Accurate coding of pos 21 in medical billing is crucial for hospitals seeking full reimbursement and maintaining compliance. Even minor errors can lead to denied claims, lost revenue, and increased audit risk.
This essential guide is designed to clarify the complexities of pos 21 in medical billing, helping healthcare organizations and billing teams improve claims accuracy and financial performance.
Inside, you will find clear explanations of what POS 21 means, when and how to use it, how it differs from other place of service codes, and practical strategies to avoid common mistakes. You will also learn about reimbursement impacts and compliance best practices.
By mastering the principles in this guide, you can protect your revenue, streamline your billing processes, and ensure ongoing regulatory compliance.
Understanding POS 21: Definition, Purpose, and Regulatory Context
Understanding pos 21 in medical billing is essential for any healthcare organization aiming for accurate claims and proper reimbursement. This section explains what POS 21 means, regulatory requirements, its impact on revenue cycles, and provides industry data to help your team avoid common pitfalls.
What is POS 21?
POS 21 in medical billing refers to the designation “Inpatient Hospital.” This code is used when a patient is formally admitted to a hospital and receives continuous, 24-hour care under direct medical supervision. POS 21 is defined by the Centers for Medicare & Medicaid Services (CMS) and is recognized by all major payers.
Assigning this code signals that the services provided took place within the hospital facility, under the appropriate inpatient protocols. Accurate use of pos 21 in medical billing sets the stage for selecting the correct claim type, reimbursement methodology, and compliance with payer rules.
Regulatory and Payer Guidelines for POS 21
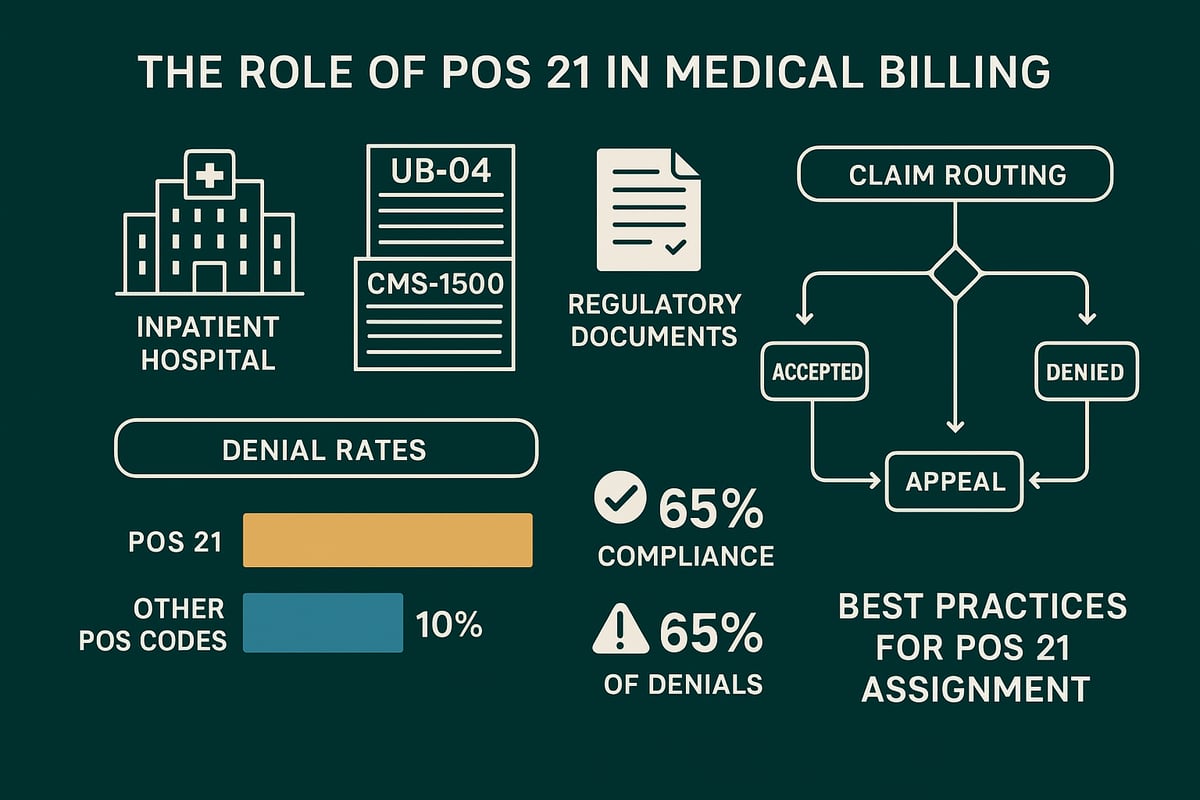
Regulatory bodies like CMS and commercial payers set strict guidelines for using pos 21 in medical billing. Inpatient designation requires clear physician orders, documented medical necessity, and adherence to established admission criteria. Claims are reported using forms such as the UB-04 for facilities and CMS-1500 for physicians, depending on the payer.
