In 2026, the stakes for getting charge entry in medical billing right have never been higher. Financial losses, compliance risks, and denied claims can all stem from a single error, putting healthcare organizations’ revenue and reputation at risk.
This comprehensive guide is designed to help B2B healthcare leaders master charge entry in medical billing, providing a clear, step-by-step approach for lasting success.
You will discover the fundamentals, essential steps, and expert strategies to boost accuracy, avoid common pitfalls, and stay ahead of evolving regulations and technology.
Take action now to streamline your charge entry process and secure stronger financial outcomes for your practice or organization.
Understanding Charge Entry in Medical Billing
Charge entry in medical billing is the process of recording and entering charges for healthcare services rendered to patients. This foundational step ensures that every service provided is accurately captured and prepared for claim submission. When completed with precision, charge entry in medical billing drives timely reimbursements and healthy cash flow for healthcare organizations. Any error, such as a missed or incorrect charge, can cause a claim to be rejected or delayed, directly impacting revenue. For example, if a provider omits a procedure from the documentation, that service goes unbilled, resulting in lost income.
Definition and Purpose of Charge Entry
At its core, charge entry in medical billing involves translating the care delivered during a patient encounter into billable charges. It bridges the gap between clinical care and financial reimbursement. This step is critical, as it sets the stage for the entire billing process. Accurate charge entry in medical billing ensures providers receive payment for their services, while inaccuracies can trigger claim denials and disrupt revenue streams. For instance, submitting a claim with an incorrect procedure code may result in immediate rejection by the payer, requiring costly and time-consuming follow-up.
The Role of Charge Entry in Revenue Cycle Management
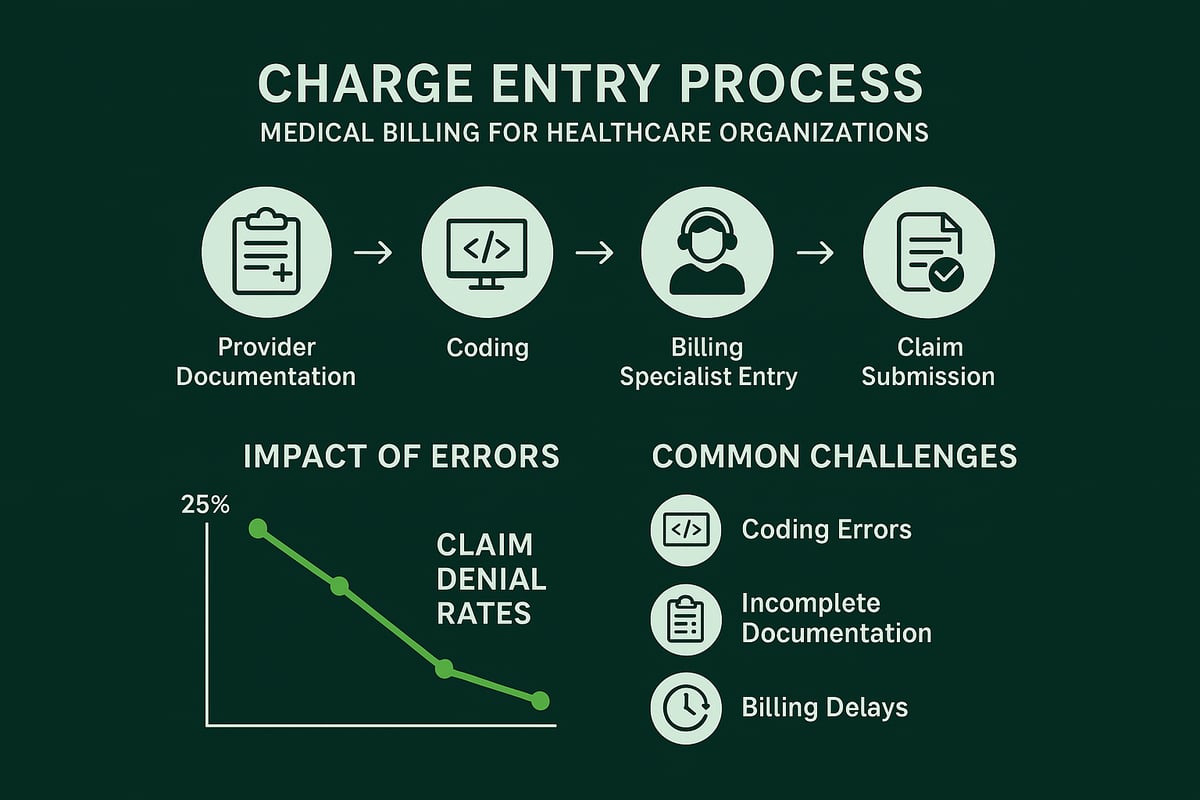
Charge entry in medical billing connects the clinical and administrative aspects of healthcare operations. It initiates the revenue cycle by transferring details from patient encounters into the billing system. This information flows through downstream processes including claim submission, payment posting, and accounts receivable management. A typical workflow starts with the provider’s documentation, moves to charge entry in medical billing, and continues until reimbursement is received. Errors at this stage can ripple throughout the revenue cycle, causing delays and increasing the risk of lost revenue. Competitor articles consistently highlight accurate charge entry as essential for achieving timely payments and minimizing denials.
