Healthcare organizations in 2026 face rising denial rates and increasing administrative costs, making clean claim in medical billing more vital than ever for revenue and operational efficiency. Inaccurate or incomplete claims can significantly delay payments and disrupt cash flow, putting financial stability at risk.
This essential guide is designed for healthcare professionals seeking a comprehensive, up-to-date resource on how to achieve and maintain clean claims. You will learn the core definition, understand why clean claims matter, identify common errors, follow a step-by-step process for submission, discover proven strategies to boost clean claim rates, and explore future trends shaping the industry.
Mastering clean claim in medical billing offers measurable benefits for your practice. Read on to optimize your billing processes and secure the financial health of your organization.
Understanding Clean Claims in Medical Billing
Clean claims are the backbone of efficient revenue cycle management. In 2026, the standards for a clean claim in medical billing have become even more stringent as healthcare organizations strive for higher accuracy and compliance. Understanding what constitutes a clean claim and how to ensure every submission meets these requirements is essential for any medical practice seeking to optimize financial performance and reduce costly delays.
Definition and Criteria of a Clean Claim
A clean claim in medical billing is a claim that is complete, accurate, and compliant with payer and regulatory requirements at the time of first submission. For 2026, this means every field is filled in correctly, all codes are current, and every required document is attached.
Essential criteria for a clean claim in medical billing:
- Complete patient and provider information
- Accurate and up-to-date coding (CPT, ICD-10, HCPCS)
- Valid insurance details and eligibility
- Supporting documentation for medical necessity
Industry standards, such as those set by CMS and commercial payers, expect claims to pass all system edits and audits without manual intervention. For example, a claim with all information in place that passes payer edits on the first attempt is a true clean claim in medical billing.
Key Components Required for a Clean Claim
Several core components must be present for a claim to be considered clean. Each piece plays a role in supporting the integrity of the claim and ensuring it processes quickly.
- Verified patient identification and insurance coverage
- Provider credentials, including NPI (National Provider Identifier)
- Accurate CPT, ICD-10, and HCPCS codes that match the services rendered
- Service dates, locations, and any required authorization numbers
- Documentation that clearly demonstrates medical necessity
By ensuring these elements are always included, practices reduce the risk of denials and keep the clean claim in medical billing process efficient.
Common Reasons Claims Fail to Qualify as Clean
Despite best efforts, many claims are rejected or delayed due to avoidable mistakes. Some of the most frequent reasons include:
- Missing or incorrect patient demographic details
- Use of outdated or incorrect codes
- Missing prior authorizations or referral information
- Lack of required supporting documentation
In fact, up to 20 percent of claims are denied or delayed due to such errors, according to industry sources. For a deeper dive into these pitfalls and how to prevent them, review Common errors with medical billing claims.
Regulatory and Payer Requirements in 2026
Regulatory and payer requirements for a clean claim in medical billing have evolved. In 2026, CMS and commercial payers have updated their policies, requiring even greater attention to detail.
Practices must adhere to new HIPAA interoperability mandates, use the latest code sets, and follow payer-specific submission rules. Recent updates to CPT and ICD-10 codes mean billing teams must stay current to avoid rejections. Compliance with these regulations ensures every clean claim in medical billing meets both legal and payer standards.
