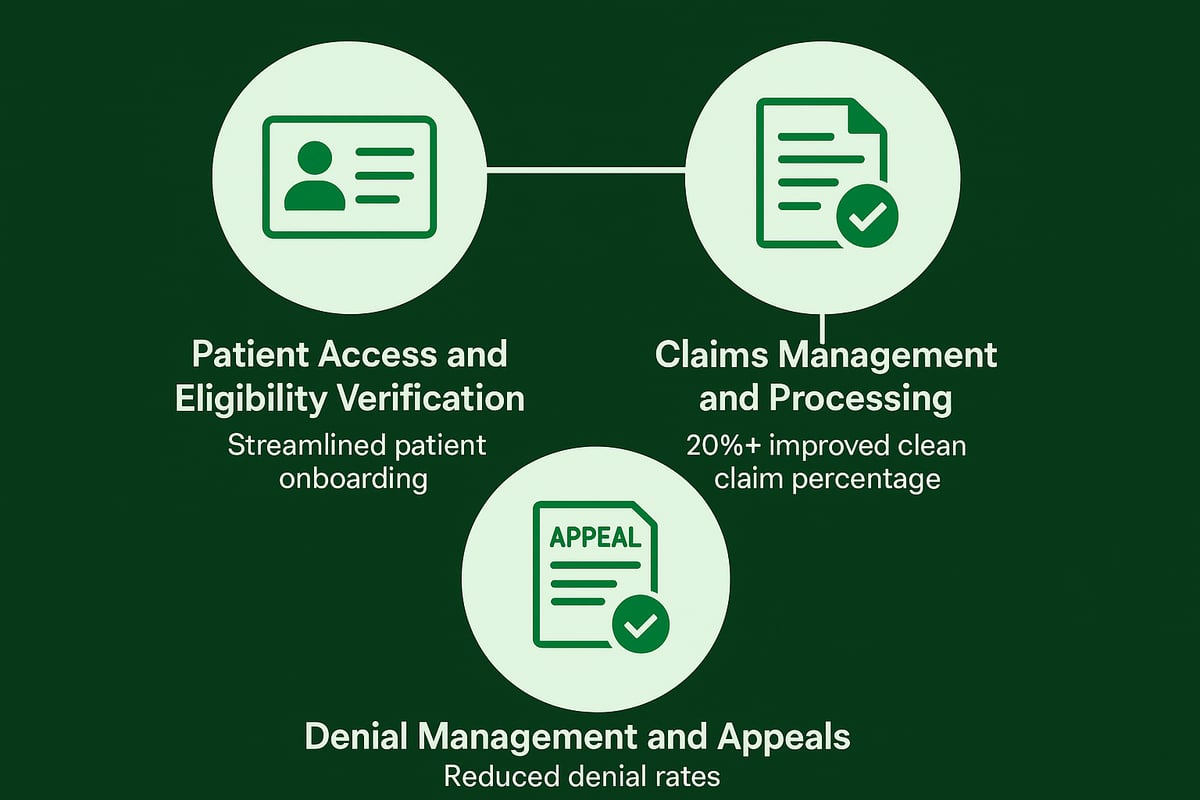
Patient Access and Eligibility Verification
Accurate insurance verification at the front end is vital for successful revenue management solutions healthcare. Eligibility errors often result in claim denials, delayed payments, and dissatisfied patients.
Practices leveraging automated eligibility verification see up to a 30% drop in denials. This proactive step ensures coverage details are correct and out-of-pocket costs are clear, setting the stage for a smoother revenue cycle.
Claims Management and Processing
Effective claims management is at the core of revenue management solutions healthcare. The process includes charge capture, precise coding, timely claim submission, and diligent tracking.
Certified billing professionals help reduce errors and maintain compliance. Organizations with strong workflows consistently achieve clean claim rates above 95%, accelerating reimbursements and reducing administrative burden.
Denial Management and Appeals
Denials often stem from coding mistakes, missing documentation, or eligibility issues. Proactive root cause analysis and structured workflows are essential for rapid resolution.
By implementing Denial management in medical billing strategies, organizations can recover 10–15% more revenue. Consistent follow-up and data-driven appeals processes turn potential losses into tangible gains.
Technology Trends Shaping Revenue Management
Healthcare organizations are rapidly embracing transformative technologies to optimize revenue management solutions healthcare. From automation to advanced analytics, these innovations are reshaping how providers manage financial operations and adapt to growing complexity.
