Understanding medical billing charges in 2026 can feel overwhelming, with new rules, hidden costs, and changing technologies adding layers of complexity for healthcare providers.
This guide is designed to demystify medical billing charges, giving your practice the knowledge to make cost-effective, informed decisions. We will break down charge types, pricing models, key factors, industry trends, and proven strategies for cost optimization.
If you have ever faced uncertainty, surprise fees, or confusion about regulations, you are not alone. Discover how to achieve clarity, unlock savings, and confidently implement best practices for your billing process.
The Fundamentals of Medical Billing Charges in 2026
Medical billing charges are at the heart of every healthcare organization’s financial health. As we enter 2026, the landscape for healthcare providers is rapidly changing, with increased attention on accuracy, compliance, and transparency. Understanding how these charges are structured, categorized, and managed is the first step toward optimizing revenue and reducing unnecessary costs.
The Evolving Role of Medical Billing in Healthcare Administration
Medical billing charges have become the backbone of revenue cycle management for healthcare organizations. In 2026, billing is no longer a back-office task but a critical component that directly influences financial performance. Every clinical service must be accurately translated into a financial transaction, making precision more important than ever.
Payers are scrutinizing claims more closely, with new regulations tightening the requirements for coding and documentation. A single coding error can result in claim rejections or delays, impacting cash flow and increasing administrative workload. For example, improper coding in a high-volume practice can lead to thousands in lost revenue each month.
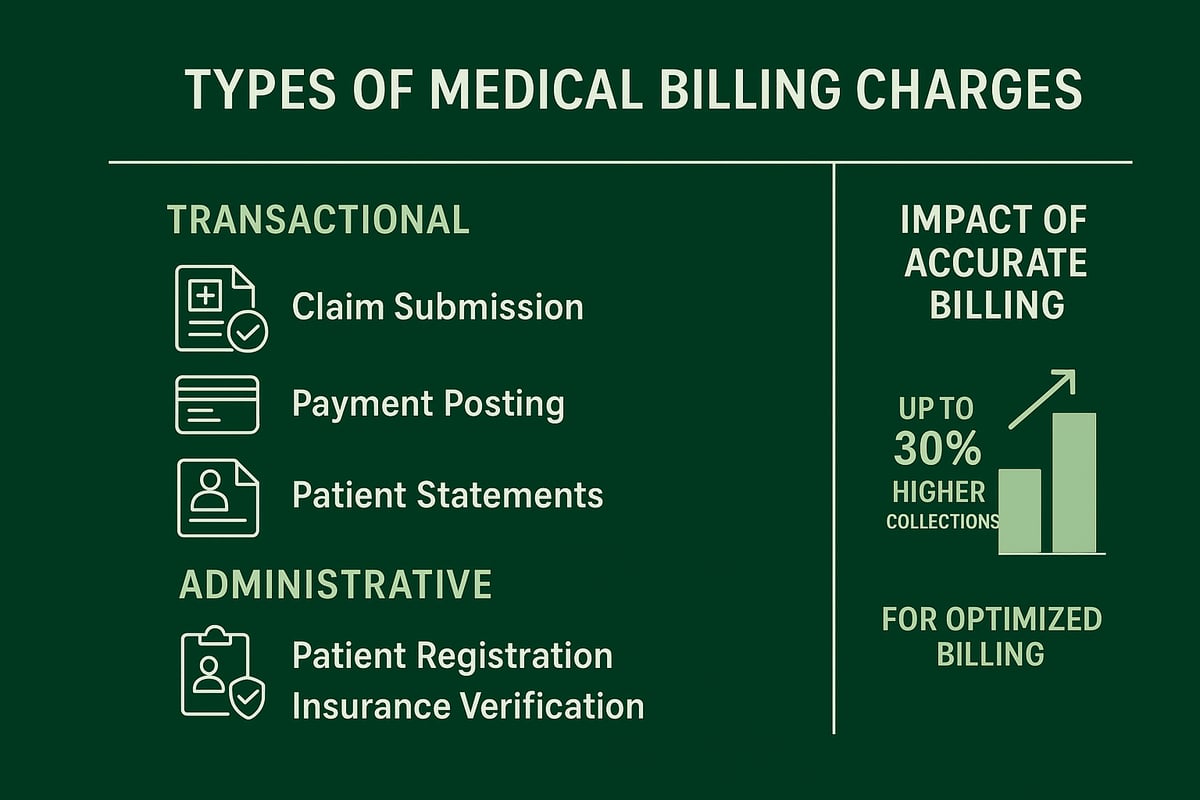
Data shows that practices with optimized medical billing charges processes see up to 30% higher collections compared to those with outdated or error-prone systems. This increased accuracy not only ensures timely payments but also supports compliance and audit readiness, both of which are essential for sustainable growth.