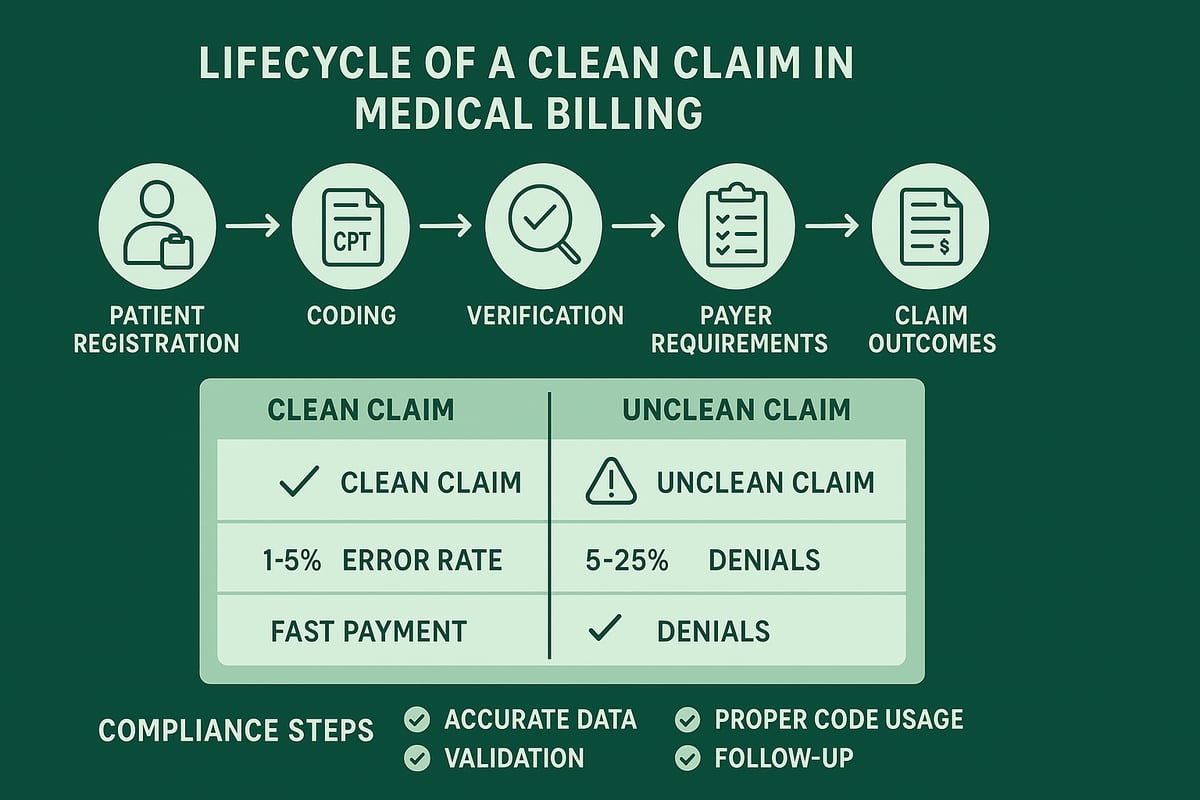
Real-World Example: Clean vs. Unclean Claim
The difference between a clean claim in medical billing and a rejected claim is often clear upon review.
| Aspect | Clean Claim | Unclean Claim |
|---|---|---|
| Patient Data | Complete and accurate | Missing DOB, incomplete address |
| Coding | Current CPT, ICD-10, HCPCS codes | Outdated or mismatched codes |
| Documentation | All required attachments included | Missing medical necessity notes |
| Outcome | Passes on first submission | Rejected, requires rework |
Submitting a clean claim in medical billing the first time saves time, reduces administrative costs, and accelerates reimbursement.
The Business Impact of Clean Claims
Clean claim in medical billing is more than a technical requirement—it is a fundamental driver of financial health and operational efficiency for healthcare organizations. Understanding the ripple effects of clean claims on revenue, compliance, and patient satisfaction is essential for every practice aiming to thrive in 2026.
