Did you know that U.S. healthcare providers lose billions each year due to inefficient revenue management? Navigating the revenue cycle process in healthcare is notoriously complex, involving numerous steps and frequent regulatory changes.
For clinics and healthcare organizations, mastering the revenue cycle process in healthcare is essential to maintaining financial stability and operational excellence. Small inefficiencies can lead to major revenue losses, denied claims, and administrative headaches.
This guide will provide a clear, step-by-step approach to optimizing your revenue cycle process in healthcare. You will find best practices, current trends, and actionable tactics tailored for providers.
Here’s what you’ll learn:
- Understanding the revenue cycle
- Key process steps
- The role of technology
- Compliance and risk management
- Essential metrics
- Future trends and innovations
By the end, you’ll be equipped to streamline your workflows and boost your bottom line.
Understanding the Healthcare Revenue Cycle Process
The revenue cycle process in healthcare is the backbone of financial operations for every provider, clinic, and healthcare organization. A clear understanding of this process is essential for maintaining healthy cash flow and long-term sustainability. However, even minor inefficiencies can lead to significant revenue leakage, making it crucial for healthcare businesses to continually optimize each step.
Definition and Importance of the Revenue Cycle
The revenue cycle process in healthcare refers to the series of administrative and clinical steps required to capture, manage, and collect patient service revenue. It begins with patient scheduling and ends when all payments are collected and reconciled. For healthcare organizations, this process directly affects cash flow, profitability, and even patient satisfaction.
Common inefficiencies such as inaccurate data entry, delayed claims submission, or missed eligibility checks can quickly erode revenue. For example, a single coding error may delay reimbursement for weeks. For a deeper look at the process, see this Revenue Cycle Medical Billing Overview.
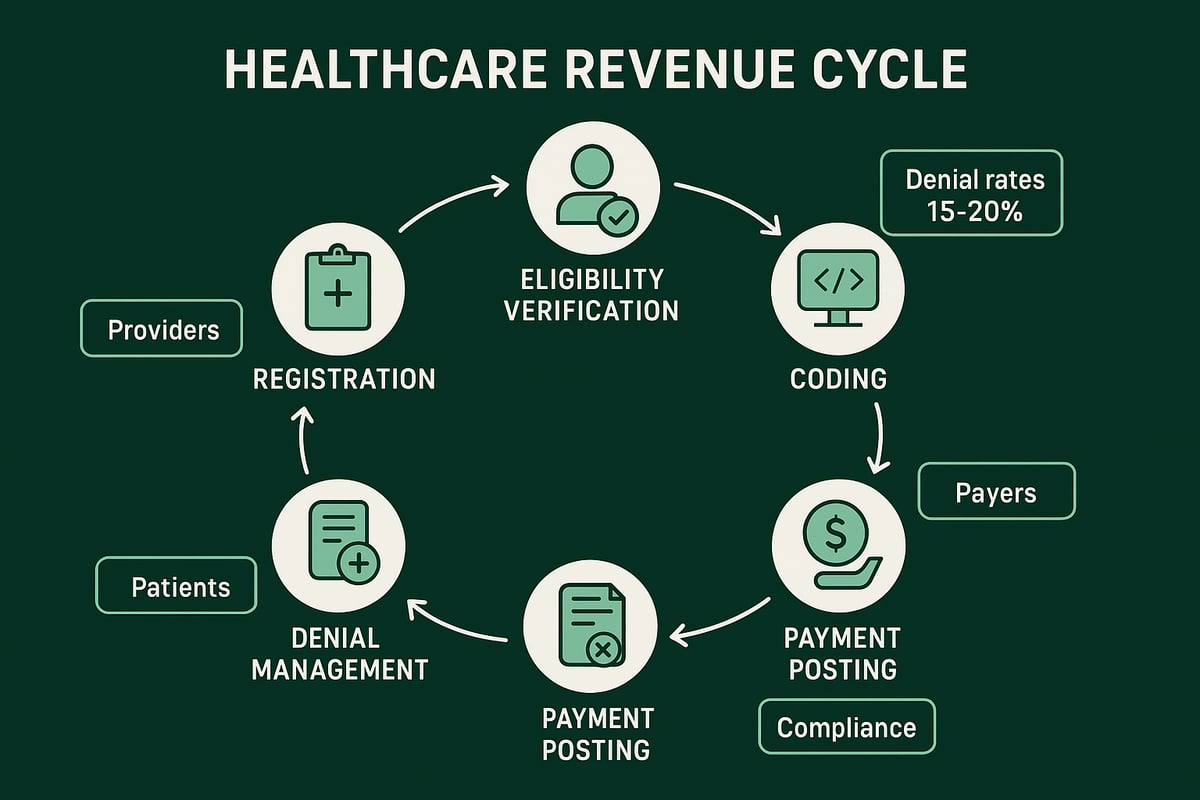
Key Stakeholders and Roles
Effective management of the revenue cycle process in healthcare relies on coordinated efforts among several key stakeholders:
- Providers: Deliver care and document services rendered.
