The landscape of health care and medical services in the U.S. is evolving at an unprecedented pace, presenting both significant challenges and new opportunities for providers in 2026.
Increasingly complex regulations, rapid technology integration, and rising patient expectations are reshaping the way organizations operate and deliver care. Professionals, clinics, and healthcare organizations must stay agile to succeed.
This article serves as your essential roadmap, offering actionable guidance for navigating regulatory changes, leveraging technology trends, optimizing care delivery models, and strengthening your revenue cycle. Prepare to future-proof your practice with strategic planning tailored for the year ahead.
Navigating Regulatory Changes in 2026
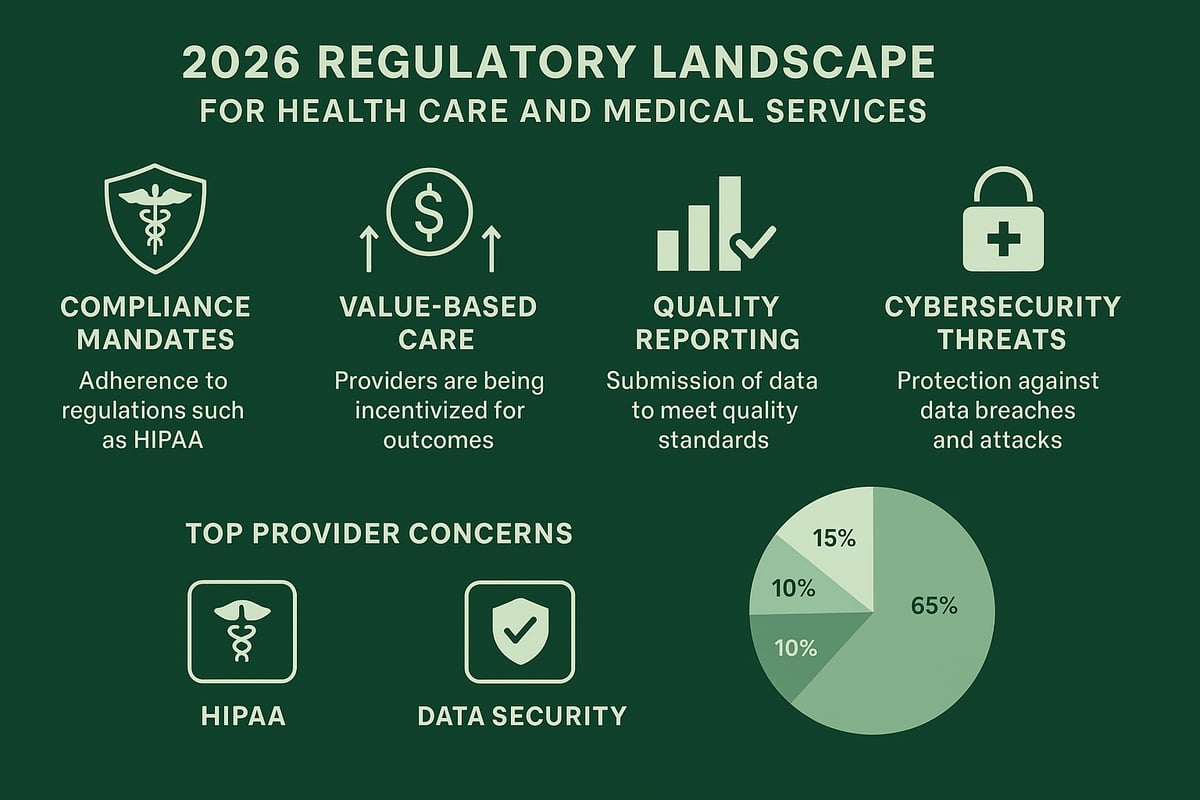
Navigating the evolving regulatory landscape is a top priority for leaders in health care and medical services. As 2026 approaches, providers face new compliance mandates, payment models, and reporting standards. Staying ahead of these changes is essential for operational stability and sustained growth.
Understanding New Compliance Mandates
In 2026, federal and state agencies are rolling out significant updates impacting health care and medical services. New HIPAA rules focus on interoperability, requiring providers to ensure uninterrupted data exchange and patient privacy.
Day-to-day operations must adapt to tighter controls and clearer documentation. Common pitfalls include incomplete consent forms and outdated privacy policies. To avoid penalties, implement regular compliance audits and staff training.