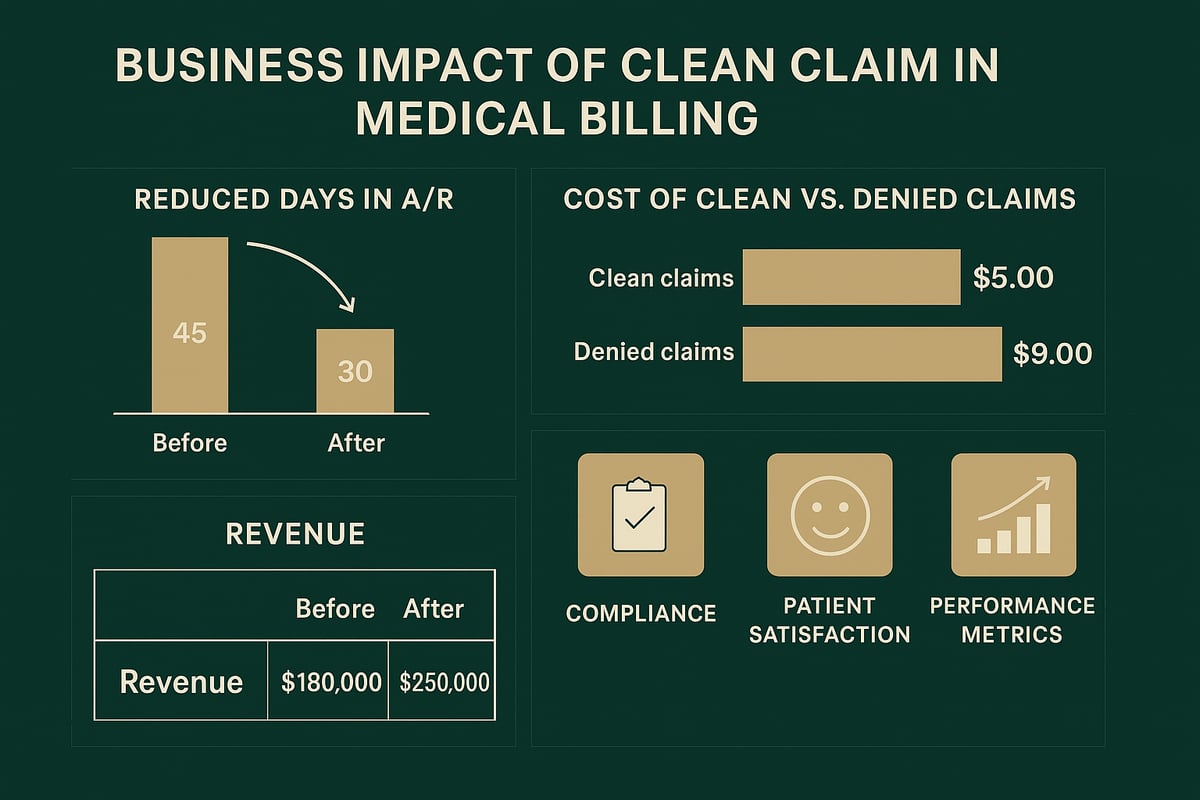
Revenue Cycle Implications
A high clean claim in medical billing rate directly accelerates reimbursements and optimizes cash flow. When claims are submitted cleanly on the first attempt, practices experience fewer payment delays, reducing the average days in accounts receivable (A/R). This efficiency translates into improved financial stability, allowing organizations to forecast revenue with greater confidence.
For example, practices achieving a clean claim in medical billing rate above 95 percent often see payments processed 30 percent faster compared to those with lower rates. This reliability empowers clinics to allocate resources strategically and invest in growth initiatives.
Cost of Denials and Rework
Every denied or rejected claim represents a tangible administrative cost. The average expense to rework a claim ranges from $25 to $30, not including the indirect costs of staff time and delayed revenue. As payer audits and denial rates continue to climb, the importance of submitting a clean claim in medical billing has never been greater. According to recent industry data, the volume of payer denials is rising, emphasizing the need for robust denial prevention strategies (Payer Audits and Denial Amounts Rise in 2025).
Reworking claims also diverts valuable staff resources from patient-facing activities to administrative tasks. Reducing rework through clean claims supports both operational efficiency and bottom-line results.
Effects on Compliance and Audit Risk
A consistently high clean claim in medical billing rate lowers the likelihood of triggering payer audits or regulatory scrutiny. Clean claims are less likely to contain compliance errors that can result in legal exposure or accusations of fraud. By minimizing improper submissions, practices protect themselves from costly investigations and penalties.
