Confused by the claim reimbursement process? You are not alone. Many healthcare professionals find themselves overwhelmed by the paperwork, regulations, and timelines that come with insurance claims.
For clinics and providers, an efficient claim reimbursement process is not just about getting paid; it is essential for maintaining steady cash flow and ensuring operational stability. Errors or delays can lead to compliance risks and dissatisfied patients.
Mastering the claim reimbursement process can transform your organization’s financial health, boost compliance, and elevate patient satisfaction. This guide will walk you through every step, from understanding how reimbursement works to overcoming common challenges and adopting best practices.
Ready to navigate with confidence? Explore key concepts, actionable steps, expert strategies, and future trends in claim reimbursement throughout this comprehensive guide.
Understanding the Claim Reimbursement Process
Navigating the claim reimbursement process is essential for healthcare organizations seeking financial health and operational efficiency. This section unpacks what claim reimbursement means, why it matters, who is involved, the various models in play, and the foundational terminology every provider should know.
What is Claim Reimbursement?
The claim reimbursement process is a core component of the healthcare revenue cycle. It ensures providers receive payment for services rendered to insured patients. Unlike direct payment, where patients pay out-of-pocket, reimbursement involves submitting claims to insurance payers for approval and payment.
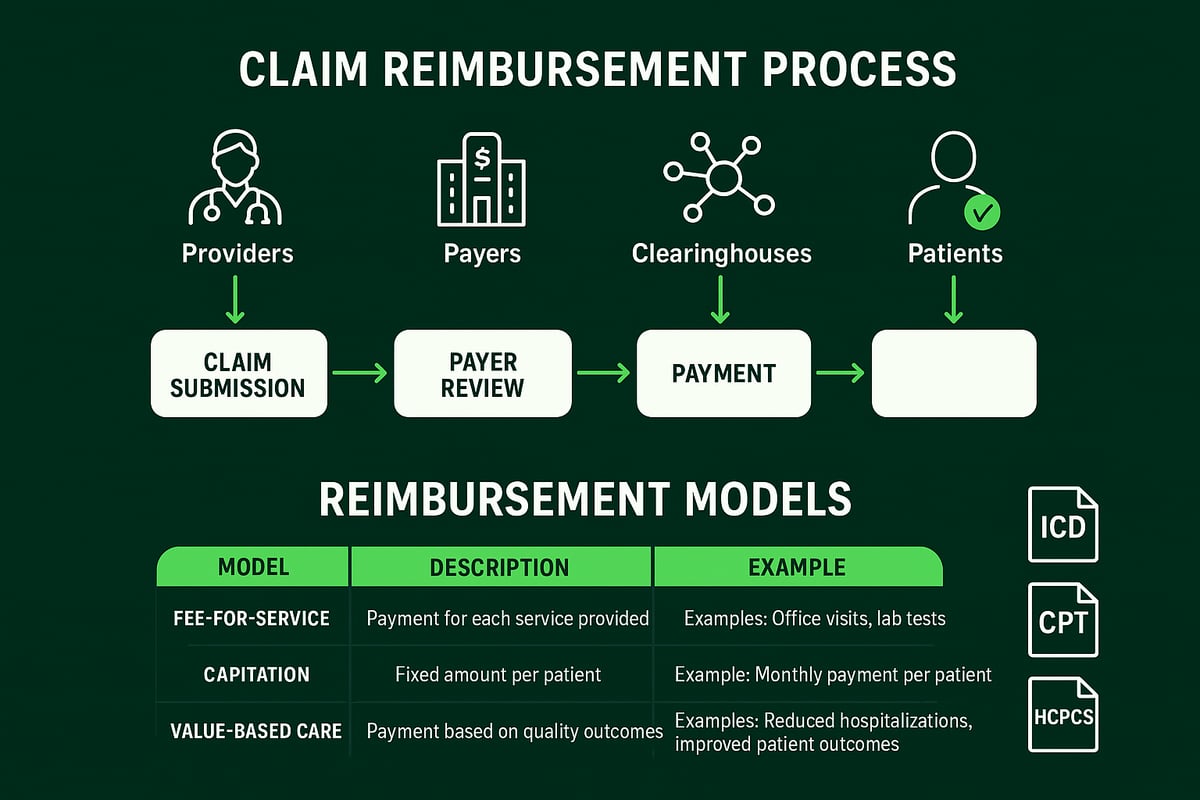
There are several types of claims, including medical, dental, and pharmacy. For example, an outpatient procedure like a minor surgery would require a detailed claim submission to the payer. The key stakeholders in the claim reimbursement process are providers (hospitals, clinics), payers (insurance companies), and patients. A comprehensive understanding of this process is vital for maintaining steady cash flow. For a broader overview, see the Revenue Cycle Process in Healthcare.