Types of Charges: Transactional vs. Administrative
Medical billing charges typically fall into two main categories: transactional and administrative fees. Transactional fees are incurred for each activity, such as claim submission, payment posting, or generating patient statements. Administrative fees, on the other hand, cover tasks like patient registration, insurance verification, and account management.
Understanding the cost structure is vital. Transactional fees are generally variable and may range based on claim volume or complexity, while administrative fees are often fixed but can fluctuate depending on practice needs. For example, integrating billing systems with EMRs may involve a one-time setup fee, but ongoing account management might have a monthly rate.
A comprehensive Medical billing costs breakdown can help healthcare providers see where their expenses are concentrated. By identifying and categorizing all medical billing charges, organizations can better manage their bottom line and avoid unexpected costs that erode profitability.
The Importance of Understanding Billing Charges for Providers
For healthcare providers, a clear grasp of medical billing charges is essential for sound financial planning. Charge transparency allows organizations to forecast expenses accurately and allocate resources efficiently. Overlooking ancillary or hidden fees can lead to budget overruns and compliance risks.
Transparent billing practices also support audit readiness, which is increasingly important given the regulatory environment in 2026. Providers who regularly audit their billing contracts often discover opportunities for savings, as seen in case studies where practices reduced costs by renegotiating terms or eliminating redundant services.
Ultimately, understanding medical billing charges means providers can make informed decisions, improve compliance, and achieve better financial outcomes.
Key Factors Influencing Medical Billing Charges
Understanding the drivers behind medical billing charges is crucial for healthcare organizations striving for cost efficiency. In 2026, these charges reflect a complex interplay of practice characteristics, service scope, regulatory demands, and technology adoption. By examining each factor, providers can pinpoint opportunities for savings and improved revenue cycle management.
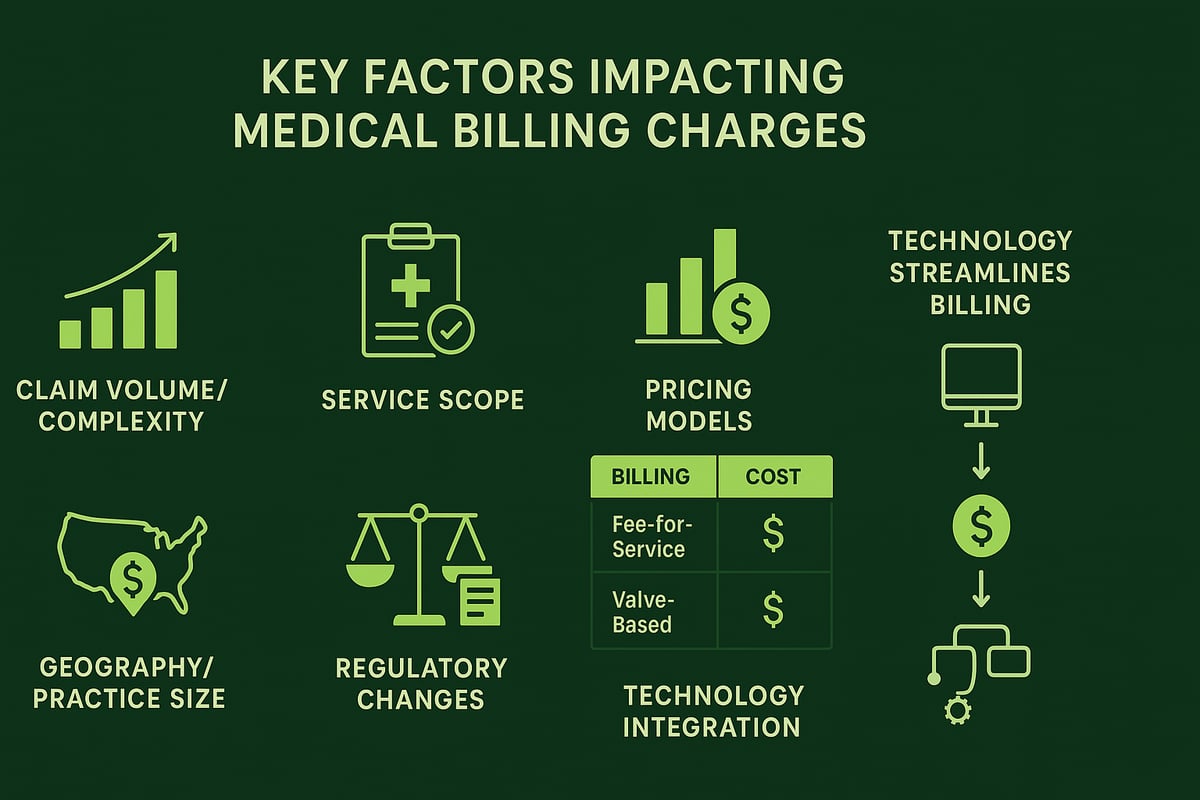
Claim Volume and Complexity
The number and complexity of claims processed each month are primary influencers of medical billing charges. Practices with higher claim volumes, such as multi-specialty clinics, typically face greater overall fees than smaller offices. Complexity comes into play with specialties that require detailed coding, frequent modifier usage, or handling multiple payer requirements.