Recent updates emphasize the importance of aligning documentation with inpatient status and following payer-specific nuances. For a deeper dive into compliance strategies and common errors, consult this comprehensive POS 21 Billing Guide. Staying current with regulatory changes is essential to avoid audit triggers and ensure compliant billing.
Why POS 21 Matters: Impact on Billing and Revenue Cycle
The correct use of pos 21 in medical billing directly affects how claims are routed—determining whether they are processed as inpatient or outpatient. This distinction drives eligibility for Diagnosis Related Group (DRG) reimbursement, which typically results in higher payments compared to outpatient claims.
Incorrect POS 21 assignment can elevate audit risk, lead to compliance issues with organizations like OIG and CMS, and skew provider performance metrics. For instance, misusing this code may cause claim denials or even recoupments, impacting both cash flow and operational analytics.
Key Statistics and Industry Insights
Industry data shows that a significant percentage of hospital claims involve pos 21 in medical billing. Studies indicate that errors in POS coding contribute to a notable share of claim denials—sometimes exceeding 10% of inpatient claims. The average reimbursement for inpatient (POS 21) claims often surpasses outpatient (POS 22/23) equivalents by thousands of dollars per case.
Recent CMS audits highlight frequent issues with documentation and code assignment. These findings underscore the importance of continuous training and rigorous internal audits to maintain accuracy and maximize revenue.
When and How to Use POS 21 in Medical Billing
Correctly using pos 21 in medical billing is essential for accurate claims and optimized hospital revenue. Assigning this code involves careful evaluation of patient status, thorough documentation, and adherence to regulatory standards. By understanding the criteria and following best practices, your billing team can reduce denials and safeguard compliance.
Criteria for Assigning POS 21
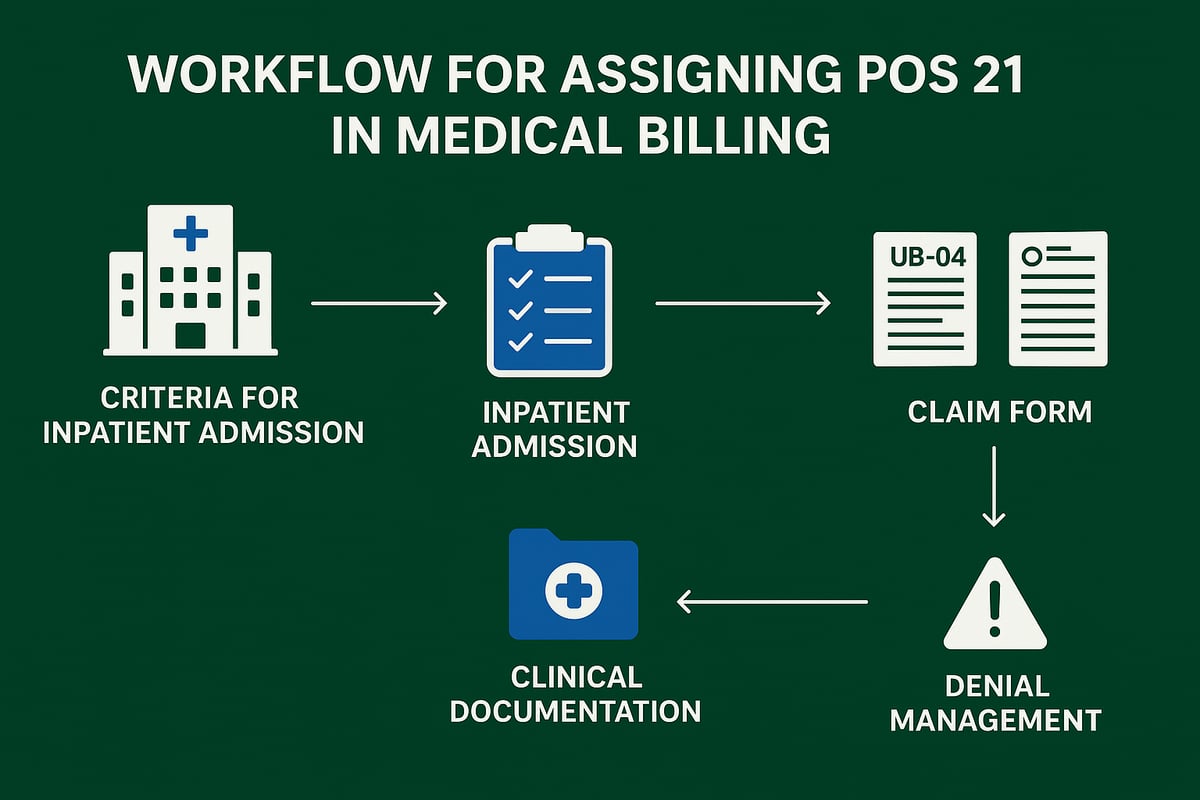
Assigning pos 21 in medical billing starts with determining if the patient requires inpatient care. The patient must have a documented medical necessity for hospital admission, supported by a physician’s order. While inpatient stays often last more than 24 hours, a shorter stay can still qualify if the clinical situation warrants it.
