Insurance verification in medical billing has become increasingly complex for healthcare organizations today. Ensuring accurate verification is critical, as even small errors can lead to costly claim denials, delayed reimbursements, and unnecessary administrative work.
Incomplete or inaccurate insurance verification in medical billing puts both financial stability and operational efficiency at risk. When verification is handled properly, it leads to fewer denials, faster payments, and greater patient satisfaction.
This comprehensive guide will walk you step by step through the essentials of insurance verification in medical billing. You will learn the basics, the verification process, common challenges, compliance best practices, and future industry trends.
Understanding Insurance Verification in Medical Billing
Insurance verification in medical billing is a foundational step in the healthcare revenue cycle. It ensures that a patient's insurance details are accurate and up to date before any medical services are rendered. This process plays a critical role in determining whether claims are accepted by payers and how quickly reimbursements are processed.
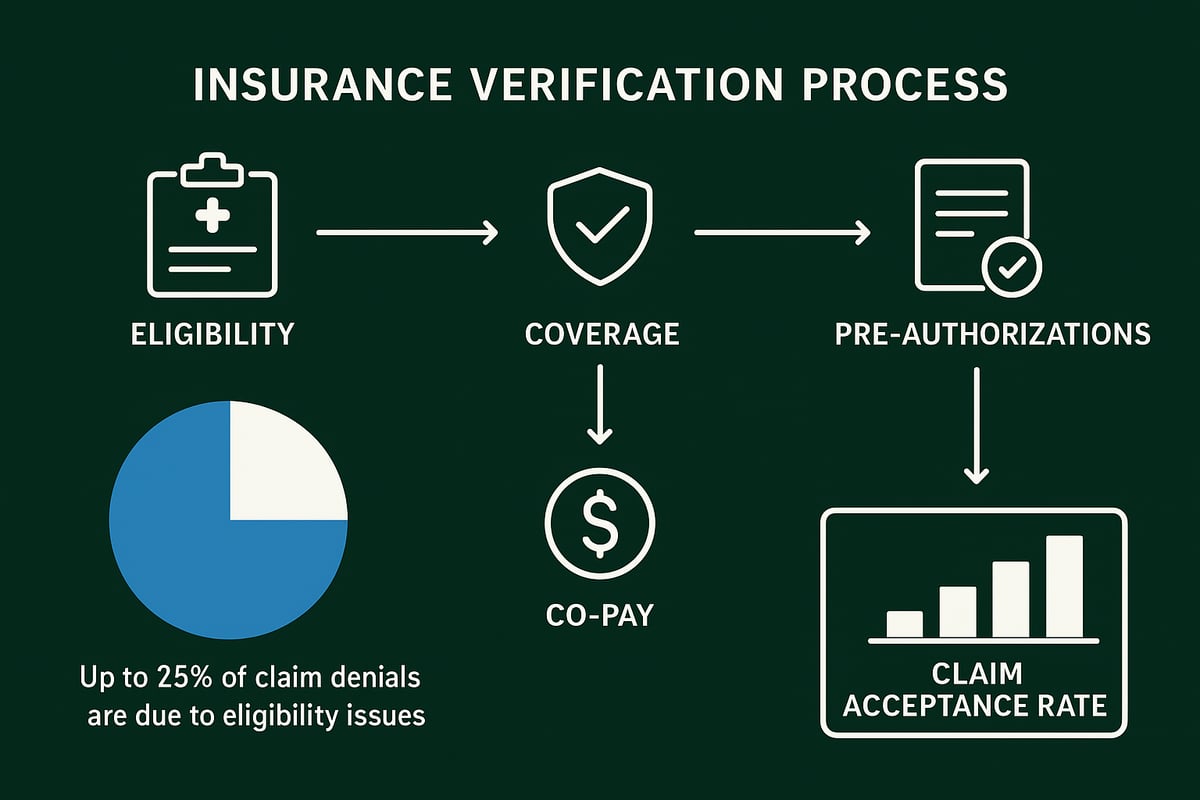
Healthcare organizations must verify several elements before patient visits. These include eligibility, coverage limits, co-pays, deductibles, and any required pre-authorizations. The table below summarizes key information typically checked during insurance verification in medical billing:
| Information Verified | Description |
|---|---|
| Eligibility | Is the policy active on the service date? |
| Coverage | What services are included or excluded? |
| Co-pay & Deductible | Patient’s financial responsibility |
| Pre-authorizations | Required approvals for specific procedures |
Missing or inaccurate insurance verification in medical billing can have serious consequences. Up to 25% of claim denials are linked to eligibility errors, leading to delayed payments and dissatisfied patients. These issues are common in busy practices, where incomplete or outdated patient details are often overlooked.