For example, behavioral health claims often involve simpler codes compared to surgical specialties, where more intricate coding increases administrative effort. The process of charge entry, which is fundamental to generating accurate billing, also scales with both volume and complexity. To learn more about how this process underpins medical billing charges, see Charge entry in medical billing.
Scope of Services and Customization
The breadth of services included in your billing solution significantly shapes medical billing charges. Full-service options cover everything from claim submission to denial management, while a la carte solutions allow practices to select only the services they need. Add-ons such as patient billing, credentialing, or custom reporting may increase costs but also enhance value.
Customized workflows—tailored to the nuances of a specialty or the unique needs of a practice—often require additional setup or integration, impacting the final price. Understanding which services are essential versus optional helps practices control medical billing charges and avoid unnecessary spending.
Pricing Models and Fee Structures
Medical billing charges are directly tied to the pricing structure chosen. Common models include:
- Percentage of collections (typically 4–9%)
- Flat fee per claim ($4–$7)
- Hourly rates ($20–$30/hour)
- Hybrid models combining these elements
Each model offers distinct advantages. Percentage models align incentives but can be more expensive for high-volume practices. Flat fees provide predictability but may not account for claim complexity. Hybrid arrangements offer customization but can complicate budgeting. Comparing models side by side enables organizations to select the most cost-effective approach for their needs.
Geographic and Practice Size Considerations
Where a practice is located and its size play a notable role in determining medical billing charges. Urban regions with higher costs of living and increased market competition often command higher fees than rural areas. Larger practices may negotiate volume discounts, while smaller groups could face minimum monthly charges.
For example, a large metropolitan clinic may benefit from economies of scale, but a rural solo provider might pay a premium for specialized expertise. Understanding these geographic and size-based variations helps practices benchmark their own medical billing charges.
Regulatory and Payer Environment
Evolving regulations and payer policies add layers of complexity to medical billing charges. In 2026, updates to HIPAA, the No Surprises Act, and payer-specific rules have increased compliance requirements and administrative workload. New mandates for prior authorization or price transparency can drive up costs by demanding more staff time and stricter documentation.