Patient Experience and Satisfaction
Submitting a clean claim in medical billing also enhances the patient experience. Accurate billing minimizes confusion, reduces the number of patient complaints, and shortens the time between service and payment resolution. When patients receive clear, correct bills, their satisfaction and trust in the practice increase.
Clean Claim Rate as a Performance Metric
The clean claim rate is a vital performance metric for any healthcare organization. Industry benchmarks recommend maintaining a rate of 95 percent or higher. By closely monitoring this KPI, practices can identify process gaps and measure the effectiveness of their revenue cycle management strategies.
Case Study: Practice Revenue Before and After Clean Claim Optimization
| Metric | Before (85% Clean Claim Rate) | After (97% Clean Claim Rate) |
|---|---|---|
| Average Denial Rate | 15% | 3% |
| Days in A/R | 46 | 32 |
| Collections Increase | – | +15% |
A real-world example: After optimizing their clean claim in medical billing processes, a clinic improved its clean claim rate from 85 percent to 97 percent, leading to a 15 percent increase in collections and significantly faster reimbursements.
Step-by-Step Process for Submitting Clean Claims in 2026
Submitting a clean claim in medical billing is no longer just a routine task—it is a mission-critical process that directly impacts your organization’s financial performance. In 2026, rising payer scrutiny and evolving compliance requirements mean that every detail matters. By mastering each step of the process, healthcare businesses can maximize revenue, minimize denials, and streamline operations for lasting success.
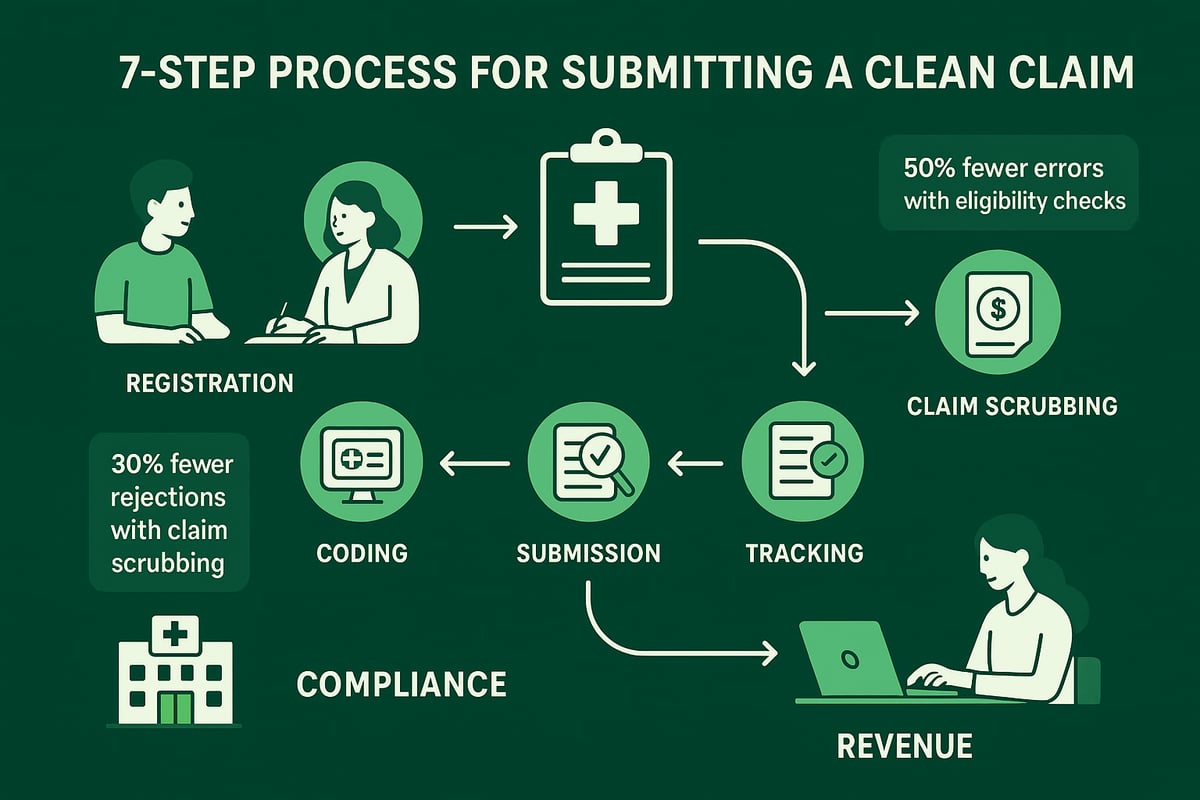
Step 1: Patient Registration and Insurance Eligibility Verification
The first step for a clean claim in medical billing is gathering complete and accurate patient information. Registration teams must confirm the spelling of names, date of birth, and address. Equally important is verifying insurance eligibility before services are rendered.