Services must occur within a licensed hospital facility. Typical scenarios include complex surgeries, acute illness management, or cases requiring continuous monitoring. If these conditions are met, pos 21 in medical billing becomes the correct code for the claim.
Step-by-Step Process for Correct POS 21 Usage
A structured workflow helps ensure pos 21 in medical billing is used accurately. Here’s a step-by-step approach:
- Verify Admission: Confirm that a formal inpatient admission order is present and medical necessity is documented in the patient record.
- Review Documentation: Ensure clinical notes, progress reports, and care plans clearly indicate inpatient status and the need for intensive services.
- Code Diagnoses and Procedures: Assign precise ICD-10, CPT, and HCPCS codes aligned with the inpatient episode.
- Select POS 21 on Claims: Enter pos 21 in medical billing forms such as the UB-04 or CMS-1500, as required by the payer.
- Submit and Monitor: File the claim and track its status. Watch for payer edits or denials tied to inpatient status or documentation gaps.
If a denial does occur, prompt action is critical. For more insights on handling claim denials and improving outcomes when using pos 21 in medical billing, see Denial management in medical billing.
Documentation Requirements and Best Practices
Comprehensive documentation is vital for pos 21 in medical billing. Admission and discharge summaries, daily progress notes, and care plans must all reflect inpatient status and care intensity. Clear, contemporaneous records show that the admission was justified and that the hospital provided the expected level of care.
Aligning clinical, administrative, and billing records reduces the risk of denials. Timely updates ensure that any changes in patient status are captured. A best practice is to use standardized checklists and templates, making it easier to meet payer requirements for pos 21 in medical billing.
Common Clinical and Administrative Scenarios
Several scenarios call for pos 21 in medical billing. For example, a patient admitted for an elective surgery that requires overnight monitoring should be coded as inpatient. Similarly, an emergency department visit that results in hospital admission must switch from observation or outpatient codes to pos 21.