Staying current with regulatory changes and payer guidelines is essential for keeping medical billing charges in check and avoiding costly errors or penalties.
Technology and Integration Requirements
The adoption of technology plays a dual role: it can add upfront costs but also drive long-term savings. Integrating billing workflows with EHR or practice management systems may involve initial setup fees, but automation and AI-powered tools reduce manual entry, minimize errors, and accelerate collections.
Practices leveraging advanced integration often see lower denial rates and faster reimbursements, offsetting the initial investment in technology. Evaluating the return on investment for these enhancements is key to optimizing medical billing charges.
Medical Billing Pricing Models Explained
Understanding medical billing charges is crucial for healthcare organizations seeking to optimize revenue and manage costs. The pricing model you choose directly impacts your financial predictability, collections, and overall operational efficiency. In 2026, several billing structures have become standard, each with unique advantages, challenges, and cost implications.
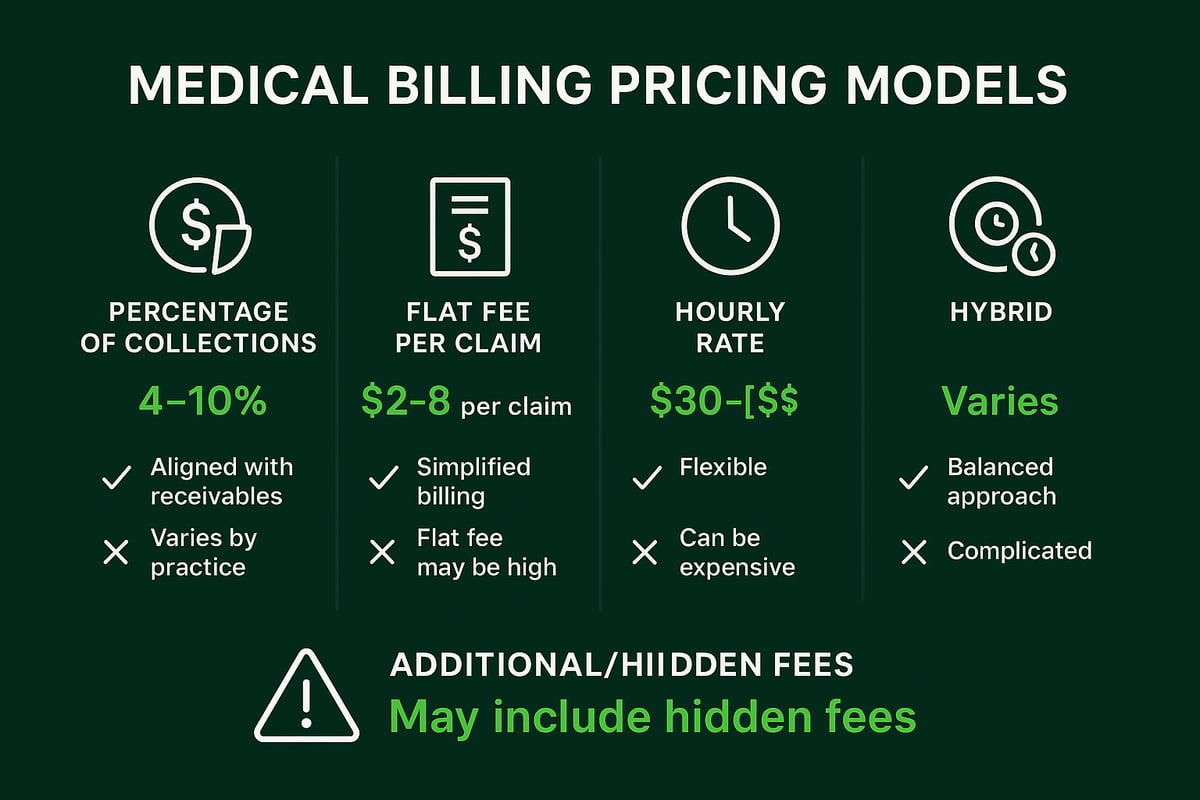
Percentage of Collections Model
The percentage of collections model remains a popular choice for medical billing charges in 2026, especially among practices seeking alignment between billing company incentives and collections performance. Here, the billing service earns a set percentage of the total revenue collected on your behalf.