According to the MGMA 2024 survey, 65% of providers list compliance as their top challenge. Prioritizing compliance helps organizations maintain trust and avoid costly disruptions.
Value-Based Care and Payment Reform
The shift from fee-for-service to value-based models is accelerating across health care and medical services. In 2026, advanced payment reforms tie reimbursement to patient outcomes and cost-efficiency.
Providers must navigate new reporting requirements and track quality metrics more closely. For example, a multi-specialty clinic recently restructured workflows to meet value-based contract terms, resulting in improved care coordination and financial performance.
Adapting to these models requires robust data collection and a proactive approach to payer negotiations. This ensures sustainable revenue and better patient experiences.
Quality Reporting and Accreditation
Quality reporting standards such as MIPS, MACRA, and private payer programs have evolved in 2026. Health care and medical services must now streamline data submission and prepare for more rigorous accreditation reviews.
Leveraging third-party services can simplify accreditation preparation and ensure all documentation meets regulatory expectations. Credentialing is also critical—organizations turn to medical credentialing services for efficient provider onboarding and compliance management.
Effective reporting not only secures reimbursement but also strengthens your reputation with payers and patients.
Data Privacy, Security, and Cyber Threats
Cybersecurity threats have surged, targeting health care and medical services with phishing, ransomware, and insider risks. Recent data breaches highlight the importance of robust security protocols.
Best practices include multi-factor authentication, regular vulnerability assessments, and ongoing staff education. Protecting patient data requires both advanced technology and a culture of security awareness.
Investing in cyber defense reduces the risk of data loss and regulatory fines, keeping your organization resilient in a digital-first environment.
Preparing for Audits and Inspections
Audits are more frequent in 2026, with payers, CMS, and internal teams scrutinizing health care and medical services for compliance. Proactive documentation and clear audit trails are your best defense.
Anticipate the types of audits you may face by maintaining thorough records and conducting mock inspections. A mid-sized practice recently passed a payer audit by implementing monthly documentation reviews and staff refresher sessions.
Audit readiness ensures uninterrupted operations and reinforces your commitment to regulatory excellence.
Integrating Technology for Efficient Medical Services
The future of health care and medical services is defined by rapid technology adoption and seamless integration. In 2026, providers face a landscape where efficiency, security, and patient engagement are driven by advanced digital tools. Staying ahead means embracing innovation while ensuring compliance and optimizing workflows.

EHR Optimization and Interoperability
By 2026, federal and state standards require health care and medical services providers to achieve higher levels of EHR integration. Seamless data sharing is no longer optional—it is essential for coordinated care and regulatory compliance.
Interoperability allows clinicians to access comprehensive patient records across systems, reducing errors and duplicative testing. For example, a specialty clinic using integrated EHRs saw faster referrals and improved patient outcomes. Investing in EHR optimization is a foundational step for efficient operations.
Telehealth and Remote Patient Monitoring
Telehealth has become a core component of health care and medical services, especially after the pandemic accelerated adoption. Utilization rates remain high, with reimbursement models evolving to support virtual visits and remote monitoring.
Clinics implementing telehealth benefit from increased access, particularly in rural areas. Practical steps include selecting HIPAA-compliant platforms, training staff, and integrating remote patient monitoring devices. A rural clinic, for instance, expanded its reach and reduced missed appointments through virtual care options.
Artificial Intelligence and Automation in Practice Management
Artificial intelligence is transforming health care and medical services by automating routine administrative tasks and enhancing decision-making. AI-powered tools streamline scheduling, documentation, and clinical support, which reduces errors and boosts productivity.
According to recent data, 42% of practices report higher efficiency with AI adoption. To explore more about these industry shifts and future trends, see Healthcare Industry Trends to Watch in 2026. Embracing AI positions organizations for sustained growth and competitive advantage.
Cybersecurity and IT Infrastructure
With the surge in cyber threats targeting health care and medical services, robust cybersecurity is non-negotiable. Ransomware, phishing, and insider risks are top concerns for providers in 2026.
Building a resilient IT infrastructure involves multi-layered security measures—firewalls, encryption, and regular vulnerability assessments. A specialty group implementing these strategies maintained uninterrupted operations even during attempted breaches. Ongoing staff training is vital to minimize human error and reinforce security protocols.