Key Stakeholders and Responsibilities
Several stakeholders participate in charge entry in medical billing. Providers supply the clinical documentation, coders translate that documentation into standardized codes, and billing specialists input the charges into the billing system. Some organizations handle charge entry in-house, while others partner with revenue cycle management experts for greater efficiency. Collaboration between clinical and billing teams is vital to ensure all relevant information is captured accurately. For example, a provider’s thorough and timely documentation feeds directly into the charge entry process, reducing the chance of errors and omissions.
Common Challenges and Industry Data
Despite its importance, charge entry in medical billing faces several challenges. These include incomplete provider documentation, coding errors, and delayed data entry. Industry studies indicate that up to 30 percent of claims are denied due to charge entry errors, leading to significant rework and lost revenue. As new codes and payer rules are introduced in 2026, the complexity of charge entry in medical billing continues to grow. According to Medical Billing Errors Statistics 2025, the financial impact of billing errors underscores the need for a structured, stepwise approach to ensure accuracy and compliance.
Essential Steps in the Charge Entry Process
Navigating the charge entry in medical billing process requires a precise, methodical approach. Each step builds on the previous, ensuring accuracy and compliance at every stage. Mastering these steps is crucial for healthcare organizations aiming to optimize revenue, minimize denials, and maintain regulatory standards.

Step 1: Collecting Complete Encounter Information
The foundation of charge entry in medical billing lies in gathering comprehensive encounter details. Providers must document every service, diagnosis, and procedure performed. This information includes patient demographics, insurance details, and clinical notes.
Accurate documentation is essential for downstream processes. Missing information, such as an incomplete birthdate or omitted insurance policy number, can result in claim denials. Source documents might include EHR (Electronic Health Record) entries, encounter forms, or superbills.
Best practices involve standardized templates and checklists. For instance, a provider might use a digital form prompting for every data element required. Regular audits can identify recurring gaps in encounter documentation.
A practical example: If a patient's insurance information is outdated or their service date is left blank, the claim will likely be rejected, delaying reimbursement. Thorough, complete information at this stage sets the tone for error-free charge entry in medical billing and helps prevent revenue leakage.
Step 2: Verifying Insurance Eligibility and Authorization
Insurance verification is a critical safeguard in charge entry in medical billing. Before charges are entered, billing teams must confirm that a patient’s insurance is active and covers the planned services. Failing to verify eligibility or secure prior authorization can lead to outright claim denials.
The process involves real-time eligibility checks through payer portals or integrated EHR systems. If a procedure requires prior authorization, documentation must be obtained and attached to the patient record. For more detailed guidance on best practices in this area, see Insurance Authorization in Medical Billing.
Industry statistics reveal that up to 20 percent of denials stem from eligibility or authorization problems. For example, if a patient’s insurance expired last month and this goes unnoticed, the charges will be unpaid. By prioritizing this step, organizations can significantly reduce denials and streamline charge entry in medical billing.
Step 3: Accurate Medical Coding (CPT, ICD-10, HCPCS)
Assigning the appropriate codes is a pivotal part of charge entry in medical billing. Coders translate provider documentation into CPT, ICD-10, and HCPCS codes, which determine reimbursement. Using current and correct codes, especially with 2026 updates, is essential to prevent denials.