Electronic verification tools play a significant role here. By integrating real-time eligibility checks into the registration workflow, practices can halve the error rate compared to manual verification. This ensures that the patient’s coverage is active, benefits are confirmed, and any copays or deductibles are identified upfront.
A single missed data point can lead to denials or delayed payments. For B2B medical groups, investing in team training and robust verification protocols is essential to boost clean claim in medical billing rates from the very start.
Step 2: Accurate Medical Coding and Documentation
Coding is the backbone of the clean claim in medical billing process. Assigning the correct CPT, ICD-10, and HCPCS codes ensures that services are billed accurately and that claims reflect medical necessity. Documentation must support every procedure and diagnosis.
Staying current with 2026 coding updates is non-negotiable. Regularly review payer bulletins and update codebooks to avoid using obsolete codes. Encourage providers to document with clarity and completeness, capturing all relevant details.
A best practice is to conduct periodic documentation audits and cross-check codes with clinical notes. This proactive approach helps prevent errors, supports compliance, and raises the percentage of clean claim in medical billing submissions.
Step 3: Charge Entry and Claim Creation
Once coding is complete, accurate charge entry is the next critical step in achieving a clean claim in medical billing. Charges must reflect the actual services rendered, including precise service dates and correct provider credentials.
Double-checking for errors during charge entry is vital. This includes confirming that all modifiers are applied appropriately, the location of service is correct, and any authorization numbers are included when required.
A streamlined charge entry process, supported by experienced RCM professionals, helps minimize data entry mistakes. By adopting checklists and standardized workflows, clinics can ensure every claim meets the criteria for a clean claim in medical billing.
Step 4: Pre-Submission Quality Checks (Claim Scrubbing)
Before submitting any claim, thorough quality checks—commonly known as claim scrubbing—are indispensable for clean claim in medical billing success. Claim scrubbing tools, powered by advanced algorithms or managed by trained staff, identify common issues such as incomplete fields, invalid codes, or missing documentation.
Practices using automated or manual scrubbing see a 30% reduction in claim rejections. These tools validate payer-specific requirements, flag inconsistencies, and prompt corrections before submission.
Quality assurance at this stage saves time, reduces administrative costs, and increases the likelihood of first-pass acceptance. For organizations aiming to optimize clean claim in medical billing rates, embedding scrubbing into daily routines is a proven strategy.
Step 5: Submitting Claims to Clearinghouse/Payer
Proper submission is the turning point for a clean claim in medical billing. In 2026, electronic submission is standard, although some payers may still accept paper claims. Each payer has unique formatting and data requirements, so attention to detail is key.
Utilize clearinghouses to transmit claims securely and to perform one last round of edits. Ensure that all required attachments, such as referral forms or medical records, accompany the claim as needed.
For a comprehensive overview of best practices and how to streamline this step, review our medical claim submission process, which details proven methods for efficient and compliant claim delivery. Consistency in this phase dramatically boosts the rate of clean claim in medical billing approvals.
Step 6: Tracking, Follow-Up, and Managing Rejections
After submission, diligent tracking and prompt follow-up are essential to maintain a high clean claim in medical billing rate. Use real-time dashboards or reporting tools to monitor claim status with each payer.