Verification methods vary. Manual processes involve phone calls or payer portals, while automated tools streamline checks and reduce human error. For example, a small clinic might rely on manual verification, while large multi-specialty groups often adopt automation to handle high patient volumes.
For a detailed overview of verification procedures, see the Insurance eligibility verification process. Mastering these steps helps healthcare providers avoid denials and maintain a healthy revenue cycle.
Step-by-Step Insurance Verification Process
Accurate insurance verification in medical billing is a multi-step process that demands attention to detail. Each step plays a critical role in ensuring claims are accepted, payments are timely, and patients have clarity on financial responsibilities. By following a structured approach, healthcare organizations can minimize errors and boost efficiency.
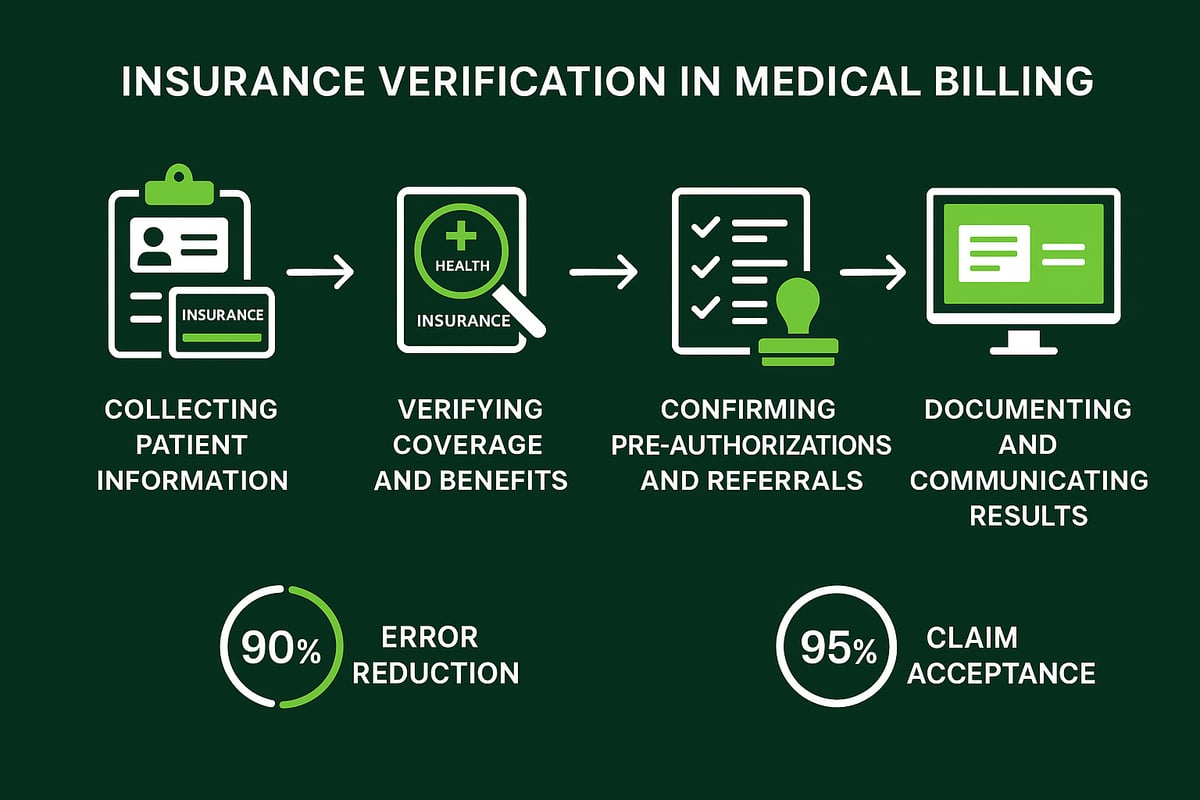
Collecting Patient Information
The insurance verification in medical billing process starts with collecting accurate patient details. Staff must gather demographic information and insurance data during scheduling and check-in.