Certified coders play a vital role in this process. They review clinical notes and select codes that accurately reflect the services rendered. Automated claim scrubbers can flag mismatches or outdated codes, reducing errors before submission.
Consider a scenario where an outdated CPT code is used for a new procedure. The payer will deny the claim, requiring rework and delaying payment. Periodic coding audits and ongoing education ensure that staff remain proficient and compliant. This commitment to precision supports a robust charge entry in medical billing workflow.
Step 4: Charge Capture and Entry into Billing System
Once coding is complete, charges must be accurately entered into the billing system. Charge entry in medical billing can be performed manually or through EHR integration and specialized charge capture tools. The goal is to record every service without omissions or duplications.
Billing specialists should double-check for missing or duplicate charges. Assigning the correct fee schedule is also critical, as discrepancies can lead to underbilling or overbilling. Checklists and system prompts help ensure nothing is overlooked.
For example, if only half of the services provided are entered, the organization will lose revenue. Implementing standardized workflows and frequent reconciliation of encounter forms with billing entries can mitigate these risks. Consistency at this stage strengthens the overall charge entry in medical billing process.
Step 5: Internal Review and Quality Assurance
Quality assurance (QA) is the checkpoint for charge entry in medical billing. Before claims are submitted, internal reviews or automated claim scrubbers identify errors, inconsistencies, or missing information. Dual verification or peer review processes further enhance accuracy.
Practices adopting QA protocols see a marked reduction in claim denials. For instance, a QA review may flag a mismatch between the documented diagnosis and the assigned code, preventing a denial. Addressing issues at this stage saves time and resources downstream.
According to competitor insights, organizations with robust QA procedures experience 15 percent fewer denials. Building a culture of accountability and regular feedback loops ensures continuous improvement in charge entry in medical billing and supports sustainable financial performance.
Step 6: Timely Submission of Charges
Speed is a crucial factor in charge entry in medical billing. Submitting charges promptly—ideally on the same day or next day—has a direct impact on accounts receivable and cash flow. Delayed entries can extend the payment cycle by weeks, leading to increased AR days and potential write-offs.
Healthcare organizations should establish internal benchmarks for turnaround time. Monitoring charge posting timeliness through daily or weekly reports helps identify bottlenecks. For example, if a clinic consistently posts charges a week after service dates, payments are delayed, negatively affecting revenue.
Best practices include real-time posting, automated reminders, and clear assignment of responsibilities. Timely charge entry in medical billing not only accelerates reimbursement but also reduces the risk of missing claim filing deadlines.
Step 7: Monitoring and Resolving Incomplete or Rejected Charges
The final step in charge entry in medical billing is ongoing monitoring and resolution of incomplete or rejected charges. Regularly running reports helps identify unbilled encounters, missing documentation, or rejected claims.
A structured process for correcting errors and resubmitting claims is vital. Root cause analysis should be conducted for recurring issues, enabling continuous process improvement. For example, if weekly reconciliation reports reveal frequent omissions in a specific department, targeted training or workflow adjustments can address the problem.
Continuous monitoring ensures that every service rendered is billed and reimbursed. By closing the loop, organizations maintain a high standard of accuracy and efficiency in charge entry in medical billing, safeguarding revenue and compliance.
Technology, Compliance, and Industry Trends in 2026
The landscape of charge entry in medical billing is rapidly evolving. For healthcare organizations, keeping pace with technology, regulatory shifts, and best practices is not just beneficial but essential. In 2026, the intersection of innovation and compliance is reshaping how charge entry in medical billing supports revenue cycle management and financial health.