Transfers from outpatient to inpatient status can be tricky. It’s important to update the claim and documentation promptly. Misclassifying observation stays as inpatient is a common pitfall, but careful review ensures the correct use of pos 21 in medical billing.
Key Arguments and Compliance Insights
Accurate use of pos 21 in medical billing is essential for compliance with regulatory standards. It protects your organization from audit risks and supports robust quality reporting. Consistent, correct coding also helps benchmark performance and maintain trust with payers.
POS 21 vs. Other Place of Service Codes: Differences and Decision-Making
Understanding pos 21 in medical billing starts with a solid grasp of Place of Service (POS) codes. These codes pinpoint where healthcare services are provided, guiding payers in claims processing and reimbursement. Accurately reporting the service location ensures proper payment and compliance, especially for hospitals and large provider groups.
Overview of Place of Service (POS) Codes
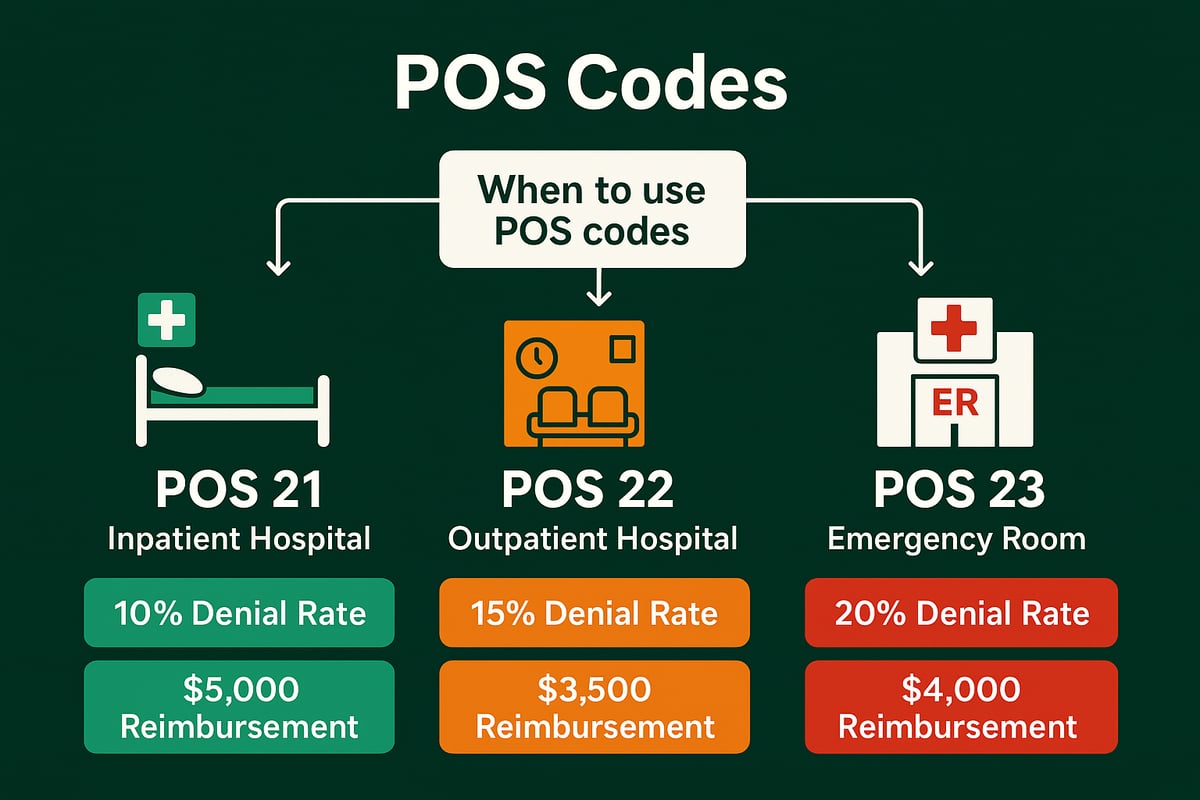
Place of Service codes are two-digit numbers used on medical claims to specify the setting where a service was delivered. For example, pos 21 in medical billing designates inpatient hospital care, while other codes like 11, 22, and 23 represent office, outpatient hospital, and emergency room settings, respectively.