It is essential to verify the insurance card, government-issued ID, and up-to-date contact details. Standardizing intake forms and checklists helps reduce data entry errors.
For example, clinics that require patients to submit documents before appointments see fewer claim rejections due to incorrect information. This proactive step lays the foundation for successful insurance verification in medical billing.
Verifying Coverage and Benefits
Next, staff confirm coverage and benefits directly with payers using online portals, phone calls, or clearinghouses. This step ensures eligibility for the scheduled service date and specific procedure.
Teams must identify any coverage limitations, exclusions, or high out-of-pocket costs. It is vital to clarify co-pays, deductibles, and any required patient payments before the visit.
By consistently verifying benefits, clinics lower the risk of claim denials and unexpected patient expenses. Accurate insurance verification in medical billing at this stage supports smoother revenue flow.
Confirming Pre-Authorizations and Referrals
Many procedures require prior authorization or a referral from a primary care provider. Staff should determine if approval is needed for each planned service, especially for high-cost imaging or specialist visits.
Obtaining and documenting these approvals prevents retroactive denials, which can disrupt cash flow. For detailed guidance on this step, refer to prior authorization services in billing.
Consistent follow-up with payers and maintaining proof of authorization are essential for robust insurance verification in medical billing.
Documenting and Communicating Verification Results
After completing the previous steps, it is crucial to record all findings in the EHR or practice management system. Clear documentation supports billing staff and providers when submitting claims.
Teams should communicate coverage status and patient responsibilities to both clinical and administrative personnel. Patients benefit from early updates about their expected costs and coverage.
Effective documentation and open communication close the insurance verification in medical billing loop, reducing misunderstandings and financial surprises.
Common Challenges in Insurance Verification