- Billing staff: Translate clinical documentation into billable claims.
- Payers: Insurance companies and government payers that reimburse providers.
- Clearinghouses: Serve as intermediaries between providers and payers for claim submission.
- Patients: Responsible for copays, deductibles, and balances.
Collaboration and timely communication between these groups are critical. If billing staff do not receive accurate clinical information from providers, or if payers are not promptly notified of services, the entire process is at risk for delays or denials.
Common Challenges and Pain Points
The revenue cycle process in healthcare is complex, and several challenges frequently hinder efficiency:
- High rates of claim denials, often due to missing or incorrect information.
- Coding errors, which can lead to compliance risks and lost revenue.
- Delays in insurance eligibility verification, resulting in postponed or rejected claims.
According to industry data, average denial rates can range from 5 to 10 percent, with millions lost annually due to preventable errors. Identifying these pain points early is essential for maintaining financial health.
The Impact of Regulatory Changes
Regulatory updates have a significant impact on the revenue cycle process in healthcare. Changes such as evolving HIPAA requirements, the shift toward value-based care, and new billing guidelines require constant vigilance. Compliance is not optional, as non-adherence can result in fines, audits, or reputational damage.
Organizations must be agile, updating internal processes and training staff as regulations evolve. Staying informed about recent changes is vital for ongoing success and risk mitigation.
Revenue Cycle Management (RCM) Services: A Strategic Solution
Outsourcing RCM services has emerged as a strategic solution for healthcare organizations aiming to optimize the revenue cycle process in healthcare. Professional RCM partners deploy skilled teams and proven workflows to address common pain points, reduce denials, improve collections, and maintain compliance with evolving regulations.
Step-by-Step Breakdown of the Revenue Cycle Process
A streamlined revenue cycle process in healthcare is the foundation of financial success for any provider organization. Each step plays a crucial role in ensuring timely and accurate reimbursement, reducing administrative burden, and supporting operational efficiency. Below, we break down every stage of the revenue cycle process in healthcare, highlighting best practices and common pitfalls to watch for.

1. Patient Scheduling and Registration
The revenue cycle process in healthcare begins the moment a patient schedules an appointment. Capturing accurate demographic and insurance data at this stage is essential. Errors, such as incorrect policy numbers or misspelled names, may seem minor but can lead to claim rejections and payment delays.
A single typo or outdated insurance detail can disrupt the entire revenue cycle process in healthcare. For example, if a patient's registration data does not match payer records, claims are likely to be denied. This step sets the tone for downstream efficiency, making thorough verification and regular staff training vital.
2. Insurance Eligibility Verification and Authorization
Verifying insurance eligibility and securing pre-authorizations are critical steps in the revenue cycle process in healthcare. Failure here is a leading cause of claim denials and lost revenue. Industry statistics show that eligibility issues account for up to 25% of denied claims.
Best practices include using electronic verification tools, confirming coverage in real time, and documenting authorization numbers. For organizations seeking to improve this process, specialized Insurance Eligibility Verification Services can help reduce errors and speed up approvals, ensuring that the revenue cycle process in healthcare moves forward smoothly.
3. Charge Capture and Medical Coding
Accurate charge capture and medical coding are the backbone of the revenue cycle process in healthcare. Providers must document all services rendered and translate them into standardized codes (ICD, CPT, HCPCS) for billing.
Mistakes in coding, such as upcoding, undercoding, or missing modifiers, can result in compliance risks and reimbursement delays. For instance, incorrect coding might trigger payer audits, disrupt cash flow, and even lead to penalties. Consistent audits and coder education are key to maintaining accuracy throughout the revenue cycle process in healthcare.