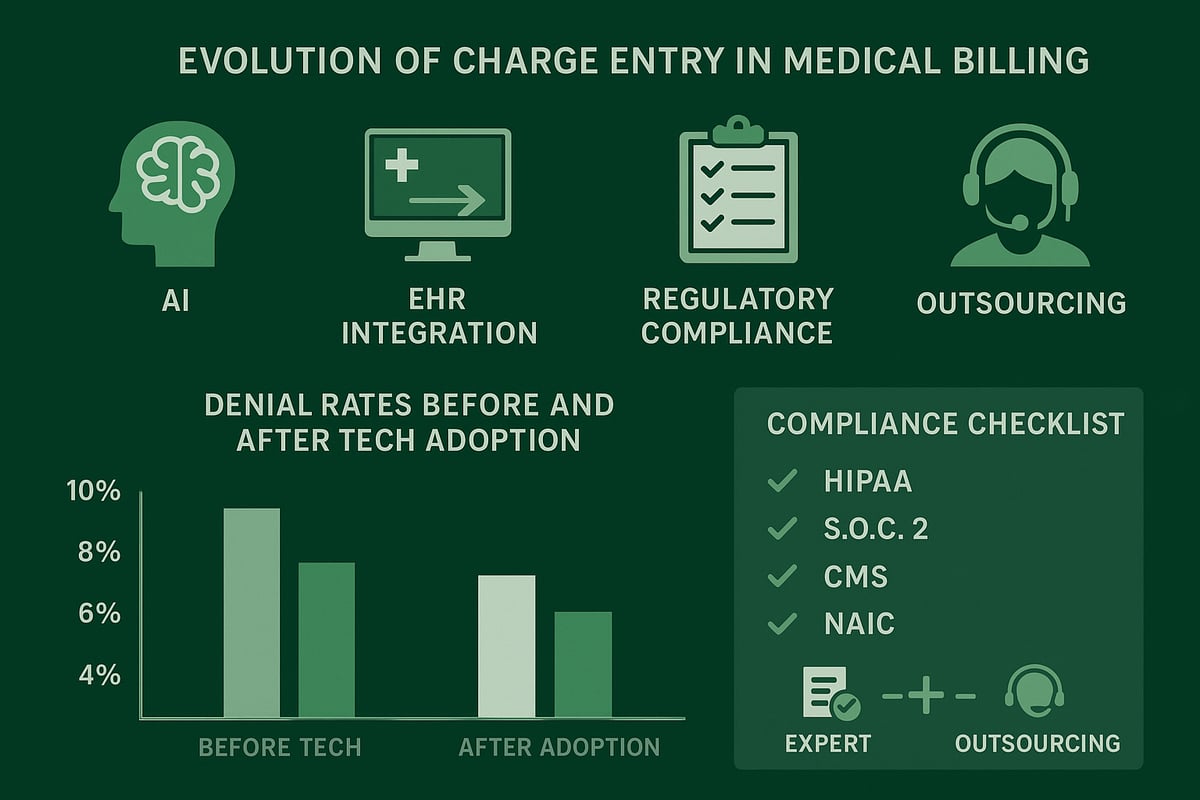
Evolving Technology in Charge Entry
Technology is transforming charge entry in medical billing for healthcare organizations. Automation, artificial intelligence, and advanced EHR integration streamline the process, reducing manual errors and improving efficiency. With AI-driven claim scrubbers and real-time validation tools, billing teams can identify discrepancies before claims are submitted.
Automated charge capture solutions are gaining traction, enabling seamless data transfer from clinical encounters to billing systems. This minimizes the risk of missed or duplicate charges. The adoption of cloud-based RCM platforms allows remote access, scalability, and secure data management.
One notable advancement is the integration of EHR systems, which has been shown to enhance charge entry accuracy and speed. By leveraging EHR Integration and Charge Entry Accuracy, healthcare organizations can significantly lower error rates and improve overall workflow.
These innovations make charge entry in medical billing not only more precise but also adaptable to the increasing complexity of payer requirements in 2026.
Regulatory and Compliance Considerations
Compliance is a cornerstone of charge entry in medical billing, especially as regulations become more complex in 2026. Healthcare organizations must adhere to HIPAA requirements for data privacy and security, ensuring patient information remains protected throughout the billing process.
Staying up to date with CPT, ICD-10, and payer-specific guidelines is critical. Regulatory changes can directly impact coding practices and charge entry accuracy. For example, new codes or documentation requirements may necessitate immediate updates to internal workflows and staff training.
According to Regulatory Trends in Medical Billing 2026, upcoming changes demand proactive adaptation from RCM teams. Non-compliance can lead to audits, penalties, and lost revenue, making continuous education and policy reviews essential.
Ultimately, integrating compliance into every aspect of charge entry in medical billing protects organizations from risk and supports sustainable financial performance.
Addressing Common Pitfalls and Denials
Despite technological advancements, common pitfalls still threaten charge entry in medical billing. The most frequent issues include coding errors, incomplete documentation, and late submissions. Each can trigger claim denials, delay payments, and increase administrative costs.