Insurance verification in medical billing presents ongoing challenges for healthcare organizations. Providers must navigate complex payer requirements and frequent updates, all while maintaining accuracy and efficiency.
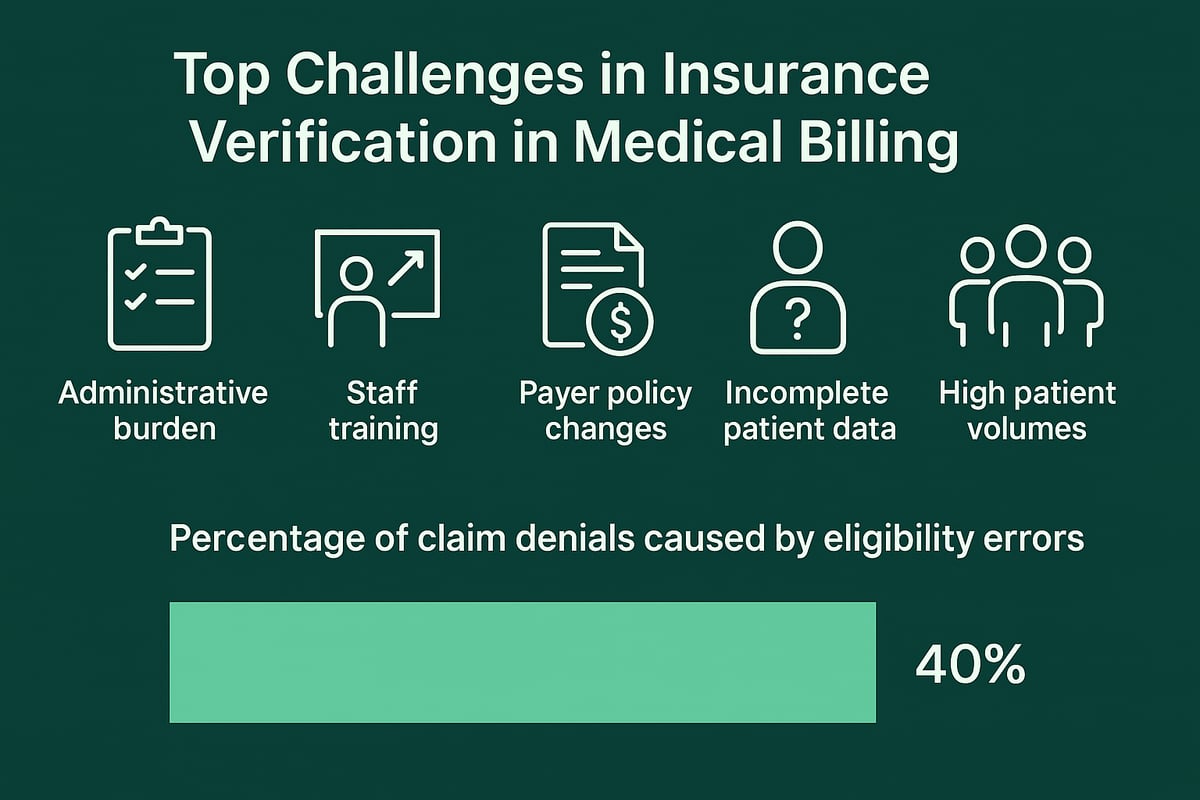
Common challenges include:
- High administrative workload and need for ongoing staff training.
- Constant changes in payer policies and inconsistent responses from insurers.
- Incomplete or outdated patient demographic and insurance information.
- Managing a surge in patient volume, especially with same-day appointments.
- Increased risk of denials when eligibility checks are missed during busy periods.
These obstacles can have a significant impact on the revenue cycle. Industry reports highlight that eligibility errors remain a leading cause of claim denials. According to Medical Billing Errors Statistics 2025, up to a quarter of denied claims are linked to insurance verification in medical billing issues, leading to delayed payments and increased administrative costs.
To address these challenges, healthcare organizations should consider:
- Cross-training staff for flexibility during high-volume periods.
- Conducting regular process audits to identify and correct gaps.
- Leveraging technology and electronic verification tools to streamline workflows.
Proactively managing these issues can reduce denials, improve cash flow, and ensure a smoother insurance verification in medical billing process for providers and patients alike.
Compliance and Best Practices in Insurance Verification
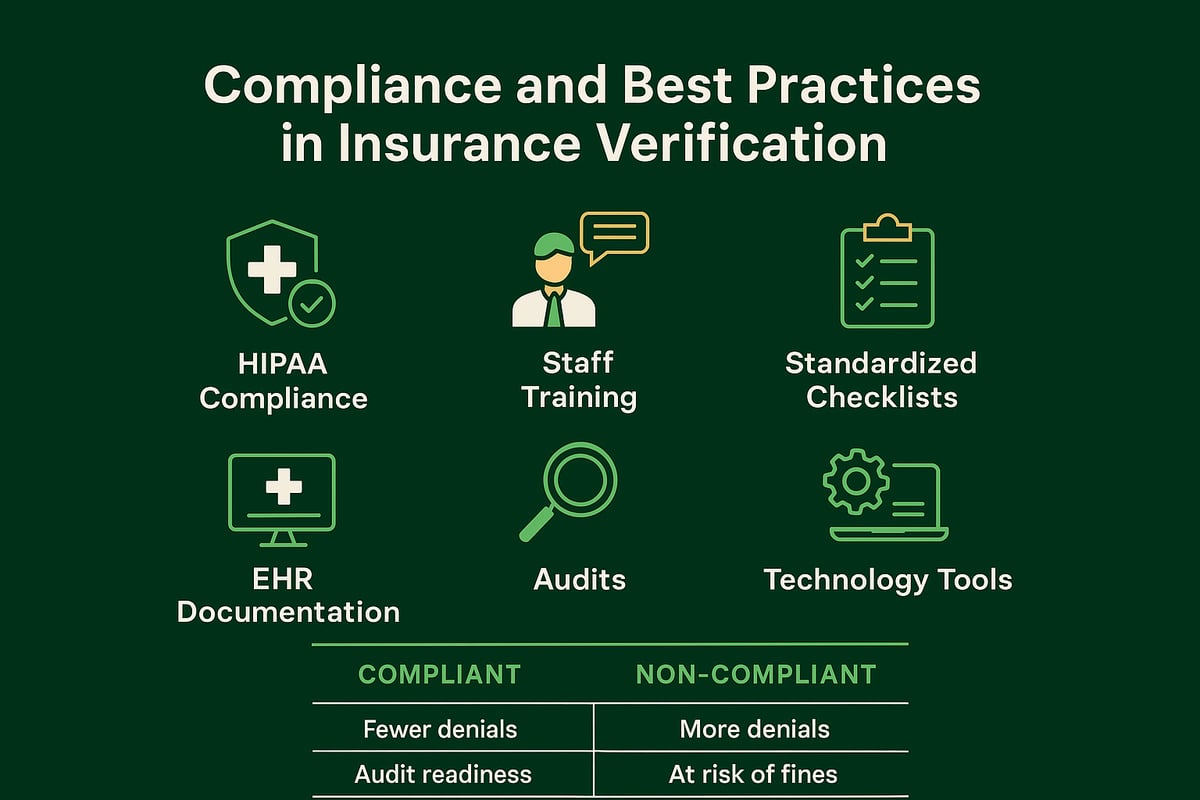
Maintaining compliance is essential for insurance verification in medical billing. Protecting patient data and adhering to HIPAA regulations should be foundational to every verification process.
Regular training keeps staff up to date on payer requirements and evolving protocols. Investing in education minimizes errors and ensures staff can respond to frequent policy changes with confidence.
Standardizing verification workflows is critical. Using detailed checklists for every patient encounter helps staff consistently capture all necessary information. This reduces the risk of missed eligibility checks or incomplete documentation.
Documenting every verification step in the patient record supports audit readiness. Ongoing audits and performance monitoring help identify gaps before they lead to denials or compliance penalties.