4. Claims Submission and Processing
Submitting claims promptly and correctly is vital to the revenue cycle process in healthcare. Claims must be reviewed for errors, formatted according to payer requirements, and sent electronically for faster processing.
Clearinghouses can identify discrepancies before claims reach payers, reducing rejection rates. On average, claim rejection rates hover around 5–10%, often due to missing or inaccurate information. Monitoring submission trends and addressing repeated errors helps keep the revenue cycle process in healthcare efficient and effective.
5. Payment Posting and Reconciliation
Once payments are received, accurate posting and reconciliation are essential in the revenue cycle process in healthcare. This involves recording payments, adjustments, and denials, then reconciling them against expected revenue.
Timely posting ensures financial reports reflect reality and allows for prompt follow-up on unpaid balances. Delays at this stage can obscure outstanding receivables, leading to missed revenue opportunities and inaccurate forecasting. A disciplined approach to reconciliation supports the overall health of the revenue cycle process in healthcare.
6. Denial Management and Appeals
Managing denials and appeals is one of the most challenging aspects of the revenue cycle process in healthcare. Identifying root causes, correcting errors, and resubmitting claims are all part of effective denial management.
Best practices include tracking denial trends, prioritizing high-value claims, and maintaining thorough documentation. Industry benchmarks suggest that successful denial resolution rates should exceed 85%. Proactive denial management not only recovers revenue but also highlights areas for process improvement within the revenue cycle process in healthcare.
7. Patient Billing and Collections
The final stage of the revenue cycle process in healthcare involves billing patients and collecting balances. Clear communication of patient responsibilities, flexible payment plans, and convenient payment options are essential for maximizing collections.
A positive experience at this stage not only drives revenue but also enhances patient satisfaction and loyalty. Practices that prioritize transparency and support in patient billing are more likely to see improved financial outcomes.
The Role of Technology and Automation in Revenue Cycle Management
Technology is transforming the revenue cycle process in healthcare, offering providers new ways to streamline operations and improve financial outcomes. As healthcare organizations face mounting complexity, digital tools and automation have become essential for maintaining accuracy, efficiency, and compliance.

Adoption of RCM Software and Digital Tools
Healthcare providers increasingly rely on RCM software and digital platforms to manage the revenue cycle process in healthcare. These tools integrate with electronic health records (EHRs), automate billing workflows, and enhance data accuracy.
By using industry-standard platforms, RCM service teams can adapt to client-owned systems, ensuring seamless collaboration. The benefits are clear:
- Faster claim processing
- Fewer manual errors
- Scalable solutions to support growth
As the revenue cycle process in healthcare evolves, having robust digital tools is now a requirement, not a luxury.
Automation of Key Processes
Automation is revolutionizing the revenue cycle process in healthcare by reducing manual tasks and improving consistency. Processes like eligibility verification, coding assistance, and claim scrubbing are now commonly automated, resulting in fewer delays and denials.
For example, practices using automated eligibility checks report higher clean claim rates and lower administrative overhead. According to AI and Automation in Revenue Cycle Management, automation trends are driving measurable improvements across the industry.
Leveraging automation enables RCM professionals to focus on complex cases, ultimately optimizing the revenue cycle process in healthcare.
Data Analytics and Revenue Cycle Optimization
Data analytics play a critical role in the revenue cycle process in healthcare. Dashboards and real-time reports help providers monitor KPIs, such as collection rates and denial trends.
By analyzing this data, organizations can:
- Identify bottlenecks quickly
- Make informed decisions to enhance collections
- Track performance against benchmarks
A data-driven approach allows continuous optimization of the revenue cycle process in healthcare, directly impacting cash flow and financial health.
Interoperability and Integration Challenges
Despite advancements, connecting disparate systems remains a challenge in the revenue cycle process in healthcare. EHRs, billing software, and payer portals often lack seamless integration, leading to information silos.
To address these issues, providers and RCM partners prioritize:
- Open standards for data exchange
- Regular system audits
- Staff training on integration workflows
Overcoming integration hurdles ensures the revenue cycle process in healthcare remains efficient and responsive to change.
Cybersecurity and Data Privacy
Protecting sensitive data is vital in the revenue cycle process in healthcare. Compliance with HIPAA and other regulations requires robust security protocols, encryption, and regular risk assessments.
RCM service providers maintain strict data privacy controls, safeguarding both patient and financial information. Proactive security measures build trust and help avoid costly breaches.
