Did you know that authorization delays can cost healthcare organizations millions each year and directly impact patient care? In 2026, authorization in medical billing remains a complex challenge for providers, as payer requirements continue to evolve. Navigating this process is crucial not only for reducing claim denials but also for improving patient satisfaction and financial performance. This guide delivers expert insights, current best practices, and actionable strategies to help providers, billing professionals, and healthcare administrators master the entire authorization workflow. Ready to take control? Dive in for practical solutions and the latest trends shaping medical billing this year.
Understanding Authorization in Medical Billing
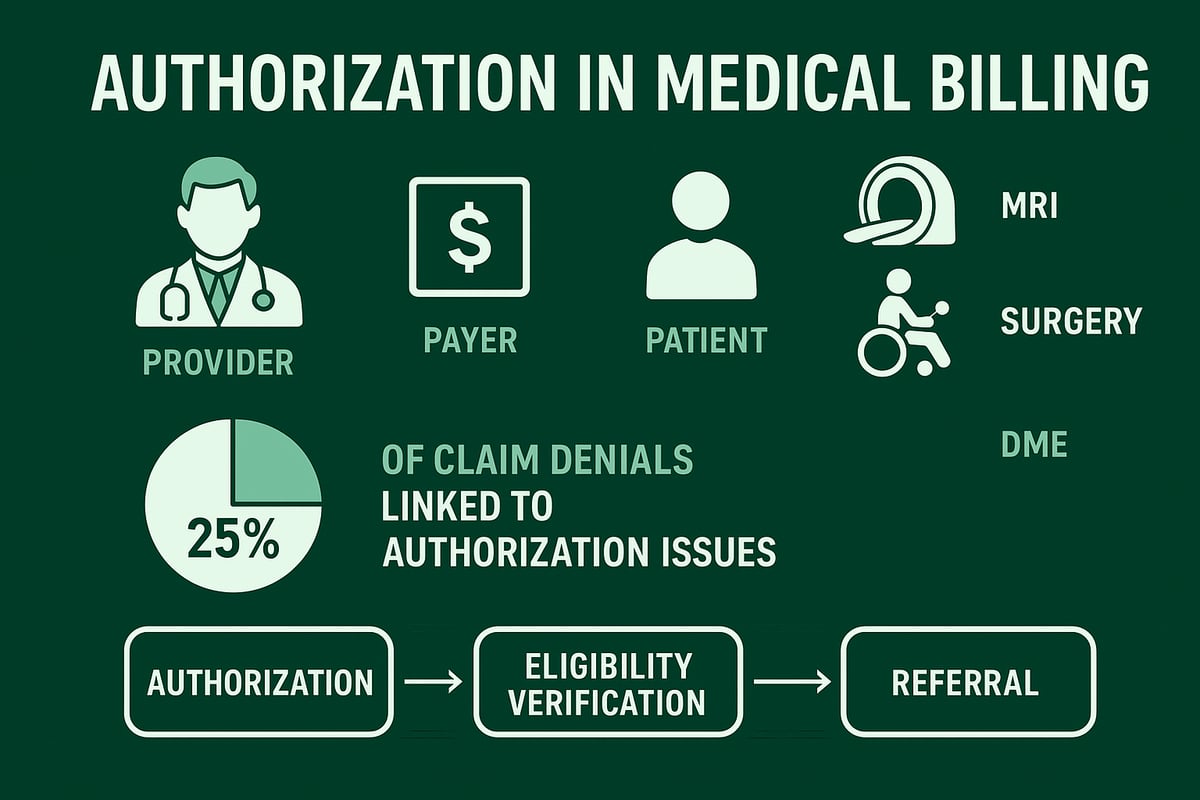
Authorization in medical billing is a formal process where healthcare providers obtain approval from payers before delivering specific medical services. This step is distinct from eligibility verification, which confirms a patient’s coverage, and from referrals, which are recommendations from a primary care provider for specialist care. Payers require authorization to manage utilization and control costs, ensuring only medically necessary procedures are performed. This process directly affects patient access to care and provider reimbursement, especially for high-value services like MRIs or surgeries. In fact, up to 25% of claim denials are linked to authorization issues, making it critical to understand and optimize this workflow. For a deeper dive into how this process works, visit the Prior authorization services overview.