Typical rates range from 4% to 10% of collections, depending on specialty, claim volume, and complexity. This model encourages billing partners to maximize reimbursements, as their earnings are tied to your success.
Pros:
- Aligns incentives with your revenue growth.
- Scales up or down with practice size.
- Often includes comprehensive services.
Cons:
- Can lead to higher costs as collections increase.
- May prioritize high-value claims over smaller ones.
For example, a practice collecting $100,000 monthly would pay $4,000 to $9,000 in medical billing charges under this model. Given current industry trends and the medical cost trend projected at 8.5% in 2026, it is important to assess whether this structure remains the most cost-effective for your organization.
Flat Fee Per Claim Model
The flat fee per claim model offers predictable medical billing charges, making budgeting straightforward for many healthcare groups. Under this structure, you pay a fixed fee for each claim submitted, regardless of the reimbursement amount.
Typical fees range from $4 to $7 per insurance claim, with lower rates ($1 to $3) often available for patient claims. This model is ideal for practices with stable claim volumes and less variability in service complexity.
Pros:
- Transparent, easy-to-understand billing.
- Facilitates accurate monthly financial planning.
- Particularly suitable for high-volume, routine practices.
Cons:
- May not account for claim complexity.
- Potential for overpaying on simple claims or underpaying on complex ones.
For example, submitting 500 claims per month at $5 per claim results in $2,500 in monthly medical billing charges. Practices must monitor claim mix to ensure fair value.
Hourly Rate Model
Some providers opt for an hourly rate model when they require specialized or intermittent billing support. In this arrangement, the billing service charges a set hourly fee, typically between $20 and $30 per hour, for time spent managing your billing tasks.
This model is often used for complex claim follow-up, appeals, or temporary coverage during staffing gaps. It provides granular insight into how time is spent on your account.
Pros:
- Pay only for actual work performed.
- Detailed cost breakdowns possible.
Cons:
- Difficult to predict total monthly spend.
- Risk of inefficiency if processes are not streamlined.
For instance, resolving a batch of complex denials might require several hours, resulting in variable monthly medical billing charges. This model works best when billing needs are sporadic or highly specialized.
Hybrid Pricing Models
Hybrid pricing models combine elements of the above structures to provide tailored solutions for diverse practice needs. A hybrid approach might involve a flat fee for routine claims, with a percentage applied to collections above a certain threshold, or hourly billing for specific add-on services.
These models are increasingly popular among multi-specialty groups or organizations with fluctuating claim volumes. Hybrid models offer flexibility but can be more complex to manage and audit.
Pros:
- Customization to fit unique workflows.
- Can balance cost control with incentive alignment.
Cons:
- Complexity in tracking and reconciling charges.
- May require more frequent contract reviews.
For example, a practice might pay a flat monthly fee for standard claims processing, then a percentage of collections for specialized services, optimizing their medical billing charges for both predictability and performance.
Additional and Hidden Fees
Beyond the primary pricing models, practices must remain vigilant about additional and hidden medical billing charges. Common extra costs include:
- Setup and Integration Fees: One-time charges for onboarding or connecting your systems.
- Clearinghouse Fees: Per-claim or monthly charges for electronic data interchange.
- Monthly Minimums: Required minimum spend, either as a flat rate or percentage.
- Hidden Charges: Fees for patient statements, claim resubmissions, or data backups.
A careful contract review is essential to avoid unexpected expenses and ensure full transparency. Practices that regularly audit their billing agreements are better positioned to identify and eliminate unnecessary medical billing charges, supporting long-term financial health.
Specialized Services and Their Impact on Billing Charges
Specialized services are a significant driver behind medical billing charges in 2026. For healthcare organizations, understanding these service components is crucial for managing costs and maximizing revenue.