As digital adoption grows, cybersecurity remains a top priority throughout the revenue cycle process in healthcare.
Compliance, Risk Management, and Regulatory Considerations
Navigating the compliance landscape is crucial for any organization involved in the revenue cycle process in healthcare. Regulatory demands are evolving, and proactive risk management is essential to protect both revenue and reputation. By focusing on regulatory frameworks, fraud prevention, documentation, and staff education, providers can ensure sustainable financial success.

Regulatory Frameworks Impacting Revenue Cycle
The revenue cycle process in healthcare is governed by strict regulatory frameworks. HIPAA, the Affordable Care Act, and payer-specific rules shape how organizations handle patient data, claims, and billing. Non-compliance can result in financial penalties, legal action, or even exclusion from payer networks.
Providers must stay current with updates to regulations. For instance, evolving value-based care models demand new billing practices and documentation standards. Regular compliance audits and risk assessments help healthcare organizations identify and address gaps in their revenue cycle process in healthcare.
Fraud Prevention and Audit Readiness
Fraud prevention is a core responsibility for any team managing the revenue cycle process in healthcare. Common red flags include unusual billing patterns, duplicate claims, and inconsistent coding. Being audit-ready means having robust internal controls and clearly documented processes.
To strengthen audit preparedness, organizations should track denial trends and regularly review claim submissions for accuracy. Partnering with experts or leveraging resources like Denial Management in Medical Billing can help reduce compliance risks and improve audit outcomes. Effective fraud prevention not only protects revenue but also builds payer trust and reduces operational disruptions.
Documentation and Recordkeeping Best Practices
Accurate documentation is the backbone of compliance in the revenue cycle process in healthcare. Every patient encounter, service provided, and billing code must be thoroughly documented to support claims and defend against audits or denials.
Best practices include standardized forms, secure electronic recordkeeping, and regular data quality reviews. Maintaining comprehensive records streamlines appeals and ensures that providers meet regulatory requirements. Proper documentation also supports transparent communication among all stakeholders involved in the revenue cycle process in healthcare.
Staff Training and Ongoing Education
Continuous education is vital for teams engaged in the revenue cycle process in healthcare. Coding rules, payer requirements, and regulatory standards change frequently. Regular training sessions help staff stay updated and reduce costly errors.
Well-trained employees are more adept at identifying compliance risks and implementing best practices. Investing in education not only minimizes mistakes but also strengthens the organization’s reputation for reliability and compliance. Forward-thinking providers make ongoing training a key part of their risk management strategy.
Key Metrics and Performance Indicators in Revenue Cycle Management
Understanding and tracking the right metrics is essential to mastering the revenue cycle process in healthcare. Key performance indicators (KPIs) provide a clear picture of financial health, operational efficiency, and areas for improvement. By focusing on these metrics, healthcare organizations can ensure a steady cash flow and proactively address potential issues before they impact the bottom line.
Essential Revenue Cycle KPIs
Several KPIs are fundamental to monitoring the revenue cycle process in healthcare. These include Days in Accounts Receivable (A/R), Clean Claim Rate, Denial Rate, and Collection Rate. Each metric highlights a specific aspect of financial performance and operational workflow.
| KPI | Definition | Benchmark |
|---|---|---|
| Days in A/R | Average days to collect payment | < 40 days |
| Clean Claim Rate | Claims paid without edits or rejections | > 90% |
| Denial Rate | Percentage of claims denied | < 5-10% |
| Collection Rate | % of billed amount collected | > 95% |
Tracking these KPIs regularly allows providers to spot trends, identify bottlenecks, and make informed decisions about the revenue cycle process in healthcare.
Analyzing and Improving Financial Performance
KPIs are not just for reporting—they are tools for driving improvement. By analyzing metrics, teams can uncover inefficiencies in the revenue cycle process in healthcare, such as delays in payment posting or high denial rates. Addressing these issues quickly leads to better cash flow and reduced write-offs.
For example, a spike in Days in A/R may signal a need for more timely claim follow-up. Leveraging Healthcare Revenue Cycle Analytics enables organizations to visualize trends, drill down into root causes, and implement targeted strategies that enhance overall performance.
Continuous analysis ensures that every stage of the revenue cycle process in healthcare is operating at peak efficiency, supporting long-term financial sustainability.