What is Authorization?
Authorization in medical billing refers to the payer’s approval required before a provider delivers certain healthcare services. Unlike eligibility verification, which checks if a patient has active coverage, or a referral, which is a primary provider’s recommendation, authorization is about getting payer consent for specific procedures. Payers implement this step to ensure utilization management and cost containment. Without proper authorization, patients may face barriers to care, and providers risk not being reimbursed. For example, a patient needing an MRI or elective surgery often requires pre-approval. With up to 25% of claim denials tied to authorization in medical billing, mastering this process is vital.
Key Purposes and Benefits
The primary purpose of authorization in medical billing is to prevent unnecessary or duplicative services. It also helps verify medical necessity, especially for costly treatments. By ensuring that only appropriate care is delivered, payers can manage risk and reduce overall healthcare spending. For providers, this process offers financial protection from uncompensated care by clarifying coverage before services are rendered. Additionally, it enhances patient understanding of what is covered, helping to avoid surprise bills. Ultimately, effective authorization in medical billing promotes accountability and transparency for all parties involved.
Types of Services Commonly Requiring Authorization
Certain healthcare services almost always require authorization in medical billing due to their complexity or cost. These include inpatient admissions, extended hospital stays, and advanced imaging such as MRI, CT, and PET scans. Durable medical equipment (DME) and high-cost specialty drugs also fall into this category. Surgeries, complex outpatient procedures, behavioral health, and home health services often trigger the need for prior approval. Recognizing which services require authorization in medical billing helps providers avoid claim denials and streamline the patient care journey.
Authorization vs. Referral vs. Eligibility Verification
Understanding the differences between authorization in medical billing, referrals, and eligibility verification is essential for clean claims. Eligibility verification confirms a patient’s active coverage and plan details. A referral is a primary care provider’s recommendation for specialist care, often needed in HMO or POS plans. Authorization, on the other hand, is payer approval for a specific service. Confusing these steps can lead to denied claims and delayed care.
| Process | Purpose | Example |
|---|---|---|
| Eligibility Verification | Confirm coverage | Checking insurance status |
| Referral | PCP recommends specialist | PCP refers to cardiologist |
| Authorization | Payer approves service | Pre-approval for MRI |
Integrating all three steps in authorization in medical billing ensures compliance and improves reimbursement outcomes.
Types of Authorization in Medical Billing
Navigating the landscape of authorization in medical billing is crucial for ensuring timely care, minimizing denials, and maintaining compliance in 2026. Each type of authorization serves a distinct role, reflecting the complexity of payer requirements and the evolving nature of healthcare services.