Leveraging technology, such as payer portals and electronic eligibility tools, streamlines processes and boosts accuracy. For practical strategies on optimizing workflows, see 7 Best Practices to Increase Medical Billing and Coding Accuracy.
A culture of compliance and accuracy not only reduces financial risk but also supports long-term revenue cycle health for healthcare organizations.
Future Trends in Insurance Verification
The landscape of insurance verification in medical billing is evolving rapidly as technology and payer expectations shift. Healthcare organizations are seeing several key trends transform the verification process.
- Real-time eligibility verification is becoming standard, allowing practices to confirm patient coverage instantly and reduce denials.
- AI-driven solutions are streamlining data entry, improving accuracy, and flagging inconsistencies before claims are submitted.
- Payer-provider collaboration is increasing, leading to more transparent and accessible coverage information for both staff and patients.
- Patient self-service verification tools are gaining traction, empowering individuals to check their own benefits and responsibilities.
By 2027, industry experts predict that more than 80% of providers will use automated verification tools. While technology reduces errors, skilled staff remain crucial for interpreting results and managing exceptions. Partnering with Eligibility verification services overview can also help practices stay ahead, integrating automation and expert support.
Staying proactive with these trends ensures insurance verification in medical billing continues to strengthen revenue cycle management and patient satisfaction.
As you’ve seen, mastering insurance verification isn’t just about reducing denials—it’s about protecting your revenue, freeing up staff time, and ensuring patients feel confident in your care. If you’re ready to streamline your processes and want expert guidance tailored to your practice, why not take the next step? We’re here to help you navigate the complexities of insurance verification, improve accuracy, and maximize reimbursements. Let’s talk about how Greenhive Billing Solutions can support your goals and set you up for success in 2026 and beyond. Book Your Free Consultation