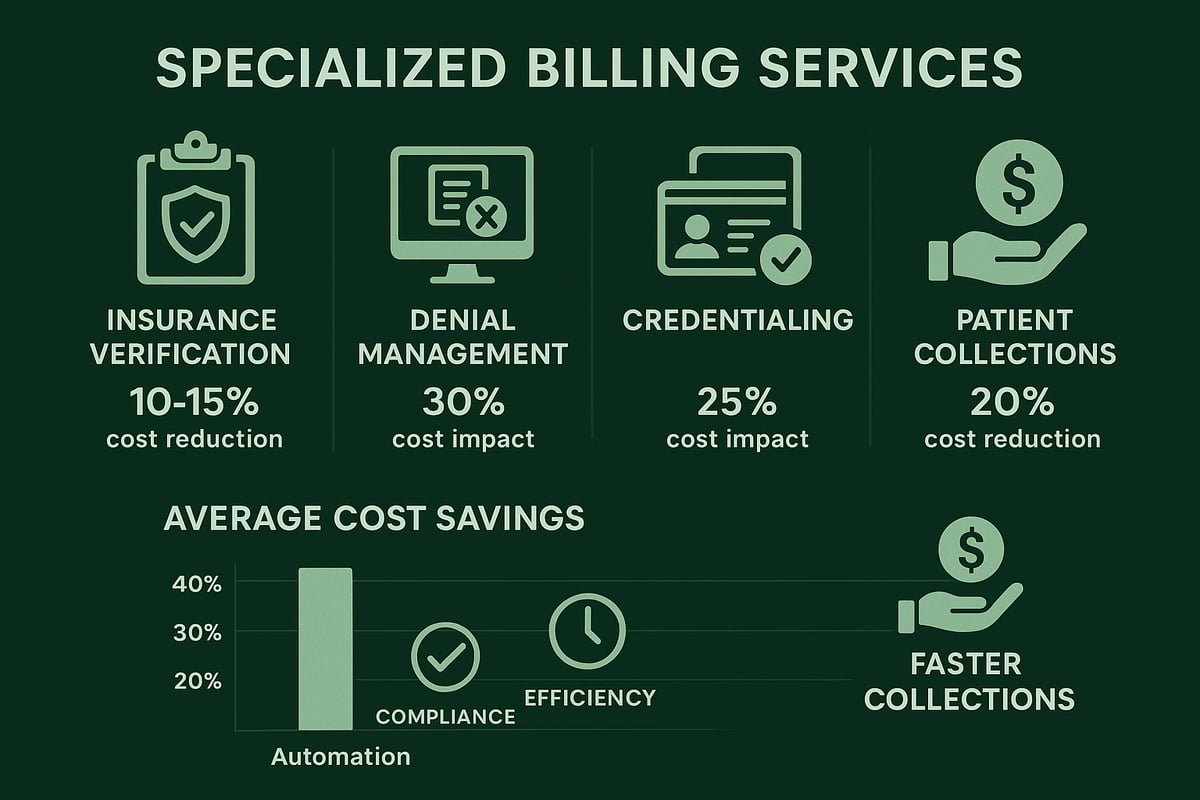
Insurance Eligibility Verification and Prior Authorization
Insurance eligibility verification is a frontline defense against denied claims, directly affecting medical billing charges. By confirming patient coverage and securing prior authorizations upfront, practices minimize claim denials and avoid costly rework.
Automated verification solutions often come bundled with billing services, or as a separate line item. Typical fees range from $2 to $5 per verification. Practices leveraging automation report up to 20% fewer denials, which translates to significant savings on overall medical billing charges.
- Upfront eligibility checks for every patient visit
- Automated vs. manual processes and their cost differences
- Reduction in denied claims and administrative burden
Clear workflows and technology adoption help reduce hidden costs tied to eligibility and authorization tasks.
Denial Management and Appeals
Denial management is critical for controlling medical billing charges. Practices routinely lose 5 to 10 percent of revenue to unresolved claim denials, making efficient management essential.