Prior Authorization (Pre-Authorization)
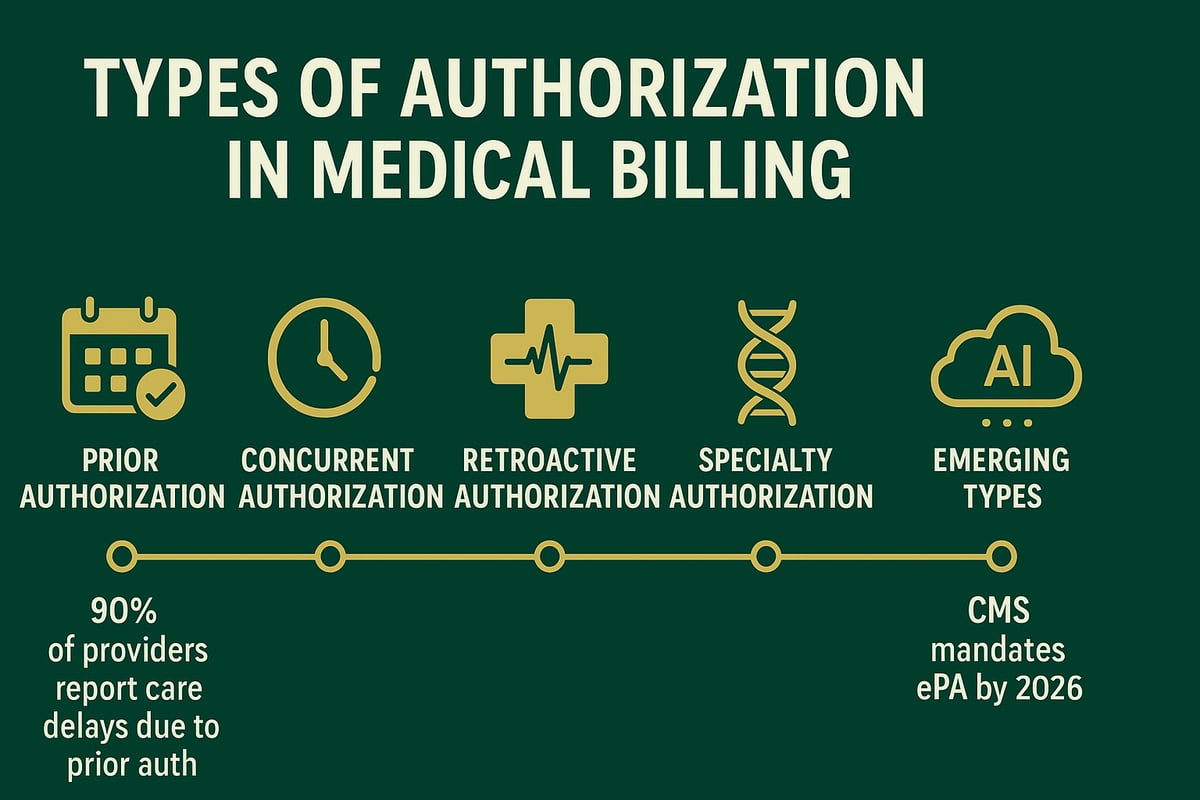
Prior authorization in medical billing is a process where providers obtain approval from payers before delivering specific services or treatments. This type of authorization is most commonly required for elective surgeries, high-cost medications, and advanced imaging procedures. For example, a provider must secure prior authorization before administering biologic drugs or scheduling non-urgent orthopedic surgery.
The process typically involves submitting detailed clinical documentation and waiting for payer review, which may take 24 to 72 hours. According to the AMA, over 90% of providers experience care delays due to prior authorization requirements. Missing or incorrect information can result in denials, so integrating robust workflows is essential for success in authorization in medical billing.
Concurrent Authorization
Concurrent authorization in medical billing applies when ongoing approval is necessary during a patient’s course of treatment. This is especially relevant for extended inpatient hospitalizations or long-term therapies, such as rehabilitation or chemotherapy. Providers regularly submit updates and clinical information to justify continued services.
If concurrent authorization lapses or is not properly managed, care interruptions and reimbursement issues may arise. For instance, if a hospital stay extends beyond the originally approved days, the provider must seek additional concurrent authorization in medical billing to avoid claim denials and ensure uninterrupted patient care.
Retroactive Authorization
Retroactive authorization in medical billing refers to obtaining payer approval after services have already been rendered. This is typically allowed in emergencies or when coverage transitions prevent timely prior authorization. Providers must submit comprehensive documentation explaining the urgent need for care and the circumstances that prevented advance approval.
A common scenario involves emergency surgery performed without prior authorization due to immediate risk to the patient. Retroactive authorization in medical billing requires strict adherence to payer timelines and policies, as delayed or insufficient documentation can lead to payment denials and financial losses for both providers and patients.