If a claim is rejected or denied, respond immediately. Quick action allows for timely correction and resubmission within payer deadlines, reducing the risk of lost revenue. Assign responsibility to specific team members for follow-up and establish clear escalation protocols.
A proactive approach to denial management, supported by analytics, ensures that trends are identified and addressed. This step closes the loop and reinforces the cycle of clean claim in medical billing excellence.
Step 7: Payment Posting and Reconciliation
The final step in the clean claim in medical billing process is accurate payment posting and reconciliation. When remittance advice is received, post payments precisely, matching them to the correct claims and service lines.
Reconcile posted payments against expected amounts to quickly spot underpayments or denials. This enables rapid appeals or correction of errors before they impact cash flow.
A well-organized reconciliation process not only secures revenue but also provides valuable feedback for process improvement. Consistent execution at this stage ensures the financial health of your organization and sustains high clean claim in medical billing performance.
Strategies to Improve Clean Claim Rates
Achieving a high clean claim in medical billing rate is a strategic imperative for healthcare organizations in 2026. With payer scrutiny intensifying and operational costs rising, practices must implement robust, repeatable processes to ensure claims are accurate and compliant from the start. Proven strategies for enhancing clean claim rate can help your team master best practices and proactively reduce errors.
Staff Training and Continuing Education
Continuous staff education is the foundation for a high clean claim in medical billing rate. Regular training sessions ensure billing and coding teams stay current with CPT, ICD-10, and payer policy updates. This reduces knowledge gaps and minimizes costly mistakes.
- Monthly workshops review recent claim denials and coding changes.
- Annual certification programs boost staff expertise.
- Cross-training between billing and clinical teams strengthens understanding of documentation requirements.
By investing in ongoing education, organizations see measurable drops in claim rejections and denials. Well-trained staff recognize common pitfalls, anticipate payer edits, and complete claims correctly the first time.
Leveraging Professional RCM Services
Partnering with experienced RCM service providers significantly improves clean claim in medical billing performance. RCM teams bring specialized expertise in coding, compliance, and payer rules, adapting seamlessly to your existing software and workflows.
- Professionals conduct thorough eligibility checks and documentation reviews.
- Outsourcing denial management reduces internal workload.
- RCM partners monitor regulatory changes and update processes proactively.
These experts ensure claims meet payer requirements and assist in resolving complex issues quickly. Many healthcare organizations report higher clean claim rates and faster reimbursements after engaging RCM services.
Implementing Quality Assurance and Internal Audits
A structured quality assurance program is essential for maintaining a high clean claim in medical billing rate. Regular internal audits catch trends, systemic issues, and recurring errors before claims reach payers.
- Use standardized checklists to validate patient demographics and coding.
- Conduct quarterly audits to assess process accuracy.
- Analyze audit findings to implement targeted improvements.
By identifying root causes of denials, organizations can refine workflows and provide corrective feedback to staff. This systematic approach ensures continuous improvement and greater financial stability.
Keeping Up with Regulatory and Payer Changes
Regulatory updates and payer policy shifts are constant in the world of clean claim in medical billing. Staying informed is crucial to avoid unnecessary denials and maintain compliance with 2026 standards.
- Subscribe to CMS and payer bulletins for real-time updates.
- Designate a compliance officer to track code set changes.
- Update internal policies and training materials promptly.
Proactive adaptation to new rules reduces disruption and ensures your claims align with current requirements. This vigilance safeguards revenue and minimizes audit risk.
Data Analytics and Performance Monitoring
Harnessing data analytics is a game-changer for clean claim in medical billing optimization. Advanced dashboards and reporting tools reveal bottlenecks, track denial trends, and highlight high-performing teams.
- Monitor clean claim rates monthly to identify variances.
- Use analytics to pinpoint frequent error types and address root causes.
- Set performance benchmarks and reward staff for improvements.
Data-driven insights enable organizations to take swift, targeted action. Continuous monitoring ensures accountability and supports long-term revenue growth.