To minimize these risks, organizations should conduct regular audits, invest in ongoing staff training, and establish feedback loops between clinical and billing teams. Coding workshops and peer reviews are effective at reducing error rates and ensuring everyone is aligned with current standards.
Industry data shows that practices implementing robust denial management strategies consistently achieve lower denial rates. By focusing on root cause analysis and continuous improvement, healthcare organizations can optimize their charge entry in medical billing processes and protect their bottom line.
The Value of Outsourcing Charge Entry to Experts
As the complexities of charge entry in medical billing grow, many healthcare organizations are turning to specialized RCM partners for support. Outsourcing charge entry offers access to experienced professionals who stay current with regulatory updates and payer requirements.
Benefits include reduced error rates, scalability for growing practices, and the ability to handle complex, multi-specialty coding scenarios. Outsourced teams can seamlessly integrate with client-owned EHRs and billing platforms, ensuring accurate and timely charge posting.
For organizations seeking to maximize efficiency and minimize risk, partnering with experts in charge entry in medical billing provides a strategic advantage. It allows internal teams to focus on patient care while maintaining high standards in financial operations.
Best Practices and Tips for Error-Free Charge Entry
Optimizing charge entry in medical billing is essential for healthcare organizations seeking to maximize revenue and minimize compliance risk. By implementing structured processes and ongoing improvement strategies, practices can reduce denials, accelerate cash flow, and build a resilient revenue cycle.
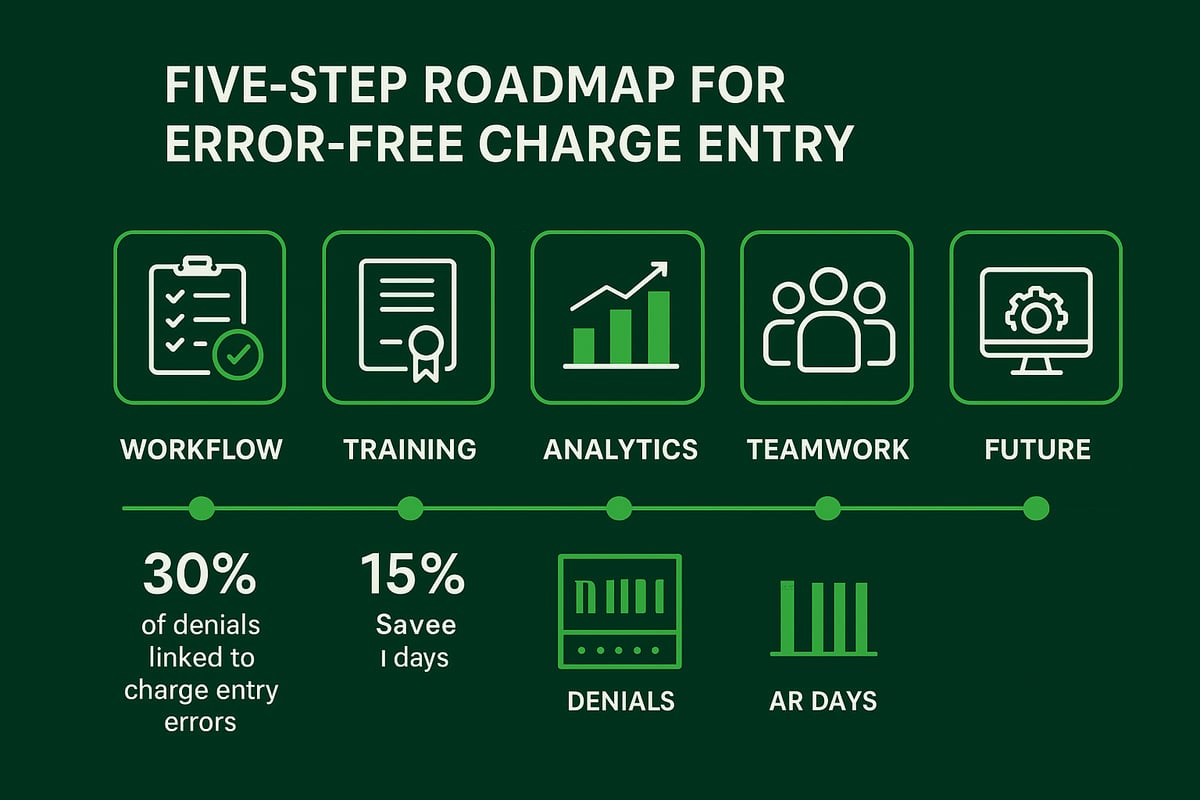
Building a Structured Charge Entry Workflow
A standardized workflow is the backbone of error-free charge entry in medical billing. Establishing clear standard operating procedures (SOPs) and detailed checklists ensures every step, from encounter documentation to claim submission, is followed consistently.
