Orthopedic practices today face mounting financial and administrative pressures as healthcare regulations, payer rules, and patient expectations continue to evolve. Industry data shows that inefficient processes and billing errors result in significant revenue loss for practices each year.
Mastering orthopedic revenue cycle management is now critical for maintaining profitability, compliance, and operational efficiency. This comprehensive guide offers a step-by-step roadmap designed to help orthopedic practices optimize every stage of their revenue cycle.
Explore common challenges, proven solutions, best practices for each phase, the latest trends, and the value of partnering with expert RCM providers. Discover actionable strategies to streamline your operations, maximize reimbursements, and secure long-term financial success.
Understanding the Orthopedic Revenue Cycle: Key Components and Challenges
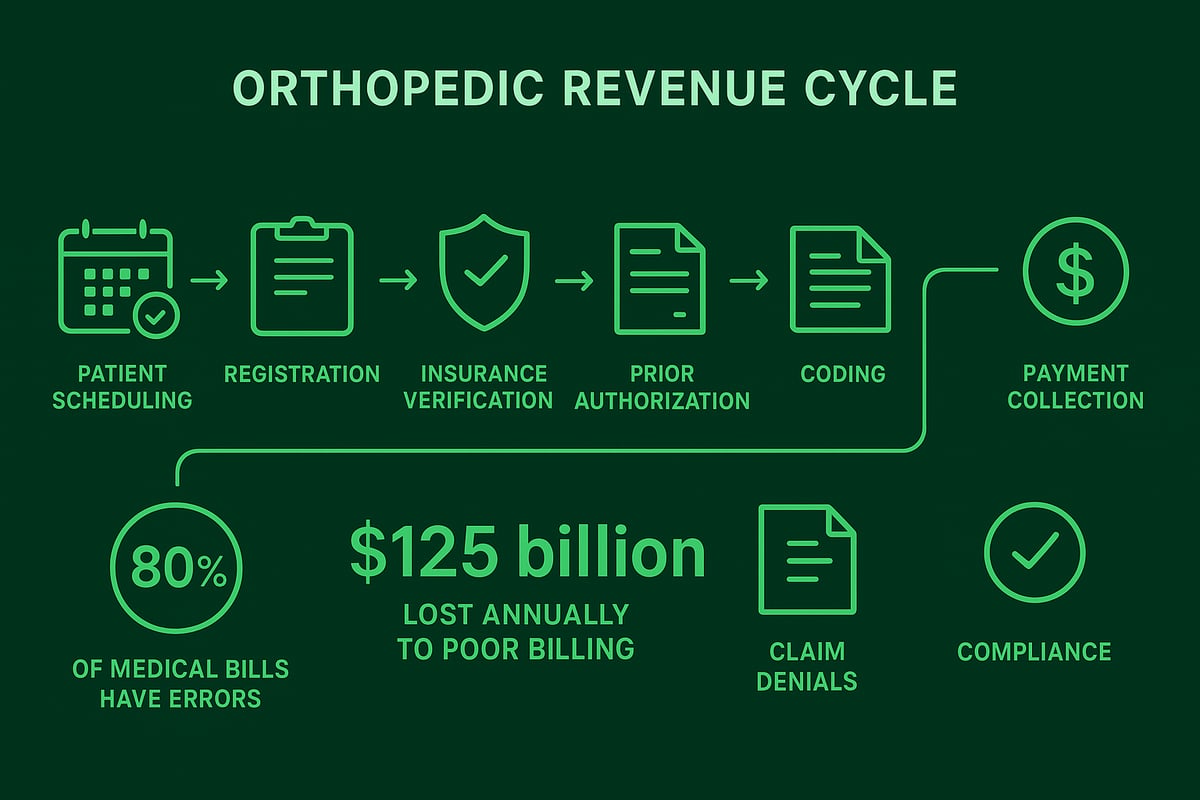
Orthopedic revenue cycle management covers every step from patient scheduling and registration to final payment collection. This cycle is the backbone of financial health for orthopedic practices, but it comes with unique complexities that demand specialized attention.
Orthopedics faces distinct challenges, such as high-volume surgical procedures, intricate coding requirements, and the frequent need for prior authorizations. These factors increase the risk of billing errors and claim denials if not managed with precision.
Major obstacles in orthopedic revenue cycle management include ongoing regulatory changes, shifting payer policies, staffing shortages, and technology gaps. In fact, up to 80% of medical bills contain errors, and inefficient billing practices cost US physicians an estimated $125 billion annually.
Common real-world setbacks include claim denials due to missing documentation and underpayments caused by incorrect coding. Such issues can severely disrupt cash flow, extend accounts receivable days, and drain valuable administrative resources. Practices must continuously monitor compliance and adapt to payer updates to avoid these pitfalls.