Why Reimbursement is Critical for Healthcare Organizations
A successful claim reimbursement process directly impacts a healthcare organization’s financial stability and operational sustainability. Industry reports reveal that up to 20% of claims are initially denied, highlighting the importance of accuracy and timeliness. Delayed or denied claims can create serious cash flow challenges, especially for smaller practices that may rely on steady reimbursement to cover daily expenses.
Regulatory compliance is another critical factor. Failing to adhere to payer guidelines or documentation standards increases audit risk and potential penalties. For example, a small clinic experiencing a backlog of denied claims might find it difficult to pay staff or invest in new equipment, underscoring the process’s central role.
Key Players in the Reimbursement Ecosystem
Multiple parties collaborate throughout the claim reimbursement process. Providers deliver care and generate claims, while payers review and adjudicate those claims. Clearinghouses act as intermediaries, ensuring claims meet formatting and data standards before reaching payers. Accurate data exchange among these players is essential for timely reimbursement.
Billing teams within provider organizations coordinate closely with payers to resolve discrepancies and manage denials. Third-party administrators, often engaged by self-insured employers, add another layer of complexity by overseeing benefits and claims processing. Each stakeholder has a unique role in ensuring claims move smoothly through the pipeline.
Types of Reimbursement Models
Healthcare organizations encounter several reimbursement models within the claim reimbursement process. The most common are fee-for-service, capitation, and value-based care.
-
Fee-for-service pays providers for each service delivered, offering straightforward billing but incentivizing volume.
-
Capitation pays a set amount per patient, regardless of services used, which may control costs but can limit care flexibility.
-
Value-based care rewards providers for quality and outcomes rather than quantity, aligning incentives with patient health.
Trends show a gradual shift toward value-based models, as payers and regulators seek to improve care quality while controlling costs. For example, many clinics now participate in bundled payment arrangements for specific procedures.
|
Model |
Payment Basis |
Pros |
Cons |
|---|---|---|---|
|
Fee-for-Service |
Per service |
Simple, transparent |
May drive unnecessary care |
|
Capitation |
Per patient |
Predictable revenue |
Risk of under-service |
|
Value-Based Care |
Outcomes/Quality |
Aligns with better results |
Complex to implement |
Foundational Terminology and Codes
Mastering the claim reimbursement process requires familiarity with essential coding systems and terminology. The most common codes include ICD (International Classification of Diseases), CPT (Current Procedural Terminology), and HCPCS (Healthcare Common Procedure Coding System). Accurate coding ensures claims are processed correctly and paid promptly.
For instance, a simple coding error, such as entering an outdated ICD code, can lead to claim denials and delayed payments. Providers should maintain updated coding resources and train staff regularly. Below is a glossary of key terms:
-
ICD Codes: Identify medical diagnoses.
-
CPT Codes: Describe medical procedures.
-
HCPCS Codes: Cover supplies, equipment, and non-physician services.
-
Remittance Advice: Document from payer detailing payment decisions.
Understanding and using these codes accurately is foundational to a successful claim reimbursement process.
Step-by-Step Guide to the Claim Reimbursement Process
Navigating the claim reimbursement process requires precision, collaboration, and attention to detail at every stage. Each step builds on the previous one, ensuring claims progress smoothly from patient intake to final payment. By mastering each phase, healthcare organizations can protect cash flow, maintain compliance, and improve patient satisfaction.