Collaboration Between Billing, Coding, and Clinical Teams
Effective collaboration across departments is vital to achieving a superior clean claim in medical billing outcome. Open communication ensures documentation, coding, and billing processes are aligned from the outset.
- Hold regular interdisciplinary meetings to discuss denial trends.
- Foster a feedback loop between clinical and coding staff.
- Share best practices and celebrate collective successes.
Collaborative workflows reduce misunderstandings and help resolve issues before claims are submitted. This team-based approach transforms billing accuracy and strengthens overall financial performance.
Common Errors and How to Avoid Them
Even with advanced tools and experienced billing teams, avoiding errors is essential for maintaining a high clean claim in medical billing rate. Understanding the most frequent mistakes and their solutions can dramatically increase efficiency and revenue for healthcare organizations.
Demographic and Insurance Information Mistakes
One of the most common obstacles to a clean claim in medical billing is incorrect or incomplete demographic and insurance information. Errors such as misspelled patient names, inaccurate dates of birth, or invalid insurance IDs can instantly trigger claim rejections.
To prevent these mistakes, staff should implement strict verification protocols at both registration and pre-claim stages. Double-checking patient details against insurance cards and using electronic verification tools can catch discrepancies early. Automated alerts for missing or mismatched data also help ensure accuracy before claim submission.
Consistent training on verification processes and regular audits can further reduce these preventable errors. A focus on detail at the front end sets the stage for successful claim outcomes.
Coding and Documentation Errors
Accurate coding and complete documentation are vital for achieving a clean claim in medical billing. Using outdated or incorrect CPT, ICD-10, or HCPCS codes is a leading cause of denials. Additionally, insufficient documentation to support medical necessity can result in costly delays.
Stay updated with annual codebook revisions and payer-specific requirements. Schedule regular documentation audits to identify gaps and ensure that every claim has the necessary supporting evidence. Leveraging resources like Accurate CPT codes for insurance claims can help billing teams stay informed and avoid common pitfalls.
Encourage open communication between clinical and billing teams to clarify coding questions and maintain compliance. This proactive approach supports clean, compliant submissions.
Authorization and Referral Lapses
Missing or expired prior authorizations are a frequent reason claims fail to qualify as clean. Without timely approvals, even perfectly coded claims can face rejection.
Implement real-time authorization tracking systems to monitor the status of required referrals and authorizations. These tools can alert staff to expiring or missing documents, reducing the risk of denials. Regularly update workflows to account for payer-specific authorization requirements and deadlines.
Payer-Specific Rule Violations
Every payer has unique rules that impact clean claim in medical billing outcomes. Failing to use the correct modifiers, omitting required attachments, or not following payer-specific formatting can lead to quick rejections.
Maintain a regularly updated database of payer requirements accessible to all billing staff. Use checklists to ensure all criteria are met before submission. Periodic training on payer updates keeps teams prepared for changes, supporting higher clean claim rates.
Timely Filing and Submission Delays
Claims not submitted within payer deadlines are automatically denied, regardless of their accuracy. Timely filing is a core component of a clean claim in medical billing.
Set up automated reminders and workflow tools to track filing windows for each payer. Assign accountability for timely submissions to specific team members. Routinely review claim aging reports to identify and resolve bottlenecks before deadlines are missed.
Example: Top Denial Reasons in 2026
Below is a summary of the leading causes for claim denials, based on industry data:
| Denial Reason | Percentage (%) |
|---|---|
| Eligibility issues | 28 |
| Coding errors | 24 |
| Lack of documentation | 19 |
| Authorization lapses | 15 |
| Payer-specific violations | 9 |
| Late submission | 5 |
By addressing these common errors, healthcare organizations can significantly improve their clean claim in medical billing rates and overall revenue cycle performance.
Future Trends and Best Practices for Clean Claims in 2026
Staying ahead in the revenue cycle requires understanding the evolving landscape of clean claim in medical billing. As technology and regulations advance, healthcare organizations must adapt their processes to maintain high standards, secure reimbursements, and minimize errors.