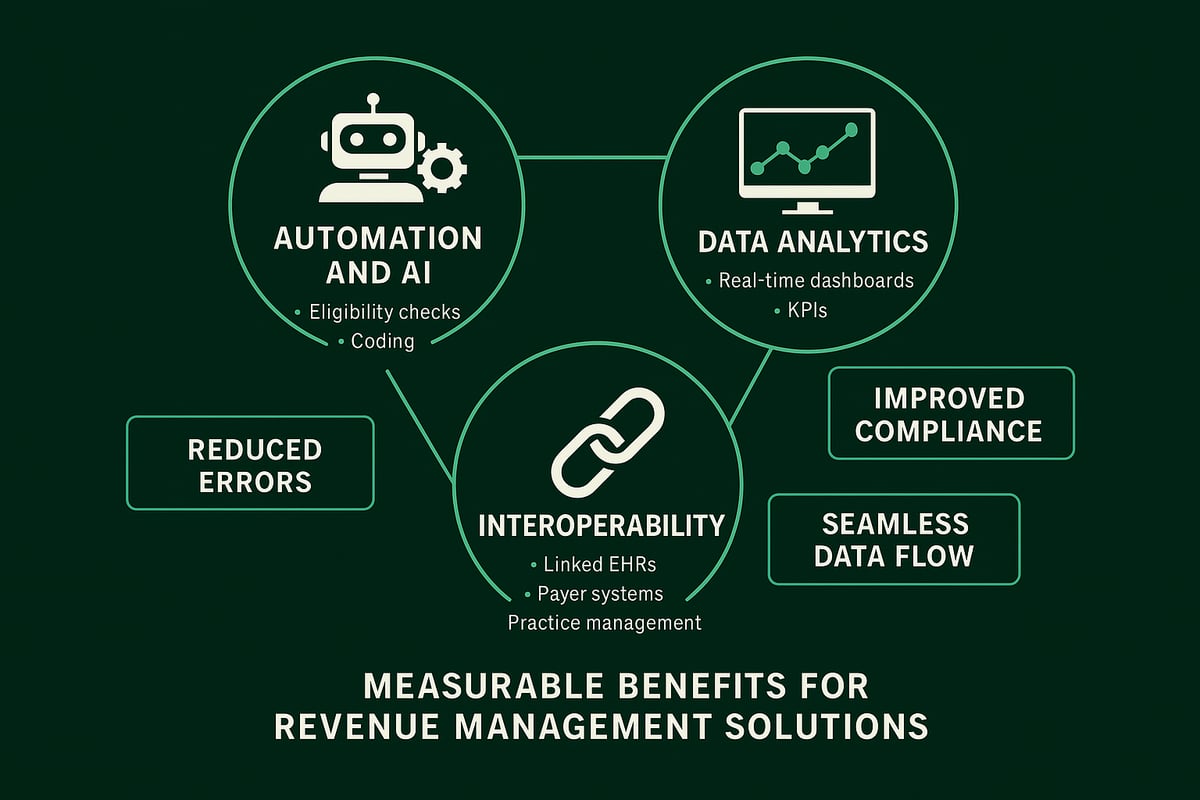
Automation and Artificial Intelligence
Automation and AI are revolutionizing revenue management solutions healthcare by streamlining repetitive tasks and minimizing manual errors. Robotic process automation (RPA) and AI tools handle eligibility checks, coding, and claims scrubbing with unmatched speed and accuracy.
These technologies accelerate claim processing times and ensure compliance with regulatory requirements. Organizations leveraging automation report fewer denials and improved cash flow, enabling finance teams to focus on complex cases and strategic initiatives.
Data Analytics and Revenue Reporting
Data analytics has become the backbone of modern revenue management solutions healthcare. Real-time dashboards track key performance indicators such as A R days and denial rates, offering immediate insights for decision-makers.
Providers are now leveraging advanced analytics for predictive insights and accurate revenue forecasting. For a deeper dive into the latest analytics innovations, see Healthcare revenue cycle analytics. These tools empower organizations to identify bottlenecks, benchmark performance, and drive continuous improvement.
Interoperability and Integration
Interoperability is essential for revenue management solutions healthcare, ensuring seamless connectivity between EHRs, practice management systems, and payers. Integrated platforms eliminate data silos, increase data accuracy, and streamline workflows across departments.