Patient Engagement Platforms and Digital Front Doors
Patient engagement solutions are redefining how health care and medical services connect with individuals. Mobile apps, patient portals, and online scheduling increase convenience and satisfaction.
Studies show 78% of patients prefer digital communication with providers. By offering intuitive self-service options, organizations improve retention and streamline administrative processes. Digital front doors empower patients while freeing staff to focus on high-value care activities.
Staff Training and Change Management
Adopting new technologies in health care and medical services requires effective change management. Resistance is common, but continuous training and clear communication can drive successful transformation.
Ongoing education programs, peer support, and leadership buy-in help teams adapt to evolving digital tools. A multi-location clinic saw smooth technology adoption by prioritizing staff engagement and feedback. Investing in people ensures technology delivers its full potential.
Optimizing Revenue Cycle Management for Financial Health
Revenue cycle management remains a cornerstone for financial sustainability in health care and medical services. As regulatory demands and payer requirements intensify in 2026, clinics and organizations must adapt their processes to secure optimal cash flow and minimize revenue leakage. A proactive approach to RCM helps ensure that patient care translates into timely and accurate reimbursement.
End-to-End Billing and Claims Processing
Efficient billing and claims processing underpin financial health for health care and medical services. In 2026, practices must keep pace with evolving payer policies and compliance standards. Common challenges include coding errors, incomplete documentation, and delayed submissions, all of which can result in lost revenue.
Key steps for success:
- Ensure precise coding aligned with new regulations
- Maintain thorough documentation for all encounters
- Implement regular audits of claim submissions
A multi-location provider recently reduced claim denials by 18% by proactively identifying documentation gaps and cross-training billing staff. This approach highlights how targeted improvements in billing workflows directly impact the bottom line for health care and medical services.
Insurance Eligibility Verification and Prior Authorization
Verifying insurance eligibility and obtaining prior authorizations are essential steps that directly affect the revenue cycle in health care and medical services. Manual processes often lead to delays, denials, and dissatisfied patients.
To streamline these tasks:
- Use automated eligibility verification tools integrated with payer portals
- Establish clear protocols for collecting and confirming patient information
- Track authorization status in real time to prevent service delays
Practices that automate eligibility checks report up to 30% fewer claim denials, which significantly improves both cash flow and patient experience. By investing in efficient verification processes, health care and medical services organizations can ensure smoother operations and fewer financial surprises.
Denial Management and Appeals Strategies
Denials remain a persistent challenge for health care and medical services, with common causes including authorization errors, coding mismatches, and missing information. A structured denial management process is crucial for revenue recovery and compliance.
Key strategies include:
- Identify denial trends through data analysis
- Develop standardized appeal templates for frequent issues
- Train staff on payer-specific documentation requirements
For a deeper dive into effective approaches, consider this guide on denial management strategies in healthcare, which outlines actionable steps to reduce lost revenue. By prioritizing denial management, organizations can turn potential write-offs into recovered income for health care and medical services.
Revenue Analytics and Performance Reporting
Data-driven decision-making is transforming how health care and medical services optimize revenue. Real-time dashboards and advanced analytics reveal trends, highlight bottlenecks, and support informed planning.
Effective use of analytics includes:
- Monitoring key performance indicators (KPIs) like days in A/R and collection rates
- Segmenting data by payer, service line, or location for targeted improvements
- Benchmarking against industry standards to identify opportunities
One clinic leveraged analytics to boost collections by 15%, simply by identifying underperforming payers and reallocating staff resources. For health care and medical services, continuous performance monitoring is essential for financial growth and sustainability.
Greenhive Billing Solutions: Enhancing Revenue Cycle Performance
Greenhive Billing Solutions offers a comprehensive suite of revenue cycle management services tailored to health care and medical services providers. Our experienced professionals work seamlessly within your existing systems, reducing administrative burden and improving reimbursement outcomes.