Outsourcing denial management can be structured as a fixed monthly fee, per-claim charge, or as part of a bundled RCM package. In-house teams require investment in training and technology, while outsourcing offers scalable expertise and rapid turnaround.
- Ongoing denial tracking and root cause analysis
- Appeals submission and follow-up protocols
- Cost-benefit of outsourcing vs. internal resources
Effective denial management not only recovers lost revenue but also reduces the administrative load on staff, keeping medical billing charges predictable.
Credentialing and Provider Enrollment
Credentialing new providers and maintaining payer enrollments have a direct impact on medical billing charges. Without timely credentialing, claims may be denied or delayed, leading to revenue gaps.
Fees for credentialing can be one-time or recurring, often determined by provider type and payer requirements. Outsourced credentialing services streamline the process, improve acceptance rates, and minimize costly errors. For more details on common fee structures and best practices, see Credentialing and provider enrollment fees.
- Initial provider enrollment and re-credentialing cycles
- Documentation and payer communication requirements
- Impact of delays on cash flow and claim acceptance
A proactive credentialing strategy ensures continuous revenue and helps control medical billing charges.
Patient Billing and Collections
Patient billing and collections represent a growing portion of medical billing charges, especially as patient financial responsibility increases. Charges may include statement processing, payment posting, and follow-up outreach.
Clear, patient-friendly billing communications can reduce accounts receivable days and lower bad debt rates. Practices using automated reminders and transparent billing see collections improve by up to 15 percent.
- Automated statement generation and payment reminders
- Options for online and mobile payments
- Reducing administrative costs with streamlined workflows
Optimizing patient billing processes is essential for keeping medical billing charges in check and maintaining healthy cash flow.
Trends and Innovations Impacting Medical Billing Charges in 2026
The landscape of medical billing charges is rapidly evolving, driven by breakthrough technologies, shifting regulations, and new service models. Healthcare organizations must keep pace to optimize costs, ensure compliance, and maximize revenue. Let's explore the most significant trends shaping medical billing charges in 2026.
Automation, Artificial Intelligence, and Data Analytics
In 2026, automation and AI are transforming how organizations manage medical billing charges. AI-powered coding tools minimize manual entry errors and accelerate claim submission, resulting in fewer denials and faster reimbursements. Predictive analytics help practices anticipate claim outcomes and forecast revenue, enabling more strategic decision-making. According to AI’s impact on medical billing efficiency, practices using AI solutions achieve up to a 25% reduction in claim rework. This shift not only streamlines billing workflows but also lowers administrative costs, making automation essential for staying competitive in the evolving billing landscape.
Regulatory Compliance and Transparency Requirements
Regulatory changes are a major driver of medical billing charges in 2026. New rules require providers to ensure complete transparency in billing, disclosing all potential fees to patients upfront. Updates to the No Surprises Act and enhanced HIPAA requirements are increasing documentation demands and audit scrutiny. As outlined in the CMS 2026 growth rates report, these changes directly impact cost structures and reimbursement rates. Practices must invest in compliance training and adapt processes to avoid penalties, which can affect both direct billing expenses and overall revenue cycle performance.
Outsourcing vs. In-House Billing: Cost and Efficiency Comparison
Choosing between outsourcing and in-house billing is a critical decision for controlling medical billing charges. Outsourcing to specialized RCM providers can reduce costs by up to 30% for medium-sized practices, thanks to lower overhead and access to expert staff. In-house teams, while providing direct control, often require significant investments in software, training, and ongoing staff development. Consider the following comparison:
| Billing Model | Average Annual Cost | Pros | Cons |
|---|---|---|---|
| Outsourcing | Lower (by 30%) | Expertise, scalability | Less on-site control |
| In-House | Higher | Direct oversight | Higher overhead, training |
Evaluating these models helps organizations align medical billing charges with their operational goals.