These codes are standardized by CMS and widely adopted by commercial payers. Accurate POS coding is essential for correct claim adjudication, as payers rely on this information to determine payment rates and validate the appropriateness of services. Mistakes can trigger denials or audits, impacting both revenue and compliance.
POS 21 vs. POS 22 (Outpatient Hospital)
The distinction between pos 21 in medical billing and POS 22 is fundamental. POS 21 applies when a patient is formally admitted as an inpatient, with continuous care and overnight observation. In contrast, POS 22 is used for outpatient services, even if performed in the same hospital building but without admission.
The financial implications are significant. Inpatient claims (POS 21) are reimbursed under DRG models, often yielding higher payments than outpatient services (POS 22), which are paid fee-for-service. Selecting the wrong code can cause compliance issues and revenue loss. To avoid common pitfalls, review common mistakes with POS 22 to reinforce the importance of accurate code selection.
POS 21 vs. POS 23 (Emergency Room) and Other Codes
POS 23 is reserved for emergency room visits where the patient is not admitted as an inpatient. If the patient transitions from the ER to inpatient status, pos 21 in medical billing must be used from the point of formal admission. Other codes, like POS 11 (office) or POS 31 (skilled nursing facility), represent distinct care environments and have unique billing rules.
A clear decision tree is critical for staff to determine when to update the POS code, especially during care transitions. Failure to switch from POS 23 to POS 21 at the right time can result in billing errors, denied claims, and audit exposure.
Decision-Making Flowchart and Examples
Navigating pos 21 in medical billing requires a structured approach. Begin by confirming the patient's admission status. If the patient is observed overnight but not admitted, use POS 22 or 23 as appropriate. Once a physician orders inpatient admission, update the POS to 21 for all subsequent services.
Case studies highlight the importance of timely code changes. Training staff with decision-making flowcharts and real-world examples reduces coding errors. Regular audits and clear protocols help maintain accuracy and support compliance, minimizing revenue risk for your organization.
Common Errors and Pitfalls with POS 21—and How to Avoid Them
Mistakes in assigning pos 21 in medical billing can lead to claim denials, compliance issues, and lost revenue. Healthcare organizations must be vigilant, especially after system updates, as new software can introduce coding mismatches. According to Medical Billing Errors Post-Updates, errors such as using POS 21 for outpatient or observation-only services, failing to update the POS when patient status changes, and missing documentation are common. Billing for non-covered services under inpatient status is another frequent pitfall. Ensuring accurate use of pos 21 in medical billing is vital for sustainable revenue.
Frequent POS 21 Mistakes in Medical Billing
Assigning pos 21 in medical billing incorrectly often results from misunderstanding inpatient criteria. Common mistakes include using POS 21 for short stays that do not meet inpatient requirements, failing to update the code when a patient transitions from observation to inpatient, and incomplete documentation. Billing departments may submit claims with pos 21 in medical billing even when no formal admission order exists or when services are not delivered within the licensed facility. Each of these errors increases the risk of claim denials and compliance scrutiny.
Root Causes and Audit Triggers
Root causes for errors with pos 21 in medical billing frequently stem from poor communication between clinical and billing teams. Inconsistent protocols for documenting inpatient admissions, lack of training, and failure to follow payer-specific rules can all lead to mistakes. Auditors often flag high rates of POS 21 usage or discrepancies between admission records and billed codes. Recent findings highlight that short inpatient stays and mismatched documentation are leading triggers for payer audits related to pos 21 in medical billing.