Key workflow elements include:
- Documenting each action with assigned responsibilities
- Using checklists to verify completeness before posting charges
- Mapping the process visually to identify potential bottlenecks
For example, a workflow diagram can clarify the handoff from providers to billing staff, reducing confusion. Regularly reviewing and updating these workflows helps organizations adapt to evolving payer requirements and regulatory changes. A structured approach not only minimizes errors but also streamlines staff onboarding and cross-training. By focusing on process optimization, organizations can make charge entry in medical billing more reliable and efficient.
Training and Continuing Education for Staff
Continuous education is vital for professionals handling charge entry in medical billing. Certification programs such as CPC, CCS, and CPB equip staff with foundational knowledge, while ongoing training ensures they stay updated on code and regulation changes.
Best practices include:
- Enrolling staff in annual coding workshops and webinars
- Facilitating peer mentoring for hands-on learning
- Encouraging cross-functional training between clinical and billing teams
Investing in education directly improves accuracy and reduces error rates. For a deeper understanding of coding’s impact, reference Medical Coding Types Explained, which highlights the importance of accurate coding in the charge entry workflow. When staff are well-trained, organizations report up to 30% fewer errors, leading to faster payments and fewer denials.
Leveraging Data Analytics and Reporting
Data analytics play a transformative role in optimizing charge entry in medical billing. By tracking key performance indicators (KPIs) such as charge lag days, error rates, and denial percentages, organizations can pinpoint areas needing improvement.
Effective analytics strategies:
- Implement monthly dashboards to visualize trends and anomalies
- Run regular denial analysis to identify root causes
- Monitor posting timeliness and reconciliation rates
For example, dashboards can quickly highlight spikes in denials related to specific codes or payers, enabling proactive responses. Utilizing insights from Understanding Denial Management in Billing supports targeted process enhancements and reduces revenue leakage. Data-driven decision-making helps organizations achieve measurable improvements across the entire charge entry in medical billing workflow.
Communication and Collaboration Across Teams
Strong communication bridges the gap between clinical, coding, and billing staff, creating a culture of accountability and shared success. Regular feedback sessions and interdepartmental huddles ensure that everyone involved in charge entry in medical billing is aligned.
Recommended practices include:
- Weekly team meetings to discuss documentation and coding challenges
- Open channels for feedback and clarification of payer rules
- Joint problem-solving for recurring issues
For instance, a brief weekly review can help resolve documentation discrepancies before they impact claims. Collaborative environments foster continuous learning and reduce the risk of incomplete or inaccurate charge entry in medical billing. Prioritizing communication streamlines workflows and enhances overall revenue cycle performance.
Preparing for Future Changes in Medical Billing
The landscape of charge entry in medical billing is constantly evolving with regulatory updates, payer policies, and technological advancements. Organizations must build resilience and adaptability into their processes to stay ahead.
Key preparation strategies:
- Engage in scenario planning for new code sets or payer requirements
- Monitor industry trends and regulatory updates regularly
- Pilot new EHR features or automation tools in a controlled environment
For example, early adoption of new compliance features allows teams to troubleshoot issues before they affect operations. By fostering a proactive mindset, healthcare organizations can ensure their charge entry in medical billing remains accurate and compliant, regardless of industry shifts.
Now that you understand how critical accurate charge entry is for your practice’s financial health and compliance—especially with the new complexities in 2026—you might be wondering how to put these steps into action without overwhelming your team. That’s where expert support makes all the difference. At Greenhive Billing Solutions, we specialize in tailored charge entry processes that minimize errors, optimize reimbursements, and keep you ahead of industry changes. If you’re ready to take the next step toward a more efficient, profitable workflow, let’s talk about your unique needs. Book Your Free Consultation