For a deeper understanding of the foundational processes involved, see this Revenue cycle medical billing overview, which outlines the essential steps and challenges of effective RCM.
Staying proactive at each stage of the revenue cycle is vital for orthopedic practices to maintain profitability, streamline workflows, and ensure long-term financial stability.
Step-by-Step Guide to Optimizing Each Phase of the Orthopedic Revenue Cycle
Optimizing orthopedic revenue cycle management requires precision at every step, from patient intake to payment posting. Each phase presents unique challenges, but by targeting improvements in workflow and communication, practices can maximize collections, reduce errors, and maintain compliance.
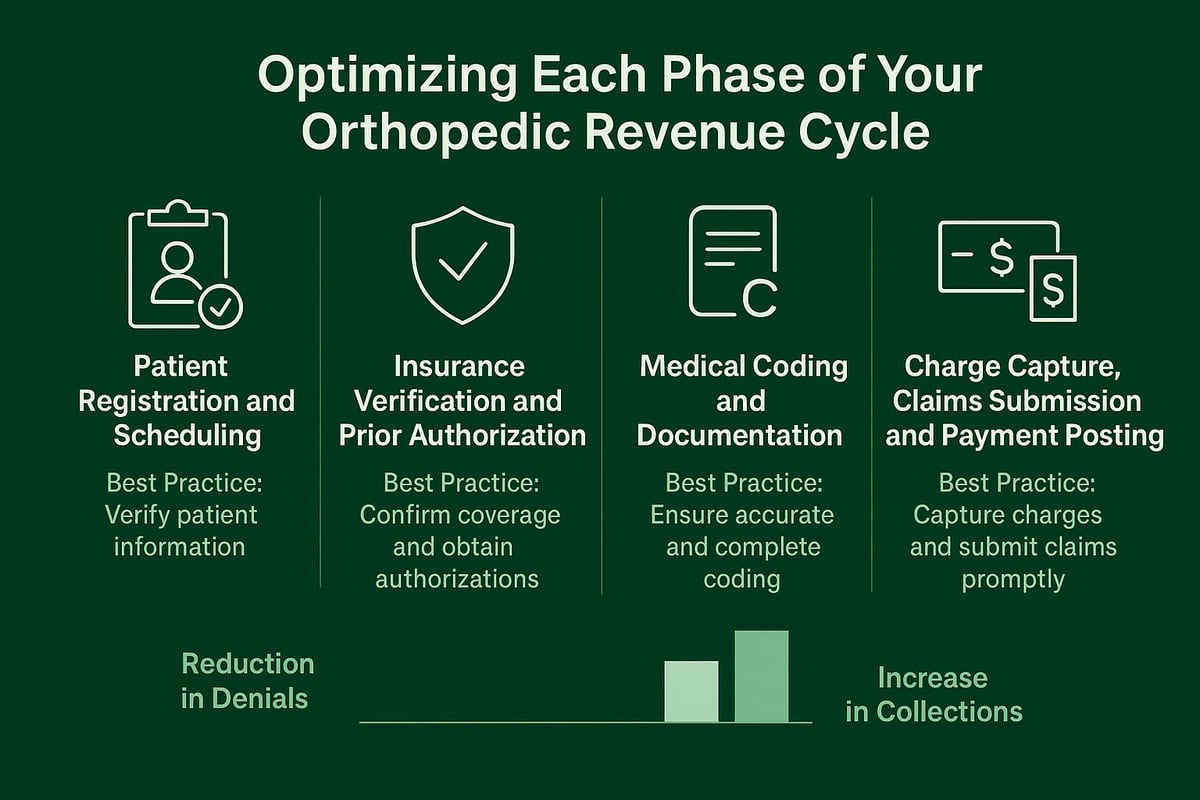
Patient Registration and Scheduling
Accurate patient data collection is the bedrock of effective orthopedic revenue cycle management. Ensure every registration captures correct insurance, demographics, and contact information. Missed insurance updates can lead to costly claim rejections and revenue loss.
- Use checklists for intake staff.
- Train regularly on documentation requirements.
- Verify insurance before scheduling.
A robust intake process minimizes denials and sets the stage for efficient downstream workflows.
Insurance Verification and Prior Authorization Management
Real-time insurance verification and proactive prior authorization are essential to orthopedic revenue cycle management. Delays or errors here cause denials and payment delays, impacting cash flow. Prior authorizations alone contribute to significant administrative costs in healthcare. Standardize workflows and consider dedicated staff or outsourcing for prior auth tasks. For more detailed best practices, see Insurance verification in medical billing.