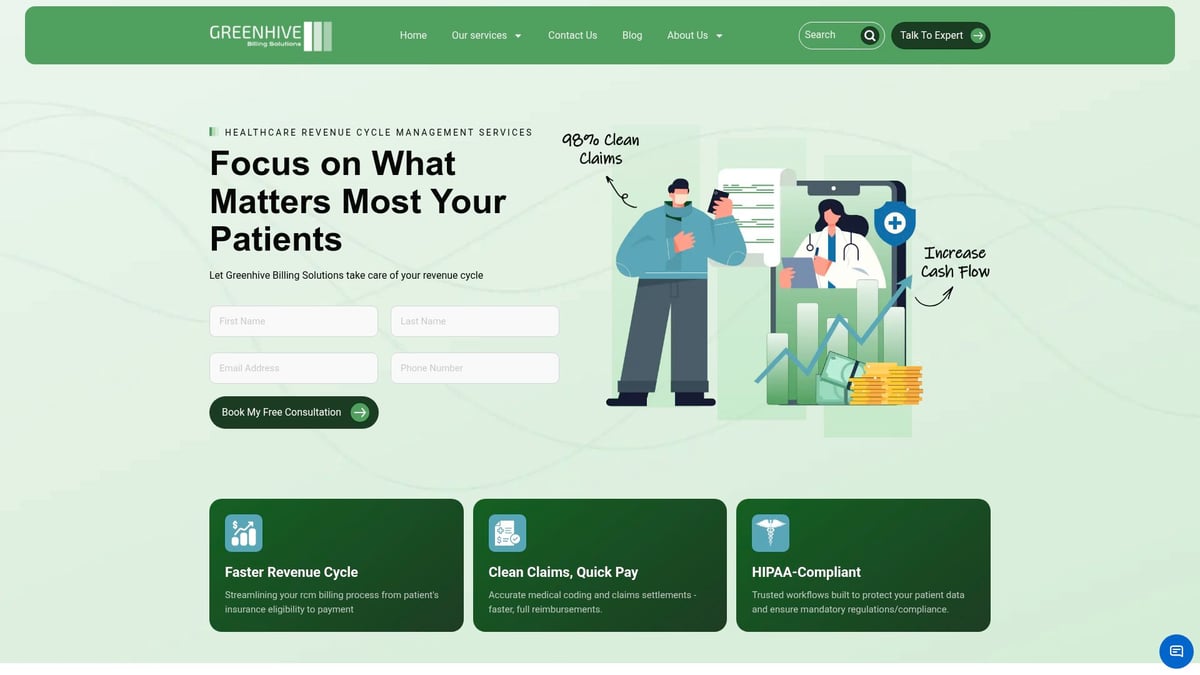
Key benefits include:
- HIPAA-compliant processes and transparent reporting
- Specialty-focused support for diverse medical practices
- Dedicated U.S.-based team of certified billing experts
On average, practices that partner with Greenhive report up to $47,000 in annual cost reductions compared to in-house billing. Our commitment is to help your organization focus on patient care while we handle the financial complexities of health care and medical services.
Evolving Models of Care Delivery
As 2026 approaches, health care and medical services are shifting dramatically in response to new patient needs, technology, and policy. Providers must be ready to adapt their care delivery models to remain competitive and deliver measurable results. The following subsections highlight the most impactful trends and strategies shaping the future of care delivery.
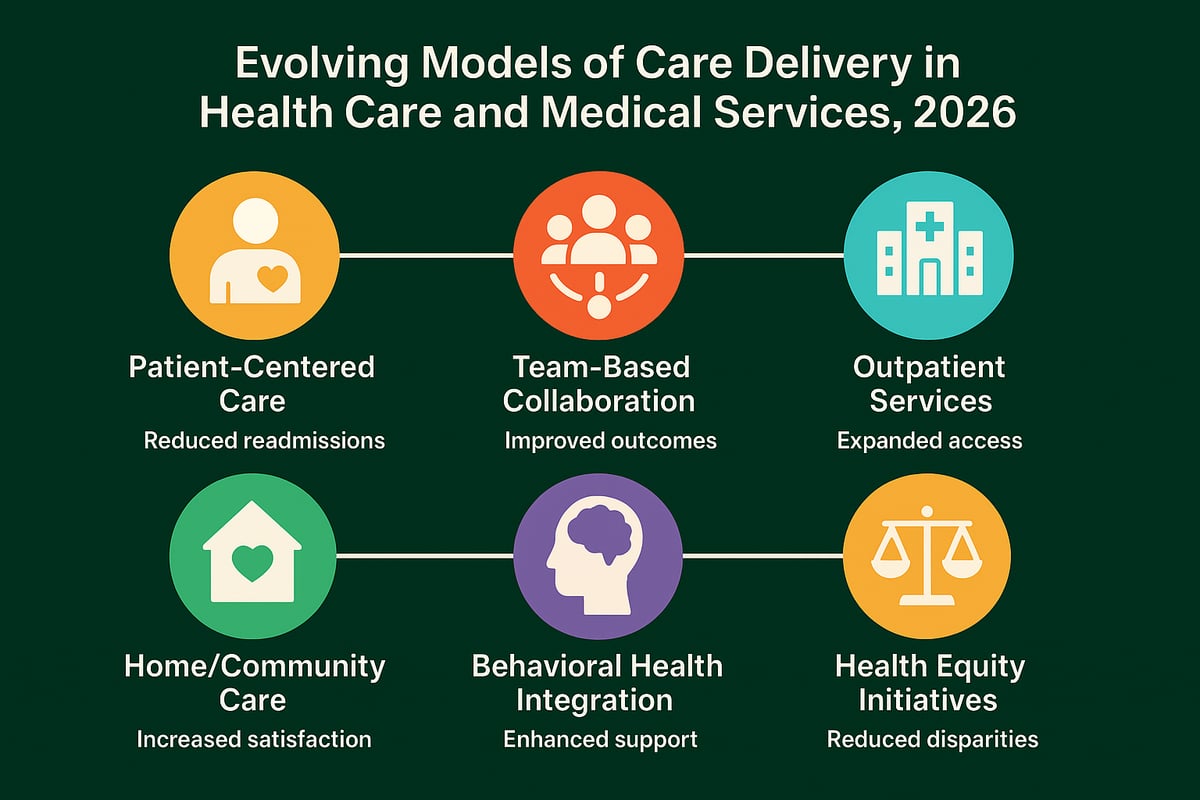
Patient-Centered Care and Population Health
In 2026, health care and medical services are increasingly focused on holistic, patient-centered care. This means looking beyond clinical symptoms to address social determinants like housing, nutrition, and access to resources. Tracking population health outcomes has become a core metric for organizations, driving quality improvement and accountability.
For example, clinics that implement targeted population health programs have seen meaningful reductions in readmission rates. The Centers for Medicare & Medicaid Services is actively seeking input on inpatient hospital whole-person care, underscoring the industry's commitment to comprehensive approaches (CMS Seeks Input on Inpatient Hospital Whole-Person Care). For providers, this shift supports stronger patient relationships and long-term financial performance.
Team-Based and Collaborative Care Approaches
Team-based models are transforming how health care and medical services are delivered. By fostering interdisciplinary collaboration among physicians, nurses, pharmacists, social workers, and administrative staff, organizations can better manage chronic conditions and complex cases.