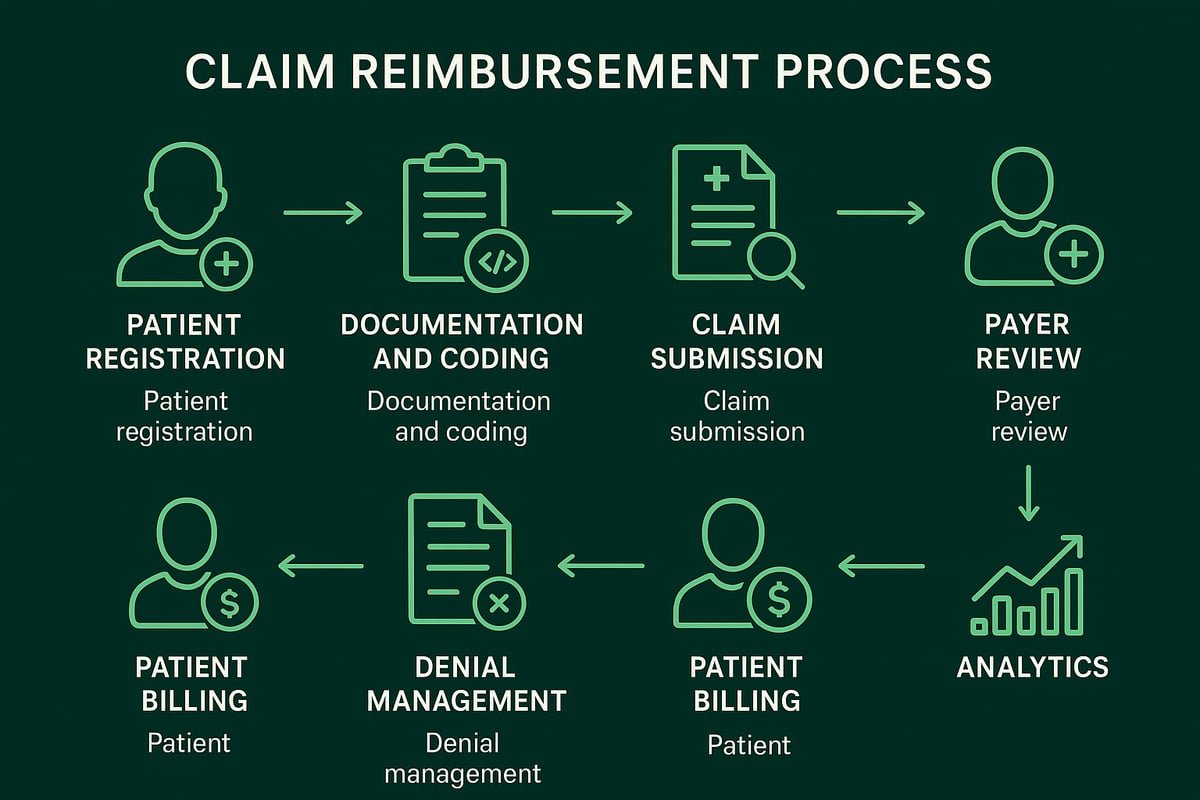
Step 1: Patient Registration and Insurance Verification
The claim reimbursement process begins with accurate patient registration and insurance verification. Front-desk teams collect demographic information, verify insurance coverage, and confirm eligibility before services are rendered. This step is critical because missing or incorrect data can lead to claim denials or payment delays.
Healthcare providers must use verification tools to check active coverage and determine patient benefits. For example, verifying eligibility prevents issues when a patient’s insurance is inactive. Best practices include double-checking details and using electronic eligibility systems. Thorough verification at this stage sets a solid foundation for the entire claim reimbursement process.
Step 2: Service Documentation and Coding
Comprehensive documentation and precise coding are essential in the claim reimbursement process. Clinical staff must document every service, diagnosis, and procedure provided. Coders then assign appropriate ICD, CPT, or HCPCS codes that match the documentation.