Medical Coding and Documentation
Orthopedic coding (ICD, CPT, HCPCS) is complex and central to orthopedic revenue cycle management. Incorrect coding leads to underpayments and potential audits. Employ certified coders, offer ongoing training, and conduct periodic coding audits to ensure compliance and accuracy.
- Use double-checks for high-value claims.
- Regularly update staff on coding changes.
Accurate documentation supports appropriate reimbursement and compliance.
Charge Capture, Claims Submission, and Payment Posting
Timely charge entry and clean claims submission are critical for optimal orthopedic revenue cycle management. Automate routine tasks where possible, and reconcile payments to catch discrepancies early. The industry standard of 2.7 billing employees per physician highlights the workload involved.
- Implement error-checking tools.
- Post payments promptly.
- Follow up on underpayments without delay.
A streamlined process here reduces delays, improves cash flow, and supports financial health.
Managing Denials, Accounts Receivable, and Patient Collections
Claim denials are a persistent challenge in orthopedic revenue cycle management. Common causes include missing documentation, coding mistakes, and lapses in prior authorization. Each denied claim strains cash flow and increases administrative workload. To address these issues, practices should implement root cause analysis, timely appeals, and track denial trends. For deeper insight on effective denial resolution, review denial management in medical billing.
![]()
Effective accounts receivable management is central to orthopedic revenue cycle management success. High A/R days signal financial risk, while unresolved denials lower collections. Best practices include regular follow-up on outstanding claims, generating aging reports, and prioritizing high-value accounts. Proactive monitoring helps identify payment delays early and maintains a healthy cash flow.
For patient collections, transparency and flexibility are key. Clear, easy-to-understand billing statements, flexible payment plans, and open communication improve self-pay rates. Many practices find that outsourcing A/R management reduces average A/R days to the industry benchmark of 34 days, while also freeing staff to focus on patient care.
Leveraging Analytics, Reporting, and Compliance for Continuous Improvement
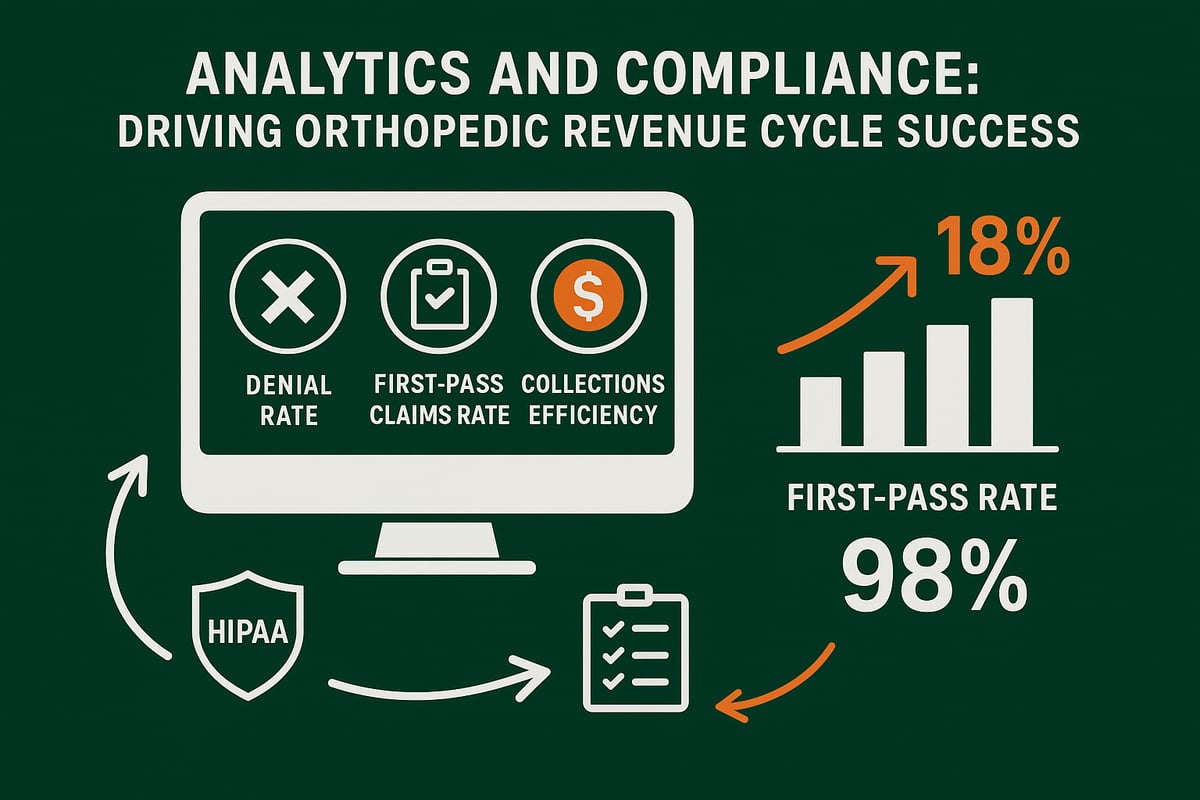
Harnessing real-time analytics and robust reporting is fundamental for effective orthopedic revenue cycle management. With dynamic dashboards, practices gain a clear view of vital performance indicators, such as denial rates and collections efficiency, enabling quick, data-driven decisions.