Benchmarking Against Industry Standards
Comparing KPIs to industry benchmarks is critical for measuring the effectiveness of the revenue cycle process in healthcare. External benchmarks provide context, revealing whether a practice is ahead of the curve or trailing peers.
Healthcare organizations can utilize market research and published reports to compare their metrics to national averages. For instance, the Healthcare Revenue Cycle Management Market Growth Projections highlight the increasing importance of efficient revenue cycle operations as the industry expands.
Regular benchmarking motivates teams to set realistic goals, prioritize improvements, and demonstrate value to stakeholders.
Continuous Process Improvement
Ongoing process improvement is vital to maintaining a healthy revenue cycle process in healthcare. Regular reviews of KPIs, combined with audits and process mapping, help identify gaps and opportunities for optimization.
Teams should establish a routine for evaluating workflow, updating policies, and integrating feedback from staff. Fostering a culture of continuous improvement ensures that best practices evolve alongside regulatory changes and market dynamics.
By committing to ongoing optimization, healthcare organizations strengthen their revenue cycle process in healthcare and secure financial resilience for the future.
Future Trends and Innovations in Revenue Cycle Process
The revenue cycle process in healthcare is evolving rapidly due to regulatory, technological, and market forces. Staying ahead requires providers to adapt to emerging trends that are reshaping the industry. Let us explore the most impactful innovations and what they mean for your organization.
Value-Based Care and Alternative Payment Models
A key shift in the revenue cycle process in healthcare is the move from fee-for-service to value-based care and alternative payment models. These models reward providers for quality and outcomes, rather than volume of services. This transition brings both opportunities and challenges.
Healthcare organizations must adapt their revenue cycle workflows to accommodate bundled payments, shared savings, and performance-based contracts. This often requires new documentation standards, quality reporting, and collaboration across care teams.
By aligning incentives, value-based models can improve patient outcomes and reduce costs. However, they also introduce complexity into billing, coding, and reimbursement. Proactive organizations are investing in analytics and process redesign to stay competitive as these models become more prevalent.
Artificial Intelligence and Predictive Analytics
Artificial intelligence and predictive analytics are transforming the revenue cycle process in healthcare. AI-powered tools help automate tasks such as coding, claim scrubbing, and denial prediction. Predictive models can identify claims at risk of denial, allowing staff to intervene early and prevent revenue loss.
According to Key Revenue Cycle Management Trends 2025, leading providers are leveraging AI to streamline workflows and boost efficiency. These technologies can analyze large volumes of data in real time, uncovering patterns and opportunities for optimization.
As AI adoption grows, healthcare organizations will see fewer manual errors, faster reimbursement, and improved decision-making throughout the revenue cycle process in healthcare.
Patient Financial Engagement and Transparency
Patients are increasingly demanding transparency and convenience in their financial interactions. This trend is reshaping the revenue cycle process in healthcare, prompting providers to offer upfront cost estimates, digital billing, and flexible payment options.
Empowering patients with clear, accurate information improves satisfaction and increases the likelihood of timely collections. Features like online payment portals, text reminders, and self-service tools are now standard for forward-thinking practices.
By prioritizing patient engagement, organizations can reduce bad debt, improve cash flow, and foster loyalty. These changes also align with regulatory initiatives focused on price transparency and consumer rights in healthcare.
Outsourcing and RCM Partnerships
Many healthcare organizations are turning to specialized RCM partners to navigate the complexities of the revenue cycle process in healthcare. Outsourcing allows providers to access deep expertise, advanced technology, and scalable solutions without the burden of managing these resources in-house.
According to Healthcare Revenue Cycle Management Market Analysis, the demand for RCM services continues to grow as practices seek operational efficiency and cost control. Key benefits include faster claims processing, reduced denials, and improved compliance.
When selecting an RCM partner, it is critical to consider experience, adaptability to existing systems, and a proven track record of results. Strong partnerships can drive sustainable improvements and support long-term financial health.
As you’ve seen throughout this guide, mastering the revenue cycle process is key to your practice’s financial health and long term success. From accurate eligibility checks to effective denial management, every step counts—and having the right partner can make all the difference. If you’re ready to pinpoint hidden inefficiencies or want expert insights tailored to your unique operation, why not take the next step? You deserve clarity, confidence, and results that support your goals. Let’s work together to elevate your revenue cycle—Get Your Free Audit and discover how streamlined processes can transform your financial performance.