Accurate coding ensures compliance and reduces the risk of denials. Missteps like upcoding or insufficient documentation can trigger audits or payment recoupments. For instance, a mismatch between services documented and codes assigned may result in a denied claim. Consistent alignment between documentation and coding supports a smooth claim reimbursement process.
Step 3: Claim Creation and Submission
Once documentation and coding are complete, the next phase in the claim reimbursement process is claim creation and submission. Billing teams prepare clean claims—those free of errors or omissions—using either paper or electronic formats. Most providers prefer electronic claims due to speed and accuracy.
Clearinghouses play a key role by scrubbing claims for errors before forwarding them to payers. Common submission mistakes include missing information or inaccurate codes. Submitting a clean claim increases the chance of prompt reimbursement, as outlined in the Clean Claim in Medical Billing resource. This step is vital to the overall claim reimbursement process.
Step 4: Payer Review and Adjudication
After submission, payers review each claim in the claim reimbursement process for accuracy, eligibility, and medical necessity. Claims undergo edits, audits, and checks against payer policies. The adjudication process determines if a claim is approved, partially paid, or denied.
For example, a claim may be denied if the payer deems the service not medically necessary. Providers must monitor adjudication outcomes closely and be prepared to respond to requests for additional information. Understanding payer requirements is essential for a successful claim reimbursement process.
Step 5: Payment Posting and Reconciliation
When payments arrive, the claim reimbursement process continues with payment posting and reconciliation. Payments are posted to patient accounts, and remittance advice (ERA or EOB) is reviewed for accuracy. This step identifies underpayments, overpayments, or discrepancies.
Billing teams must reconcile payments with claim details and resolve any mismatches. For instance, if a claim is paid less than expected, teams investigate the reason and take corrective action. Accurate payment posting ensures financial transparency and keeps the claim reimbursement process on track.
Step 6: Denial Management and Appeals
Denials are an inevitable part of the claim reimbursement process. Common reasons include coding errors, missing documentation, or lack of prior authorization. Effective denial management involves identifying denial causes, correcting errors, and submitting timely appeals.
Teams must gather supporting documentation and follow payer-specific appeal processes. For example, a successful appeal may overturn a medical necessity denial, resulting in payment. Proactive denial management is crucial for optimizing the claim reimbursement process and protecting revenue.
Step 7: Patient Billing and Collections
The claim reimbursement process also includes communicating patient financial responsibility. Once payer payments are posted, patients are billed for any remaining balances, such as deductibles or coinsurance. Clear, understandable statements and flexible payment plans improve collections.
Managing outstanding balances is essential for cash flow. For example, offering online payment options can reduce patient bad debt. Transparent communication and streamlined billing help ensure patients fulfill their obligations, supporting the overall claim reimbursement process.
Step 8: Reporting and Analytics
The final step in the claim reimbursement process is robust reporting and analytics. Monitoring key performance indicators (KPIs) such as days in accounts receivable, denial rates, and first-pass resolution rates highlights process strengths and weaknesses.
Using analytics tools, organizations can identify bottlenecks and implement targeted improvements. For instance, tracking denial trends enables proactive adjustments in documentation or coding. Data-driven decisions help optimize the claim reimbursement process, ensuring continuous financial and operational improvement.
Common Challenges and How to Overcome Them
Healthcare organizations encounter several obstacles as they navigate the claim reimbursement process. Addressing these challenges proactively is crucial for maintaining financial health, regulatory compliance, and operational efficiency. Below, we break down the most common hurdles and provide actionable strategies for overcoming them.