| KPI | Benchmark |
|---|---|
| First-Pass Claims Rate | 98% |
| Denial Rate | < 5% |
| Collections Efficiency | 95%+ |
Practices using advanced analytics often see an 18 percent increase in payments and a 98 percent first-pass claims rate. Accurate reporting uncovers bottlenecks, optimizes workflows, and pinpoints revenue leakage for proactive intervention. For a deeper dive into analytics and common obstacles, see Orthopedic RCM Challenges and Solutions.
Staying compliant with evolving regulations is just as crucial. Regular staff education and timely policy updates help maintain HIPAA compliance and adapt to payer rule changes. Scheduled revenue cycle assessments ensure that the orthopedic revenue cycle management process remains efficient and up to date.
Actionable reports not only inform business decisions but also support revenue forecasting and resource planning. Leveraging analytics allows practices to adjust staffing, negotiate with payers, and continuously refine workflows for optimal results.
Continuous improvement in orthopedic revenue cycle management depends on a strong foundation of analytics, rigorous compliance, and a commitment to adapting processes as the industry evolves.
The Strategic Advantage of Partnering with an Expert Orthopedic RCM Provider
Outsourcing orthopedic revenue cycle management brings a competitive edge to practices seeking financial health and operational efficiency. As the healthcare landscape becomes more complex, partnering with an expert RCM provider offers immediate access to deep specialty expertise, scalable staffing, and the latest industry technology.
Many practices struggle to keep up with billing complexities. In fact, 63% report staff shortages as a major challenge. By collaborating with an experienced RCM team, you close resource gaps and free up your in-house staff to focus on patient care.
Key benefits of an expert RCM partner:
| Benefit | Impact on Your Practice |
|---|---|
| Specialty billing expertise | Higher accuracy, fewer denials |
| Scalable staffing | Handles volume spikes effortlessly |
| Advanced tools & analytics | Real-time insight, better decisions |
| Compliance & transparency | Reduced risk, peace of mind |
| Proven results | Faster payments, improved cash flow |
When evaluating RCM partners, look for transparency, orthopedic-specific experience, and a strong compliance track record. Integrated services—such as eligibility checks, denial management, and analytics—ensure every stage of the revenue cycle is optimized.
Practices that leverage expert partners often see faster reimbursements, lower denial rates, and more predictable revenue. For 17 actionable tactics on maximizing results, explore these RCM Strategies for Orthopedic Practices.
Ultimately, a trusted RCM partner adapts quickly to regulatory and payer changes, positioning your practice for ongoing success with orthopedic revenue cycle management.
Future Trends and Best Practices in Orthopedic Revenue Cycle Management
Orthopedic revenue cycle management is evolving rapidly as payer policies, regulatory requirements, and patient financial responsibility continue to shift. Practices must stay agile, adopting best practices such as ongoing staff training, workflow automation, and routine revenue cycle audits to remain competitive.
Embracing technology and data-driven strategies is becoming essential. Real-time analytics, automated claim scrubbing, and robust reporting tools help practices identify revenue leaks and optimize performance. According to the US RCM Market Growth Forecast, the demand for advanced revenue cycle management solutions is expected to rise, reflecting this industry-wide transformation.
To stay ahead, orthopedic practices should focus on:
- AI-powered denial prediction and prevention
- Expanded telehealth billing capabilities
- Patient engagement and digital payment tools
Evaluating revenue cycle performance annually and seeking expert support when needed ensures processes remain adaptable and scalable. By prioritizing proactive management, leveraging specialized partnerships, and committing to continuous improvement, practices can secure long-term success in orthopedic revenue cycle management.
As you look ahead to 2026, optimizing your orthopedic revenue cycle isn’t just about staying compliant—it’s about ensuring your practice thrives. We’ve explored the key challenges, actionable strategies, and the real impact streamlined processes can have on your bottom line. If you’re ready to pinpoint hidden inefficiencies and discover where your revenue cycle can improve, why not take the next step? You deserve clear insights tailored to your practice’s unique needs. Let’s work together to maximize reimbursements and reduce administrative headaches—start with a Get Your Free Audit and see how much more your practice could achieve.