Clinics adopting these models report 20 percent better patient outcomes, according to AHRQ 2025. Coordinated care meetings, shared care plans, and streamlined communication processes ensure every professional is aligned with patient goals. This approach not only improves satisfaction for patients but also enhances morale and retention among care teams.
Expansion of Outpatient and Ambulatory Services
The expansion of outpatient and ambulatory services is a defining trend in health care and medical services for 2026. Providers are opening more urgent care centers, specialty clinics, and ambulatory surgery centers to meet rising demand and control costs.
These settings offer financial advantages, reduced overhead, and greater flexibility for both patients and staff. For instance, one ambulatory surgery center reported a significant increase in patient volumes after shifting select procedures out of the hospital environment. This trend enables practices to capture new revenue streams while delivering efficient, high-quality care.
Home-Based and Community Care Innovations
Home-based care is rapidly gaining traction in health care and medical services. Advances in remote monitoring, mobile clinics, and community partnerships are making it possible to reach patients where they live.
Practices that embrace these models see notable benefits. For example, a home-based care initiative reduced emergency room visits by 30 percent, improving both patient experience and operational efficiency. Technology enables providers to track vital signs, medication adherence, and social needs, ensuring continuity of care beyond the clinic walls.
Integrating Behavioral and Mental Health Services
Integrating behavioral and mental health into primary care is now a priority for health care and medical services organizations. Regulatory incentives and updated reimbursement models are driving adoption of collaborative care approaches, where mental health professionals work closely with primary care teams.
Technology-enabled support, like virtual counseling and digital screening tools, helps streamline integration. According to SAMHSA 2025, practices that incorporate behavioral health see an 18 percent improvement in patient adherence and engagement. This comprehensive model addresses the full spectrum of patient needs and supports better health outcomes.