Specialty Authorization
Specialty authorization in medical billing focuses on services that require advanced expertise or unique treatment protocols, such as oncology, cardiology, or fertility care. These authorizations often involve complex clinical reviews and additional layers of documentation, including genetic testing results or prior treatment records.
The interplay between referrals and specialty authorization in medical billing is critical, as many payers require both a referral from a primary care provider and a separate authorization for the specialist’s intervention. For example, obtaining specialty authorization is essential for approval of targeted cancer therapies, ensuring appropriate and covered care.
Referral Authorization
Referral authorization in medical billing is initiated by a primary care provider (PCP) when a patient needs to see a specialist. This process is common in Health Maintenance Organization (HMO) and Point of Service (POS) plans, where network rules are strict. The PCP submits a referral request, and once approved, the patient can access specialist services.
Properly documenting referral authorization in medical billing is crucial; errors or omissions can result in denied claims or increased out-of-pocket costs for patients. For instance, a dermatology consult for a suspicious skin lesion requires both a PCP referral and payer authorization to guarantee coverage and compliance.
Other Emerging Types (2026 Trends)
In 2026, digital and automated solutions are reshaping authorization in medical billing. Real-time electronic prior authorization (ePA) platforms, AI-driven workflows, and payer portals are reducing manual effort and speeding up approvals. Telehealth and virtual care services have prompted new authorization rules, with some payers now offering instant decisions for remote behavioral health visits.
Regulatory changes, such as the CMS Interoperability and Prior Authorization Final Rule, mandate greater transparency and faster turnaround times for authorization in medical billing. The widespread adoption of ePA and automation is expected to streamline processes and improve outcomes for both providers and patients.
Step-by-Step Authorization Workflow in 2026
Navigating the authorization in medical billing workflow in 2026 requires a precise, step-by-step approach. Each stage is vital to ensure clean claims, reduce denials, and support timely patient care. Below, we break down the modern workflow, highlighting best practices and real-world examples at every phase.
Step 1: Insurance Eligibility Verification
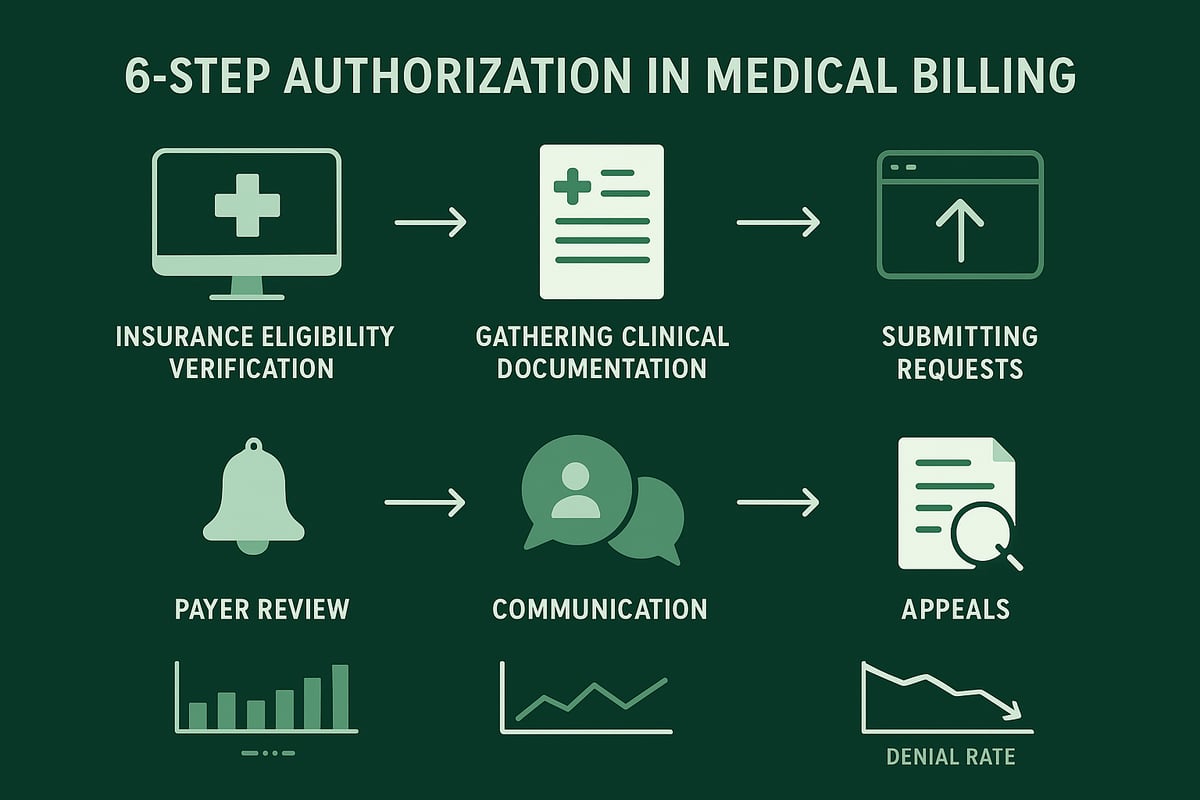
The first step in authorization in medical billing is verifying insurance eligibility. This process confirms the patient’s active coverage and identifies which services require prior approval. Accurate eligibility checks prevent costly mistakes and claim denials.
Modern practices rely on integrated EHR tools and payer portals for real-time eligibility confirmation. For example, automated systems can flag services needing authorization during appointment scheduling. For more details on optimizing this step, review Eligibility verification best practices.