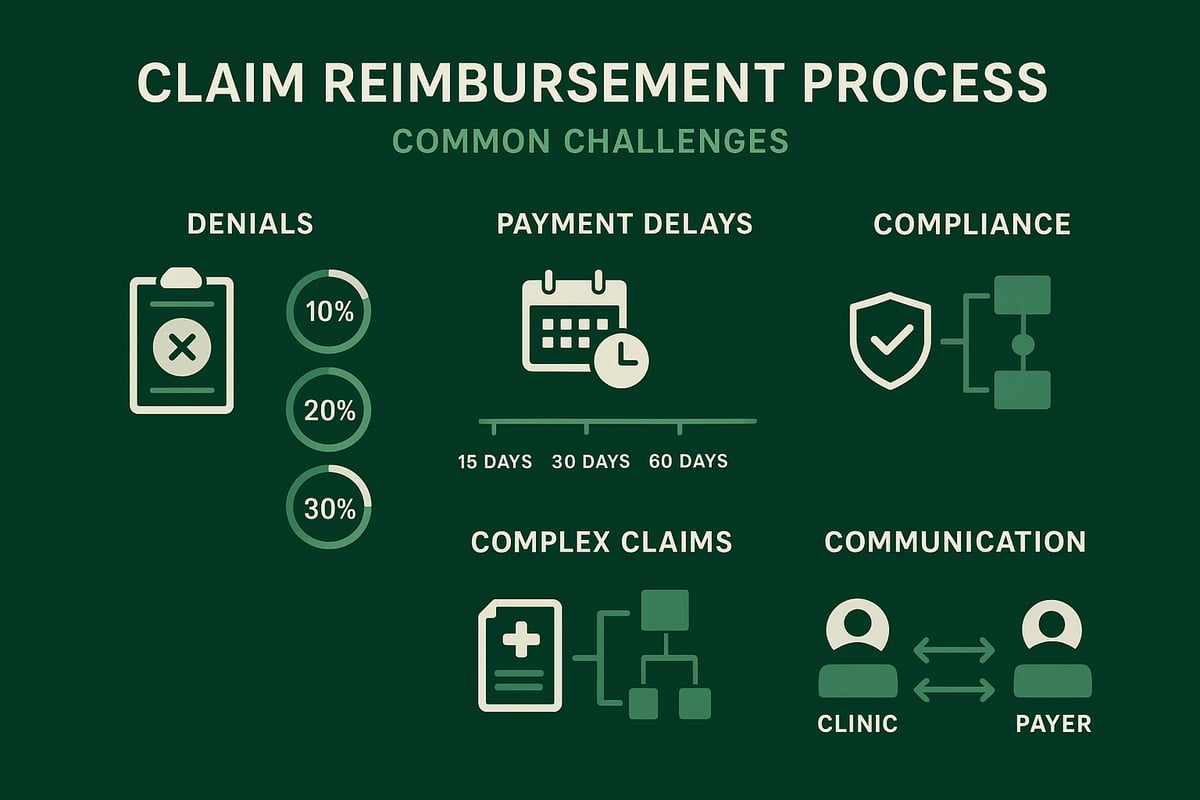
Frequent Causes of Claim Denials
Claim denials are a persistent issue within the claim reimbursement process, often leading to revenue loss and increased administrative burden. The most frequent causes include incomplete or incorrect patient information, coding errors, missing prior authorizations, and lack of supporting documentation. In fact, industry data shows that the top five denial reasons stem from these avoidable mistakes.
|
Top Denial Reason |
Percentage (%) |
|---|---|
|
Inaccurate Patient Info |
28 |
|
Coding Errors |
25 |
|
Missing Authorization |
18 |
|
Late Submission |
15 |
|
Insufficient Documentation |
14 |
To address denials effectively, healthcare providers should invest in staff training, implement pre-bill audits, and leverage denial management expertise. For a deeper dive into strategies, see Denial Management in Medical Billing, which outlines proven solutions for reducing denials within the claim reimbursement process.
Delays in Payment Processing
Delays in the claim reimbursement process can significantly disrupt cash flow, especially for smaller practices. Common causes include slow payer processing, missing documentation, and untimely claim submissions. These bottlenecks can result in extended accounts receivable cycles and increased financial strain.
To minimize delays, ensure that claims are submitted promptly and accurately. Establish a systematic follow-up protocol for outstanding claims and maintain open communication with payers to resolve discrepancies quickly. Regular monitoring of payment timelines helps organizations identify and address recurring issues in their claim reimbursement process.