Denial Management and Appeals for POS 21 Issues
When a claim with pos 21 in medical billing is denied, prompt and structured action is essential. Begin by reviewing the denial reason and gathering supporting documentation, such as detailed admission notes and care plans. Submit an appeal referencing payer guidelines and clinical evidence of medical necessity. Track all denials related to pos 21 in medical billing to identify patterns and implement corrective measures. Timely, well-documented appeals can lead to successful revenue recovery and improved payer relationships.
Best Practices for Preventing POS 21 Errors
Preventing errors with pos 21 in medical billing requires continuous staff education and standardized workflows. Implement checklists for admission and billing processes, conduct regular internal audits, and use technology to identify inconsistencies in real time. Encourage collaboration among clinical, administrative, and billing teams to ensure documentation aligns with coding. Organizations that invest in these best practices see a measurable reduction in denial rates and improved accuracy in pos 21 in medical billing.
Key Insights and Industry Data
Industry data shows that errors with pos 21 in medical billing account for a significant percentage of denied inpatient claims. Financially, the average revenue loss per denied claim can be substantial, especially when errors go uncorrected. Benchmarking against industry standards reveals that organizations with robust compliance programs have higher billing accuracy and lower audit risk. Staying informed about payer trends and regulatory changes is crucial for maintaining best-in-class performance with pos 21 in medical billing.
POS 21 and Reimbursement: Financial Impact, Payer Models, and Revenue Optimization
Understanding the relationship between pos 21 in medical billing and reimbursement is essential for healthcare organizations aiming to optimize revenue. Accurate coding not only drives payment outcomes but also ensures compliance with payer standards. Let's break down how pos 21 in medical billing directly affects your financial processes.
How POS 21 Influences Reimbursement Structures
POS 21 in medical billing designates inpatient hospital care, triggering Diagnosis Related Group (DRG) payment models. DRGs bundle hospital services into a single payment, which usually exceeds outpatient fee-for-service rates. This model incentivizes accurate documentation and coding, since hospital revenue for inpatient stays often surpasses what is received for similar outpatient care.
Consider a routine surgical procedure: billed as inpatient under POS 21 in medical billing, it qualifies for DRG-based reimbursement, potentially doubling payment compared to outpatient coding. The correct use of POS 21 in medical billing ensures your claims are routed for the highest appropriate payment, supporting your bottom line.
| Scenario | POS Code | Payment Model | Typical Reimbursement |
|---|---|---|---|
| Inpatient Surgery | 21 | DRG | Higher |
| Outpatient Surgery | 22 | Fee-for-Service | Lower |
Medicare, Medicaid, and Commercial Payer Rules
Medicare relies on DRG bundling for pos 21 in medical billing, enforcing strict criteria for inpatient admissions. Only services on the inpatient-only list qualify, and documentation must support medical necessity. Medicaid often mirrors Medicare’s standards, but reimbursement rates and qualifying criteria can vary by state.
Commercial payers introduce contractual nuances. Some require pre-authorization, while others have unique definitions of inpatient status. For all payers, improper use of pos 21 in medical billing can trigger audits and recoupments, so staying current with payer-specific rules is critical.
Revenue Cycle Management Strategies for POS 21 Claims
Efficient revenue cycle management (RCM) is vital for maximizing returns from pos 21 in medical billing. Begin with eligibility verification and pre-admission checks to reduce denials. Ensure billing and clinical teams collaborate to align documentation with coding. Monitor claims for edits and denials, and act quickly on payer feedback.
Leverage analytics to track trends and identify bottlenecks. Streamlined workflows, staff education, and regular audits drive improvement. For a deeper dive into how these processes support your financial health, review this Revenue cycle medical billing overview.
Compliance, Documentation, and Audit Readiness
Accurate pos 21 in medical billing is inseparable from strong compliance practices. Maintain audit-ready records for every inpatient claim. This includes detailed admission notes, care plans, and discharge summaries that clearly demonstrate medical necessity.