A thorough eligibility verification at this stage lays the foundation for smooth authorization in medical billing throughout the rest of the process.
Step 2: Gathering Clinical Documentation
The second step of authorization in medical billing involves collecting all necessary clinical documentation. This includes provider notes, lab results, imaging studies, and any evidence supporting medical necessity.
Each payer has specific requirements, so documentation must match their criteria exactly. Missing or incomplete records often lead to delays or outright denials. For example, durable medical equipment requests may need recent test results and detailed physician notes.
Timely and accurate documentation ensures that authorization in medical billing requests are processed efficiently and meet payer expectations.
Step 3: Submitting Authorization Requests
Submitting the authorization in medical billing request comes next. Practices use various channels such as online portals, fax, phone, or clearinghouses, but digital submissions are increasingly standard in 2026.
Standard forms must be filled out completely, including all relevant patient, provider, and clinical details. Submitting through a payer’s digital portal often speeds up review times. For example, many payers now offer real-time status updates for submitted requests.
Careful attention to submission details reduces errors and supports a successful authorization in medical billing outcome.
Step 4: Payer Review and Response
After submission, payers conduct a review as part of the authorization in medical billing workflow. Depending on service complexity, review timelines may range from 24 to 72 hours.
Payers respond with an approval, denial, or request for more information. Tracking the status of each request is essential, especially for concurrent authorizations, such as ongoing hospital stays.
Prompt follow-up on payer communications helps avoid unnecessary care delays and keeps the authorization in medical billing process on track.
Step 5: Communicating Outcomes to Patients and Providers
The next essential step in authorization in medical billing is to communicate outcomes promptly. Clinical teams and patients must be notified as soon as a decision is made.
If an authorization is denied or partially approved, providers should discuss alternative options or the next steps. All communications should be documented for compliance. For example, notifying a patient about a denied specialty drug allows for timely appeals or care adjustments.
Clear and timely communication supports transparency and patient satisfaction during the authorization in medical billing journey.
Step 6: Appeals and Reconsiderations
If a request is denied, the final step in authorization in medical billing is the appeals process. Providers must gather additional documentation, address payer feedback, and submit appeals within specified timelines.
Understanding escalation paths and preparing comprehensive appeal packets are crucial for overturning denials. For example, appealing a denied pre-authorization for surgery may require medical literature and updated clinical notes.