Compliance and Regulatory Hurdles
Compliance is a critical component of the claim reimbursement process, as healthcare organizations must adhere to HIPAA, state-specific regulations, and payer policies. Non-compliance can lead to financial penalties, audits, and reputational damage.
Staying current with regulatory changes is essential. Assign dedicated compliance officers or partner with RCM experts who monitor updates and implement necessary adjustments. Conduct regular audits to identify areas of risk and ensure that claims data is managed securely and in accordance with all legal requirements within the claim reimbursement process.
Managing High Volumes and Complex Claims
Large clinics and multi-specialty practices often face high claim volumes and complex billing scenarios. Laboratory, behavioral health, and specialty care claims can introduce additional layers of complexity to the claim reimbursement process.
Scalable workflows and skilled professionals are vital. Standardize procedures for handling complex claims, cross-train staff, and utilize technology for batch processing and error detection. Outsourcing to experienced RCM service providers can also help organizations handle surges in claim volume and maintain accuracy throughout the claim reimbursement process.
Effective Communication with Payers and Patients
Clear, timely communication is essential for resolving issues and improving outcomes in the claim reimbursement process. Misunderstandings with payers or patients can escalate disputes and delay payments.
Adopt a structured communication protocol, using templates for payer correspondence and patient notifications. Leverage secure messaging platforms to ensure quick, documented exchanges. Proactive engagement, such as confirming receipt of claims and clarifying patient responsibilities, can significantly reduce friction and improve the overall efficiency of the claim reimbursement process.
Best Practices for Maximizing Reimbursements
Healthcare organizations aiming to master the claim reimbursement process must focus on proven strategies to optimize revenue and minimize denials. Below, we outline best practices that help clinics and providers achieve consistent, compliant, and efficient claim reimbursement outcomes.
Ensuring Accurate and Complete Documentation
Accurate documentation is the backbone of a successful claim reimbursement process. Every service provided must be thoroughly recorded, with attention to clinical details and patient information. Incomplete or vague records often result in costly delays or denials.
-
Train staff regularly on documentation standards.
-
Conduct internal audits to catch discrepancies early.
-
Use checklists to ensure all required elements are captured.
A small clinic implemented routine audits and saw a measurable reduction in denials. This demonstrates how the claim reimbursement process benefits from ongoing documentation improvements.
Optimizing Coding and Charge Capture
Proper coding ensures that services are billed correctly and reimbursed at appropriate rates. The claim reimbursement process relies on skilled coders who assign ICD, CPT, and HCPCS codes that accurately reflect the care delivered.
-
Invest in coder education and certification.
-
Leverage up-to-date coding manuals and resources.
-
Align documentation with coding to avoid mismatches.
One group practice improved reimbursement rates by refining its coding workflows, highlighting the direct impact accurate coding has on the claim reimbursement process.
Proactive Denial Prevention Strategies
Denial prevention is essential for a smooth claim reimbursement process. Identifying and addressing root causes of denials before submission saves time and preserves cash flow.
-
Analyze denial trends to spot recurring issues.
-
Implement pre-bill edits and validation checks.
-
Use real-time dashboards to monitor denial rates.
A clinic that adopted pre-submission audits lowered its denial rate by 10 percent, demonstrating the value of proactive measures within the claim reimbursement process.
Leveraging Technology and Industry Expertise
Automation and industry expertise can dramatically streamline the claim reimbursement process. Electronic claim submission, automated edits, and EFT adoption are changing the landscape.
-
Automate repetitive tasks to reduce manual errors.
-
Partner with RCM experts who understand payer requirements.
-
Stay informed about trends like the rise of EFT healthcare claim payments for faster, more secure reimbursements.
Organizations that embraced automation and expert support reported reduced A/R days and improved claim reimbursement process efficiency.
Staff Training and Continuous Education
Continuous staff training is vital to keep up with the evolving claim reimbursement process. Payer rules, coding standards, and compliance requirements are always changing.