Responding promptly to payer documentation requests reduces payment delays and audit risks. Internal audits help identify gaps before external scrutiny. Avoid upcoding or misclassification, as errors can result in costly recoupments or penalties.
Optimizing Financial Outcomes with Expert RCM Support
Partnering with an experienced RCM service provider amplifies the benefits of pos 21 in medical billing. Skilled professionals verify inpatient admissions, ensure proper coding, and manage claims through every stage of the revenue cycle. This proactive approach lowers denial rates and accelerates cash flow.
B2B clients benefit from transparent reporting, advanced analytics, and industry expertise tailored to inpatient billing. The right RCM partner adapts to your systems, supporting compliance and revenue growth.
How Greenhive Billing Solutions Enhances POS 21 Revenue Cycle Management
Greenhive Billing Solutions specializes in managing pos 21 in medical billing for hospitals and healthcare organizations. Our team verifies inpatient admissions, aligns clinical documentation, and assigns correct codes to safeguard compliance.
We handle proactive denial management and appeals, reducing lost revenue. Transparent analytics provide actionable insights, while our specialty-specific expertise minimizes errors. By focusing on pos 21 in medical billing, we help clients maximize reimbursement and maintain regulatory standards.
Step-by-Step Guide to Using POS 21 Correctly: Chronological Billing Workflow
Navigating the correct use of pos 21 in medical billing requires a structured, sequential approach. Below is a practical, stepwise workflow designed for hospital and practice billing teams. By following each stage, you can reduce errors, improve compliance, and maximize reimbursement outcomes.
Step 1: Patient Admission and Eligibility Verification
The process begins with confirming a valid inpatient admission. For pos 21 in medical billing, ensure the physician has issued a formal admission order and documented the medical necessity for inpatient care.
Conduct real-time insurance eligibility and benefits verification before care is rendered. This step helps avoid downstream denials and payment delays. If your payer requires pre-authorization for inpatient stays, secure it and document approval in the patient record.
Record all admission details, including time, date, and admitting diagnosis, in both the EHR and billing system. For example, verifying coverage upfront for a complex surgery ensures your team can bill pos 21 in medical billing without costly rework.
Step 2: Clinical Documentation and Coding Alignment
Accurate documentation is the backbone of compliant pos 21 in medical billing. All progress notes, admission orders, and care plans must clearly reflect inpatient status and the intensity of services delivered.
Assign ICD-10, CPT, and HCPCS codes that directly correspond to the patient’s diagnoses and procedures performed during the inpatient stay. Cross-check these codes with the medical record to ensure consistency and completeness.
A robust documentation process supports claim acceptance and audit readiness. For instance, a well-documented acute heart failure admission can justify the use of pos 21 in medical billing, reducing the risk of claim denials.
Step 3: Claims Preparation and POS 21 Assignment
Once documentation is complete, select the correct place of service code on the claim form. For inpatient claims, pos 21 in medical billing must be entered on the UB-04 or CMS-1500, depending on payer requirements.
Include all supporting documents, such as admission summaries and physician orders, to substantiate inpatient status. This is also a critical stage to apply any relevant modifiers that clarify the circumstances of the care provided. For a deeper understanding of correct modifier use with POS codes, refer to Types of modifiers in medical billing.
A thorough claims preparation process ensures accurate and timely reimbursement for the full scope of inpatient services billed under pos 21 in medical billing.
Step 4: Claims Submission and Payer Communication
With claims prepared, submit them to payers using the appropriate electronic or paper channel. Monitor claim status closely, watching for payer edits or requests for additional information that often relate to pos 21 in medical billing.
Maintain proactive communication with payer representatives to resolve any ambiguities quickly. Respond promptly to inquiries, providing clarifications or supplemental documents as needed.
Timely and transparent communication can reduce payment cycle times and improve the likelihood of first-pass acceptance for claims using pos 21 in medical billing.
Step 5: Denial Management and Appeals Process
Denials related to pos 21 in medical billing are not uncommon, often stemming from insufficient documentation or misclassified admissions. Track all denied claims, identify recurring patterns, and investigate the root causes.