A structured approach to appeals not only recovers lost revenue but also strengthens future authorization in medical billing efforts.
Common Authorization Challenges and How to Overcome Them
Healthcare organizations continue to face significant hurdles with authorization in medical billing, affecting both operational efficiency and patient care. Understanding the most common challenges and how to address them is critical for providers aiming to reduce denials, accelerate reimbursements, and enhance patient satisfaction.
Frequent Reasons for Authorization Denials
Authorization in medical billing is particularly prone to denials due to a range of preventable errors. The most frequent reasons include:
- Submission of incomplete or incorrect patient or procedural information.
- Absence of required clinical documentation to establish medical necessity.
- Failure to follow payer-specific criteria or using outdated forms.
- Use of out-of-network providers for services that require pre-authorization.
- Expired or missing authorizations at the time of claim submission.
Each of these issues can result in payment delays or outright claim denials. Proactive review of authorization in medical billing requirements and regular audits of submission processes are essential to minimize these avoidable errors.
Administrative and Workflow Bottlenecks
Many practices struggle with internal workflow challenges that hinder effective authorization in medical billing. Common bottlenecks include:
- Insufficient staff training on payer requirements and evolving policies.
- High turnover among billing or authorization teams, leading to knowledge gaps.
- Heavy reliance on manual tracking systems such as spreadsheets or paper logs.
- Slow communication between clinical staff and billing teams, causing missed deadlines.
To address these challenges, organizations should invest in staff education and adopt automated tracking tools that streamline the authorization in medical billing process. This not only reduces errors but also ensures timely follow-up on outstanding requests.
Payer-Specific Complexities
No two payers are alike when it comes to authorization in medical billing. Providers must navigate:
- Different documentation requirements and medical necessity criteria for each insurance plan.
- Frequent changes in payer policies, requiring constant vigilance and updates.
- Multiple online portals and submission systems, each with unique processes and timelines.
For example, the steps to obtain an authorization for a Medicare Advantage patient may differ significantly from those for a commercial insurance plan. Misunderstanding these nuances can lead to avoidable denials and increased administrative burden. Maintaining a payer matrix and regular policy reviews can help standardize processes and reduce confusion.
Patient Impact and Satisfaction Risks
When authorization in medical billing is delayed or denied, the effects ripple out to patients. Common risks include:
- Delays in scheduling or receiving medically necessary treatments.
- Unexpected out-of-pocket expenses if services are denied after delivery.
- Negative experiences that can impact satisfaction scores and patient retention.
A delay in cancer therapy, for instance, due to an authorization denial can have serious health and emotional consequences for patients. Clear communication with patients about authorization status and coverage expectations is crucial for fostering trust and satisfaction.
Best Practices for Reducing Denials and Delays
Implementing structured workflows and proactive communication can dramatically improve outcomes in authorization in medical billing. Key best practices include:
- Using standardized checklists to ensure all required data is collected before submission.
- Conducting regular training sessions for staff on payer updates and documentation standards.
- Leveraging technology for automated reminders, status tracking, and integrated EHR workflows.
- Establishing open lines of communication with payers and patients to resolve issues quickly.
Industry data shows that denial rates can drop by 30% when robust pre-authorization processes are in place. For more targeted strategies, explore these denial management strategies to further minimize authorization-related claim denials and optimize your revenue cycle.
Regulatory Updates and Payer Policy Changes for 2026
Navigating regulatory changes is critical for anyone managing authorization in medical billing. The landscape in 2026 is rapidly evolving, with new federal mandates, payer-driven reforms, and industry-wide technological upgrades shaping how practices secure approvals and minimize claim denials.
CMS and Federal Regulations
For 2026, CMS has finalized rules requiring greater transparency and faster turnaround times for authorization in medical billing. These regulations mandate electronic prior authorization (ePA) for Medicare, Medicaid, and many commercial plans. Practices must ensure all requests and responses are transmitted electronically, reducing paper-based delays.