Customization and Specialty-Specific Billing
The demand for customized, specialty-specific billing services is on the rise. Practices in fields like cardiology, orthopedics, and behavioral health face unique coding challenges and complex payer requirements, which influence medical billing charges. Tailored RCM solutions address these nuances, reducing denial rates and increasing collections. For instance, a cardiology group working with specialists familiar with intricate procedures reported significantly fewer claim rejections. As specialty billing expertise becomes more accessible, providers can optimize revenue while ensuring compliance with ever-evolving payer policies.
Integration with Practice Management and EHR Systems
Seamless integration between billing services and client-owned EHR or practice management systems is critical for minimizing errors and controlling medical billing charges. Integrated platforms eliminate duplicate data entry, reduce claim delays, and speed up the revenue cycle. While initial setup or integration fees may apply, the long-term benefits include improved workflow efficiency and fewer billing mistakes. Practices leveraging integrated solutions report up to a 15% reduction in billing cycle times, supporting both cost savings and enhanced patient satisfaction.
Staying ahead of these trends empowers healthcare organizations to manage medical billing charges more effectively, drive operational efficiency, and remain compliant in a rapidly changing environment.
Actionable Strategies for Managing and Reducing Medical Billing Charges
Effectively managing medical billing charges requires a proactive and strategic approach. By implementing the following best practices, healthcare organizations can achieve greater clarity, cost control, and operational efficiency.
Conducting Regular Billing Audits
Routine billing audits are essential for identifying unnecessary or duplicate medical billing charges. By reviewing contracts and invoices, organizations can uncover hidden fees and benchmark against industry standards. Audits also support compliance and prepare practices for regulatory scrutiny.
Leveraging resources such as Denial management in medical billing can help providers pinpoint claim denials and optimize revenue cycle performance. Regular audits not only reduce expenses but also foster transparency and trust with stakeholders.
Negotiating Contracts and Fee Structures
Negotiating the terms of your medical billing service agreements plays a pivotal role in controlling medical billing charges. Healthcare providers should seek clarity on all fee components, from setup and transaction fees to bundled services.
Stay informed about regulatory changes, such as those highlighted in the 2026 outpatient billing changes overview, to gain leverage during contract discussions. Volume discounts and performance-based pricing can also yield long-term savings.
Leveraging Technology and Automation
Implementing automation tools streamlines workflows and reduces manual intervention, directly impacting medical billing charges. Automated claim scrubbing, eligibility verification, and payment posting all minimize errors and speed up collections.
Partnering with an RCM service provider that integrates seamlessly with your existing platforms ensures optimal efficiency. Automation not only lowers operational costs but also improves accuracy and compliance.
Staff Training and Compliance
Continuous training for billing and coding staff is crucial. Up-to-date knowledge of coding standards, payer requirements, and regulatory updates reduces costly mistakes and compliance risks.
Certified billing professionals are more likely to identify potential issues early, preventing revenue loss. Investing in staff development pays dividends through improved claim acceptance and fewer denials.
Monitoring Key Performance Indicators (KPIs)
Tracking KPIs such as denial rates, days in accounts receivable, and collection percentages is vital for managing medical billing charges. Analytics tools can reveal trends and areas for improvement.
By leveraging insights from denial management solutions, providers can take corrective action quickly. Regular KPI monitoring supports data-driven decisions and ongoing cost optimization.
Choosing the Right RCM Partner
Selecting a reputable RCM partner is one of the most impactful ways to control medical billing charges. Evaluate providers based on transparency, expertise, and flexibility in adapting to your systems.
A strong partner delivers measurable results, such as higher net collections and fewer compliance issues. Prioritize firms with a proven track record and clear communication to maximize your revenue cycle efficiency.
Understanding medical billing charges in 2026 is no small feat, especially with evolving regulations and so many moving parts impacting your bottom line. If you want to take control, improve transparency, and ensure you’re not leaving money on the table, having an expert ally makes all the difference. We’re here to help you navigate every fee, contract, and compliance update, so you can focus on patient care while optimizing your revenue cycle. If you’re ready for clear answers and tailored solutions, let’s talk about your practice’s unique needs—Book Your Free Consultation.