Gather additional documentation when necessary and submit appeals in accordance with payer guidelines. Strong clinical evidence and a clear demonstration of inpatient necessity can turn a denial into a successful payment.
Implement corrective actions based on denial trends to prevent future issues. For example, a hospital that reviews and appeals denied pos 21 in medical billing claims can recover significant revenue otherwise lost to administrative errors.
Step 6: Continuous Improvement and Staff Training
Continuous education is essential for minimizing errors with pos 21 in medical billing. Schedule recurring training sessions for billing and clinical staff to reinforce the latest payer requirements, documentation standards, and compliance strategies.
Review denial data regularly and update workflows to address gaps. Utilize analytics to benchmark performance against industry standards and set measurable goals for improvement. For in-depth guidance on compliant POS code usage, see Place of Service Codes Compliance.
By fostering a culture of learning and accountability, your organization can ensure continued accuracy and compliance in pos 21 in medical billing.
Advanced Tips, Compliance Trends, and Future Outlook for POS 21
Staying current with industry shifts is essential for any organization managing pos 21 in medical billing. Let us explore the latest trends, technology advancements, compliance priorities, and forward-looking strategies to ensure your inpatient billing remains accurate and profitable.
Emerging Trends in Inpatient Billing and POS 21
The landscape of pos 21 in medical billing is rapidly evolving. Payers are refining inpatient admission criteria and increasing scrutiny on short-stay claims. Hospitals must track regulatory updates, such as CMS initiatives that impact inpatient status reviews and DRG payments.
A major trend is the integration of advanced analytics, which payers use to identify outliers and potential compliance risks. Value-based care models are also shifting reimbursement priorities, making accurate pos 21 coding more critical than ever. For a broader perspective on how digital transformation and AI are fueling industry expansion, review the recent Medical Billing Market Growth insights.
Technology and Automation in POS 21 Billing
Technology continues to transform pos 21 in medical billing. EHR integrations streamline documentation and coding, reducing manual errors. Automated eligibility checks and claim scrubbing tools flag inconsistencies before submission, improving first-pass acceptance rates.
Professional revenue cycle teams leverage client-owned platforms to maximize efficiency. Outsourcing RCM services brings expertise in using analytics dashboards, ensuring each inpatient claim meets payer requirements. Automation not only increases speed but also supports compliance by providing audit trails and real-time reporting.
Compliance Hotspots and Audit Readiness
Compliance remains a central concern for pos 21 in medical billing. Auditors focus on areas such as short inpatient stays, observation versus inpatient status, and proper documentation of medical necessity. To mitigate audit risk, organizations should maintain thorough, up-to-date records for every admission.
Proactive internal audits help catch discrepancies before external reviews. Standardized protocols for documenting admission orders, physician notes, and care intensity support defensible claims. Being audit-ready is not just about avoiding penalties, but also about protecting your reputation and revenue.
Preparing for the Future: Best Practices for Sustained Success
Looking ahead, sustained success with pos 21 in medical billing depends on continuous adaptation. Regularly update staff on payer and CMS guideline changes. Invest in ongoing education and process refinement to ensure everyone understands the nuances of inpatient billing.
Building strong partnerships with experienced RCM service providers enables scalability and compliance. Track key performance indicators like denial rates and audit outcomes to guide improvement efforts. By staying agile and informed, your organization can optimize reimbursement and maintain compliance as industry standards evolve.
As you’ve seen, understanding and applying POS 21 correctly is crucial for accurate claims, compliance, and stronger reimbursement outcomes. Even with the best resources, it’s easy for small mistakes to add up and impact your bottom line. If you want expert guidance tailored to your practice and a chance to identify hidden opportunities for improvement, why not take the next step? Let’s work together to ensure your billing processes are as efficient and compliant as possible. You can Get Your Free Audit and gain valuable insights into your current POS 21 billing practices—no strings attached.