Technological Advancements in Claims Processing
Modern technology is revolutionizing clean claim in medical billing. Artificial intelligence (AI) tools and predictive analytics are now central to claim scrubbing, error detection, and process automation. These solutions help reduce human error and ensure claims are accurate before submission.
Interoperability between EHRs and payers is also improving. Seamless data exchange minimizes manual entry and shortens the claim lifecycle. According to recent reports, AI tools can reduce claim errors by up to 40%. The AI in Medical Billing Market Growth demonstrates the rising demand for automation and compliance in healthcare billing.
Regulatory Changes and Their Impact
The regulatory environment for clean claim in medical billing continues to evolve. In 2026, updates from CMS and commercial payers include new code sets, stricter documentation requirements, and enhanced data exchange standards. HIPAA rules now emphasize interoperability, making it essential for providers to integrate compliant workflows.
Staying current with these changes is critical. The CMS initiative to modernize payment accuracy highlights the importance of compliant claims and reduced waste. Learn more about these changes in the CMS Modernizes Payment Accuracy and Reduces Waste press release.
Emphasis on Data Security and Compliance
Data security is foundational for clean claim in medical billing. HIPAA compliance is non-negotiable, requiring encrypted data transmission and secure storage for all claim-related information. Any breach can result in financial penalties and damaged trust.
Protecting patient data and ensuring secure access to billing systems should be a top priority for every organization.
Value-Based Care and Clean Claims
The rise of value-based care models puts additional focus on clean claim in medical billing. Clean claims are essential for bundled payments and value-based reimbursement contracts, as they ensure timely, accurate payment and reduce administrative friction.
Organizations that prioritize clean claims are better positioned to succeed in these evolving payment structures.
Best Practices Checklist for 2026
To maintain high clean claim rates, healthcare organizations should:
- Ensure registration accuracy at every patient encounter
- Keep coding and documentation up to date
- Use quality assurance protocols and regular audits
- Monitor analytics dashboards for trends and bottlenecks
- Stay compliant with regulatory and payer requirements
Following this checklist helps streamline workflows and reduce costly errors.
Preparing Your Practice for the Future
Building a culture of continuous improvement is vital for clean claim in medical billing. Invest in staff training, embrace new technologies, and review processes regularly. By staying proactive, your organization can adapt quickly to changes and maintain operational excellence.
Partnering with Professional RCM Services for Clean Claims
In today’s complex healthcare landscape, achieving a high clean claim in medical billing rate is critical for financial success. However, the evolving regulatory environment and payer requirements can make this process challenging for practices of any size. Many organizations are turning to professional revenue cycle management (RCM) services to streamline their billing operations and reduce costly errors.
Greenhive Billing Solutions specializes in maximizing clean claim in medical billing outcomes for healthcare providers. Our experienced teams work directly within client-owned software and adapt to each client’s existing workflows. We ensure that every claim meets the latest compliance standards for 2026, including HIPAA, payer-specific rules, and up-to-date code sets.
By leveraging our expertise in coding, eligibility verification, and Denial management in medical billing, we help our clients achieve significantly higher clean claim in medical billing rates. Our clients report faster reimbursements, fewer denials, and improved revenue cycle performance. Real-world results show consistent increases in collections and a measurable reduction in administrative workload.
Partnering with Greenhive means transparent communication, tailored solutions, and strict adherence to data security standards. Outsourcing RCM services allows your organization to reallocate internal resources, freeing your team to focus on delivering excellent patient care. With the right support, your practice can confidently navigate the complexities of clean claim in medical billing and secure long-term financial health.
After exploring the strategies and best practices for clean claims in 2026, you might be wondering how to put these insights into action for your own practice. Navigating new regulations, technology, and payer requirements isn’t always easy—but you don’t have to do it alone. At Greenhive Billing Solutions, we’re here to help you streamline your billing processes, reduce denials, and boost your financial performance with tailored, compliant solutions. If you’re ready to see how expert support can make a measurable difference, let’s connect.
Book Your Free Consultation
and discover how you can achieve a higher clean claim rate with confidence.