-
Schedule regular training sessions for billing and coding teams.
-
Share updates on payer policies and industry best practices.
-
Foster a culture of learning and accountability.
A clinic enhanced its first-pass acceptance rate by prioritizing ongoing education in the claim reimbursement process, reducing costly rework and delays.
Greenhive Billing Solutions: Expert Support for Efficient Claim Reimbursement
Greenhive offers tailored RCM services that help healthcare providers maximize every step of the claim reimbursement process. Our experienced team manages billing, coding, and denial prevention with an emphasis on compliance and transparency.
By leveraging data-driven insights and adapting to client-owned software, Greenhive enables practices to achieve faster payments and fewer denials. One client saw a dramatic improvement in cash flow and claim reimbursement process outcomes after partnering with our experts.
Future Trends in Claim Reimbursement
The healthcare landscape is rapidly evolving, and the claim reimbursement process is at the center of these changes. Staying ahead of trends is essential for healthcare organizations that want to optimize revenue, remain compliant, and deliver a positive patient experience. Let’s explore what the future holds for claim reimbursement.
Evolving Payer Policies and Reimbursement Models
Payer policies are shifting, and reimbursement models are becoming more complex. The claim reimbursement process will be impacted by the continued transition from fee-for-service to value-based care and bundled payments. Healthcare organizations must adapt to new payer requirements, such as expanded quality metrics and care coordination expectations.
Recent updates, such as those detailed in CMS Finalizes 2026 Medicare Reimbursement Policies, demonstrate the focus on telehealth, chronic disease management, and digital health. B2B partners must stay agile to respond to these changing rules and ensure claims are processed efficiently.
Advances in Automation and AI
Automation and AI are revolutionizing the claim reimbursement process. AI-driven tools can identify claim errors, predict denials, and accelerate claim scrubbing, reducing manual workloads for billing teams. Automation streamlines repetitive tasks such as eligibility verification, coding checks, and claims submission.
Healthcare organizations benefit from faster turnaround times and improved accuracy. By leveraging these technologies, B2B service providers can deliver measurable improvements in claim approval rates and reduce administrative costs, creating a more efficient revenue cycle.
Increasing Focus on Patient Financial Responsibility
High-deductible health plans and rising out-of-pocket costs are shifting more financial responsibility onto patients. This trend directly affects the claim reimbursement process, as organizations must clearly communicate balances, offer flexible payment options, and proactively manage collections.
B2B billing partners play a key role in designing patient-friendly statements and payment plans. Using data-driven insights, organizations can increase patient satisfaction while minimizing bad debt. Adapting to this shift is essential for maintaining healthy cash flow in today’s environment.
Regulatory Changes and Compliance Demands
Regulatory requirements are evolving, and compliance is more critical than ever within the claim reimbursement process. Updates to HIPAA, CMS guidelines, and state laws require healthcare organizations to stay vigilant. Non-compliance can lead to audits, penalties, and reputational risk.
B2B service providers must monitor changes and ensure all claims data is handled securely and accurately. Preparing for new interoperability standards and privacy mandates helps organizations avoid disruptions and maintain trust with payers and patients.
Data Analytics and Real-Time Reporting
Data analytics is transforming the claim reimbursement process by providing actionable insights. Real-time dashboards and KPI tracking allow organizations to identify trends, monitor denial rates, and optimize revenue cycle performance.
According to the Healthcare Claims Management Market Forecast, the demand for digitalization and efficiency is driving market growth. B2B RCM providers harness analytics for continuous process improvement, giving healthcare clients a competitive edge.
After exploring the ins and outs of the claim reimbursement process—from accurate coding to overcoming denials, you might be wondering how your practice measures up and where you can improve. That’s where expert insight becomes invaluable. At Greenhive Billing Solutions, we’re dedicated to helping healthcare providers like you maximize reimbursements, reduce errors, and streamline every step of your revenue cycle. If you’re ready to see where your current processes stand and discover actionable ways to boost your financial performance, let’s take the next step together.
Claim Billing Free Audit