This connectivity leads to faster eligibility verification, efficient claims processing, and a better patient experience. By investing in integrated systems, healthcare providers boost both operational efficiency and financial performance.
Best Practices for Implementing Revenue Management Solutions
Implementing revenue management solutions healthcare requires a structured approach to achieve measurable financial improvements. By following proven best practices, healthcare organizations can streamline operations, boost reimbursements, and minimize errors.
Assessing Organizational Needs and Readiness
Start by conducting a comprehensive workflow audit to identify current pain points and inefficiencies. Engage stakeholders from finance, clinical, and IT departments to gain a holistic view. This ensures your revenue management solutions healthcare implementation targets real challenges and aligns with organizational goals.
Review existing processes, technology, and staff capabilities. Prioritize areas with high denial rates or delayed reimbursements. For additional strategies, see the Top 5 Ways to Optimize Healthcare Revenue Cycle Management.
Selecting the Right Solution Partners
Choose service partners with proven expertise in revenue management solutions healthcare. Evaluate candidates based on scalability, specialty experience, compliance credentials, and support infrastructure.
Request case studies to confirm measurable outcomes. Transparent communication and a strong track record are essential for a successful partnership. Ensure the partner can adapt to your existing software and workflows for seamless integration.
Training and Change Management
Comprehensive staff training is vital for maximizing the value of new processes. Offer hands-on learning sessions and provide ongoing support to boost confidence and minimize resistance.
Monitor staff adoption rates and gather feedback for continuous improvement. Regular refresher courses help maintain compliance and performance standards.
Greenhive Billing Solutions: Expert Revenue Cycle Management Services
Greenhive delivers comprehensive revenue management solutions healthcare organizations rely on to streamline their financial operations and maximize reimbursement. Our experienced team partners with providers, clinics, and medical groups, offering services such as eligibility verification, claims processing, denial management, and revenue reporting.
We prioritize HIPAA compliance, transparent communication, and tailored workflows that meet each specialty’s unique needs. By leveraging our Eligibility verification services overview, clients reduce claim denials and accelerate payments. Practices consistently report increased clean claim rates, reduced A/R days, and significant cost savings after engaging Greenhive.
Our experts seamlessly adapt to client-owned software and existing systems, providing support that drives operational efficiency and measurable results. Greenhive stands out as a trusted B2B partner, committed to optimizing every aspect of your revenue cycle.
Future-Proofing Revenue Management: Strategies for Sustainable Success
Adapting to the future of healthcare requires more than just reacting to change. Organizations need to be proactive in how they approach revenue management solutions healthcare, especially as regulations, payer rules, and patient expectations continue to evolve. Staying ahead means understanding what is coming and building a strategy that is both resilient and agile.
Keeping up with regulatory changes is vital. New rules on price transparency, reimbursement, and data privacy can have immediate financial impacts. By monitoring healthcare trends for 2026 and beyond, providers can anticipate shifts and adjust processes before compliance issues arise.
Process improvement should be ongoing, not a one-time event. Regular performance reviews, internal audits, and benchmarking against industry standards help teams identify revenue leakage and streamline operations. Engaging clinical, administrative, and financial staff in continuous education ensures everyone is prepared for new payer requirements and system updates.
Investing in technology and data analytics is another key strategy. Leveraging automation, predictive analytics, and AI-powered tools can improve accuracy, speed, and compliance. According to AI in Healthcare Financial Planning, organizations that use advanced analytics gain better forecasting and risk management capabilities.
Building flexible workflows is essential as reimbursement models shift. Solutions should easily adapt to bundled payments, value-based care, and new payer contracts. Patient-centered billing processes and engagement strategies, such as transparent statements and payment plans, support not only financial health but also patient satisfaction.
By prioritizing these practices, healthcare organizations can strengthen their revenue management solutions healthcare and position themselves for sustainable success, no matter how the industry evolves.
Navigating the evolving landscape of healthcare revenue management can feel overwhelming, especially with shifting regulations and growing financial pressures. As we’ve explored, embracing integrated solutions and proven best practices is key to optimizing your workflow and maximizing reimbursements. If you’re curious about how your current processes stack up or where hidden opportunities might exist, why not take the next step? You deserve clarity and peace of mind as you prepare for 2026. Let’s work together to identify strengths and areas for improvement—start by Get Your Free Audit today.