The new CMS rules establish maximum response windows, often 72 hours for urgent requests, which directly impacts operational workflows. Practices should familiarize themselves with these requirements and monitor updates closely. For a deeper look at how these federal changes will improve prior authorization processes, see CMS Finalizes Rule to Expand Access to Health Information.
Failure to comply with these standards can result in delayed payments and increased denials. Ensuring that your workflow aligns with federal requirements is essential for success with authorization in medical billing.
Major Payer Policy Shifts
Private payers are also shifting their approach to authorization in medical billing. Many insurers are streamlining or even eliminating prior authorization requirements for select services, particularly preventive care and routine screenings. This trend is designed to reduce administrative burden for providers and improve patient access.
Payers are investing in automated approval systems and exploring new policies for telehealth and remote care, reflecting lessons learned during the pandemic. For example, some insurers have begun waiving authorization for virtual visits and behavioral health services, a significant change from previous years.
Staying informed about these evolving payer-specific requirements is crucial for anyone managing authorization in medical billing. Regularly check payer bulletins and participate in industry forums to stay ahead of policy changes.
Industry Standards and Best Practices
Industry groups such as the AMA and MGMA are leading efforts to standardize authorization in medical billing. Widespread adoption of electronic data interchange (EDI) and artificial intelligence is making real-time approvals more common. These standards help reduce manual errors, speed up approvals, and improve the overall efficiency of revenue cycle management.
AI-powered systems can flag incomplete requests, ensure documentation meets payer criteria, and track status updates automatically. Following best practices, like using certified EHR integrations and standardized checklists, helps practices adapt to new industry norms for authorization in medical billing.
Ongoing collaboration between providers, payers, and technology vendors is accelerating these improvements, making compliance less burdensome and more transparent.
Preparing Your Practice for 2026 Changes
To stay compliant with the latest requirements for authorization in medical billing, practices should conduct regular audits of their workflows. Upgrading to EHR and billing systems that support ePA is now essential. Staff training on new payer portals and federal rules should be a priority.
Create a compliance checklist that includes documentation standards, eligibility verification, and timely submission protocols. Engage in ongoing education through webinars and professional associations to keep your team informed about regulatory updates.
By proactively preparing, you can ensure your practice meets 2026’s regulatory demands and maintains a high standard for authorization in medical billing.
Technology and Automation in Authorization Management
Staying ahead in authorization in medical billing depends on embracing technology and automation. As digital solutions mature, providers can streamline workflows, reduce errors, and respond faster to payer requirements. Technology not only accelerates routine tasks but also supports compliance, data security, and continual performance improvement.
Digital Authorization Platforms and Tools
Modern digital platforms are transforming authorization in medical billing. Electronic prior authorization (ePA) solutions integrate seamlessly with EHR and practice management systems, allowing staff to submit requests and receive real-time updates without leaving their workflow. These platforms reduce manual data entry, minimize errors, and speed up approvals.
Providers benefit from automated reminders, standardized forms, and built-in payer rules. Many payers now offer online portals for faster submissions. Industry momentum is building, as health insurers work to ease prior authorization requirements through streamlined digital processes and greater transparency. Adopting these tools is essential for efficient authorization in medical billing as payer requirements evolve.
AI and Machine Learning Applications
Artificial intelligence is optimizing authorization in medical billing by automating complex, repetitive tasks. AI-driven platforms use predictive analytics to flag which services require authorization, extract relevant clinical data, and auto-complete forms with high accuracy. Machine learning models learn from historical data to identify patterns, helping staff prioritize high-risk or time-sensitive cases.
These tools significantly reduce processing time. In fact, AI-powered solutions can cut authorization turnaround by 40 percent, freeing up staff for more value-added work. As AI continues to develop, it will become a cornerstone of efficient authorization in medical billing, helping organizations stay ahead of payer changes.