Addressing Health Equity and Access Disparities
Closing gaps in access is essential for the future of health care and medical services. Providers are leveraging data analytics to identify underserved populations and design targeted outreach programs. Community partnerships and culturally competent care delivery are also key strategies.
One urban clinic, for example, improved access for minority patients by offering multilingual support and flexible scheduling. These initiatives not only promote health equity but also expand patient panels and strengthen organizational reputation in the communities served.
Strategic Planning and Future-Proofing Your Practice
Strategic planning is essential for every organization offering health care and medical services in 2026. The industry faces constant change, requiring proactive measures to navigate workforce challenges, financial pressures, technological advancements, and evolving patient needs. Future-proofing your business means adopting flexible strategies, building resilience, and using data-driven insights to stay ahead.
Workforce Planning and Talent Management
The demand for skilled professionals in health care and medical services continues to outpace supply. In 2026, organizations must address provider shortages and staff burnout by implementing robust recruitment tactics. Flexible work arrangements, career development programs, and employee well-being initiatives are essential for retention.
Consider creating talent pipelines through partnerships with universities and professional organizations. Staffing analytics can help forecast needs and adjust scheduling. Since 54% of practices cite staffing as their top concern, a proactive approach ensures operational stability and quality patient care.
Financial Forecasting and Budget Optimization
Reliable financial forecasting is critical for health care and medical services to withstand reimbursement shifts and rising costs. Scenario planning tools enable organizations to model different payment environments, especially with regulatory changes like the CMS Proposes Physician Payment Rule for 2026 impacting future revenue.
Budget optimization requires continuous review of expenses and identification of cost-saving opportunities. Multi-site groups often benefit from centralized procurement and shared services. Routine financial analysis allows practices to align investments with growth goals, securing long-term sustainability.
Embracing Innovation and Continuous Improvement
Innovation drives success in health care and medical services. Foster a culture where staff are encouraged to suggest improvements and pilot new processes. Launching pilot programs for new service lines or workflow enhancements can reveal scalable solutions.
Regular feedback loops and performance reviews support continuous improvement. Track pilot results, measure outcomes, and scale what works. Staying adaptable allows your organization to respond swiftly to market trends and patient expectations, maintaining a competitive edge.
Building Strategic Partnerships and Referral Networks
Collaborating with other health care and medical services providers, hospitals, and community organizations strengthens care continuity and expands business opportunities. Strategic partnerships can increase access to specialty services, improve patient outcomes, and generate new revenue streams.
Establish formal referral networks to streamline care transitions and reduce delays. For example, practices that actively manage referrals see higher patient satisfaction and better utilization of specialty services. Building strong relationships with partners ensures mutual growth and resilience.
Risk Management and Business Continuity Planning
Identifying and mitigating risks is vital for health care and medical services leaders. Common risks include cyber threats, natural disasters, and operational disruptions. Developing a comprehensive business continuity plan ensures uninterrupted patient care during unexpected events.
Key elements of an effective plan:
- Regular risk assessments
- Data backup and recovery protocols
- Cross-training staff for critical functions
A well-prepared organization can maintain operations and protect its reputation, even in challenging circumstances.
Measuring Success: KPIs and Benchmarking
Defining and tracking key performance indicators (KPIs) is fundamental for health care and medical services to achieve financial and operational excellence. Benchmarking against industry standards helps identify strengths and areas for improvement. Practices using KPIs report 22% higher financial performance, according to the Medical Group Management Association in 2025.
Utilize real-time dashboards and analytics, such as those detailed in Healthcare revenue cycle analytics insights, to monitor revenue, patient outcomes, and staff productivity. Regularly review benchmarks with leadership to inform strategic decisions and drive continuous growth.
As you prepare for the future of healthcare, navigating new regulations, adopting innovative technology, and optimizing your revenue cycle can feel overwhelming. We know how important it is to stay ahead—whether you're focused on compliance, boosting efficiency, or maximizing reimbursements. If you want to discuss tailored strategies for your practice and see how expert support can make a difference, let’s connect. You deserve a partner who understands the unique challenges of 2026 and can help you thrive with confidence.
Book Your Free Consultation
We’re here to help you achieve your goals, every step of the way.