Data Security and HIPAA Compliance
As practices digitize authorization in medical billing, safeguarding patient data is non-negotiable. Platforms must ensure secure data transmission, robust encryption, and strict access controls. HIPAA and state privacy rules dictate how information is stored, shared, and audited across systems.
Best practices include using cloud-based solutions with end-to-end encryption, regular user access reviews, and comprehensive audit trails. By prioritizing security, providers protect both their patients and their reputation. Secure technology is foundational for successful authorization in medical billing, especially as automation increases data exchange.
Measuring ROI and Performance
To maximize the value of technology in authorization in medical billing, organizations must track key performance indicators. Metrics such as approval rates, turnaround times, and denial rates provide actionable insights. Monthly dashboards and benchmarking help practices identify bottlenecks and areas for improvement.
Leveraging analytics, revenue cycle teams can refine workflows, reduce claim denials, and boost financial outcomes. For more on how technology and denial management drive results, see improving cash flow with denial management. Continuous measurement ensures technology investments translate to tangible gains in authorization in medical billing.
Training, Outsourcing, and Expert Support for Authorization Success
Building a strong foundation for authorization in medical billing depends on having the right expertise, tools, and support systems in place. As payer rules and technologies evolve, investing in staff development and strategic partnerships can transform your revenue cycle performance.
Building an Expert Authorization Team
A dedicated and knowledgeable team is essential for successful authorization in medical billing. Key roles include authorization specialists, billers, and clinical reviewers, each bringing unique expertise to the process. Certification and ongoing education keep staff current with the latest payer requirements and regulatory changes.
Cross-training enables coverage during absences, ensuring no interruption in workflow. Practices that invest in certified staff often see a measurable reduction in claim denials and faster turnaround times. Consider regular in-service sessions and workshops to keep your team sharp and compliant.
| Role | Key Responsibilities |
|---|---|
| Authorization Specialist | Request submission, payer follow-up |
| Biller | Claims integration, documentation |
| Clinical Reviewer | Medical necessity evaluation |
When to Outsource Authorization Management
For many organizations, the demands of authorization in medical billing can exceed in-house capacity. Outsourcing becomes a strategic option when high volumes, complex specialty services, or rapid payer changes create administrative burdens.
Outsourcing offers scalability, access to specialized expertise, and advanced technology platforms that streamline workflows. It helps reduce errors, minimize delays, and improve denial management. Evaluate potential vendors by their compliance standards, transparent reporting, and proven results with practices similar to yours.
Practices with frequent staff turnover, specialty authorizations, or rapid growth often achieve greater efficiency and cost savings through an experienced outsourcing partner.
Partnering with Greenhive Billing Solutions for Authorization Excellence
Partnering with Greenhive Billing Solutions elevates your approach to authorization in medical billing through end-to-end management and technology-driven workflows. Greenhive’s experts understand payer-specific requirements for specialty authorizations and proactively prevent denials.
Their integrated, HIPAA-compliant systems deliver fast, accurate submissions and real-time tracking for every request. Transparent communication with your clinical and billing teams ensures nothing falls through the cracks. With Greenhive, practices nationwide report reduced denial rates, improved cash flow, and higher patient satisfaction scores.
Choosing the right partner can be a catalyst for sustained success and compliance in today’s complex landscape.
Continuous Improvement and Staying Informed
Success in authorization in medical billing requires ongoing vigilance. Regularly update your team on payer policies, regulatory changes, and best practices. Conduct process audits and leverage resources from professional associations like CMS and AMA to stay ahead of the curve.
As you’ve seen throughout this guide, mastering authorization in medical billing can make a significant difference in reducing denials and ensuring faster reimbursements for your practice. If you’re ready to streamline your workflows, stay compliant with evolving regulations, and boost your financial performance, you don’t have to do it alone. Let’s work together to build a customized solution that meets your unique needs and supports your team every step of the way.
Book Your Free Consultation and discover how Greenhive Billing Solutions can help you take the guesswork out of authorization management.