Navigating the complexities of medical insurance pay is more critical than ever for healthcare organizations striving for financial stability. As payer rules and regulations continue to evolve, gaining a clear understanding of how medical insurance pay works can directly shape your practice’s revenue and patient satisfaction.
This comprehensive guide empowers healthcare providers, practice managers, and billing teams with actionable steps, expert strategies, and essential insights. By mastering the processes and compliance requirements, your organization can maximize reimbursements and avoid costly errors.
Read on to discover a step-by-step overview of medical insurance pay, including key concepts, claim workflows, payer rules, denial management, compliance essentials, reimbursement optimization, and future industry trends. Take the next step toward a stronger, more resilient revenue cycle.
Understanding Medical Insurance Pay: Key Concepts and Terminology
Navigating the landscape of medical insurance pay can feel overwhelming, yet it is essential for healthcare organizations aiming to maintain predictable revenue. Understanding the key concepts and terminology behind medical insurance pay lays the groundwork for efficient billing, accurate claim submissions, and improved patient communication.
![]()
What is Medical Insurance Pay?
Medical insurance pay refers to the process and financial transactions through which healthcare organizations receive payment from insurance carriers for services rendered to insured patients. Unlike patient self-pay, where individuals cover costs directly, or government payers such as Medicare and Medicaid, medical insurance pay primarily involves commercial insurers, managed care organizations, and sometimes specialized coverages like Med Pay.
Providers often interact with a variety of payer types, including commercial insurance, Medicaid, Medicare, and managed care plans. For example, a routine care visit may be covered by a commercial PPO, while auto accident injuries might fall under Med Pay, which covers medical expenses regardless of fault, as outlined by Allstate and State Farm. However, some mistakenly believe Med Pay covers lost wages or property damage, which it does not. Knowing these distinctions is crucial for accurate billing and maximizing medical insurance pay.
Essential Terms and Acronyms
A strong grasp of industry terminology is fundamental for smooth medical insurance pay processes. Common acronyms include EOB (Explanation of Benefits), ERA (Electronic Remittance Advice), CPT (Current Procedural Terminology), ICD-10 (diagnosis coding), and NPI (National Provider Identifier). Financial terms such as deductible, co-pay, and coinsurance directly affect how much insurance will pay and what remains the patient’s responsibility.
Consider the differences between medical payments coverage and liability coverage: Med Pay is designed to cover medical expenses regardless of fault, while liability coverage addresses injuries to others. Reviewing EOB and ERA documents is essential for identifying payment amounts and reconciling accounts. Understanding policy limits and exclusions helps avoid common errors. For a deeper dive into eligibility verification and how it impacts medical insurance pay, see Verify Medical Insurance Eligibility.
Types of Medical Insurance Coverage and Their Impact on Pay
Medical insurance pay outcomes are shaped by the type of coverage held by the patient. Common coverage types include PPO, HMO, EPO, indemnity plans, Med Pay, and PIP (Personal Injury Protection). The type of plan determines payment responsibility, claim submission workflow, and which expenses are covered.
For instance, Med Pay may act as the primary payer for accident-related injuries, while in other cases it is secondary to health insurance. State regulations also play a significant role, as Med Pay is not available in all states and coordination of benefits rules vary. When patients have multiple policies, understanding who pays first is vital for efficient medical insurance pay and timely reimbursement.
Recent Regulatory and Industry Changes
The rules governing medical insurance pay are constantly evolving. Recent regulations have affected how payers process claims, set reimbursement rates, and define coverage requirements. For example, Med Pay availability varies by state, and some states require no-fault insurance, impacting payment procedures.
Payer policy updates frequently introduce new documentation standards and reimbursement models. The shift from fee-for-service to value-based models is reshaping payment flows and compliance obligations. Staying informed about these changes ensures healthcare organizations remain compliant and optimize medical insurance pay processes for both current and future requirements.
The Medical Insurance Pay Workflow: From Patient Encounter to Reimbursement
Navigating the medical insurance pay workflow is crucial for healthcare organizations aiming to achieve consistent cash flow and minimize revenue leakage. Each step, from verifying coverage to collecting patient balances, plays a specific role in ensuring accurate and timely reimbursement. Understanding and refining these processes can directly impact your bottom line and operational efficiency.
Step 1: Insurance Eligibility Verification
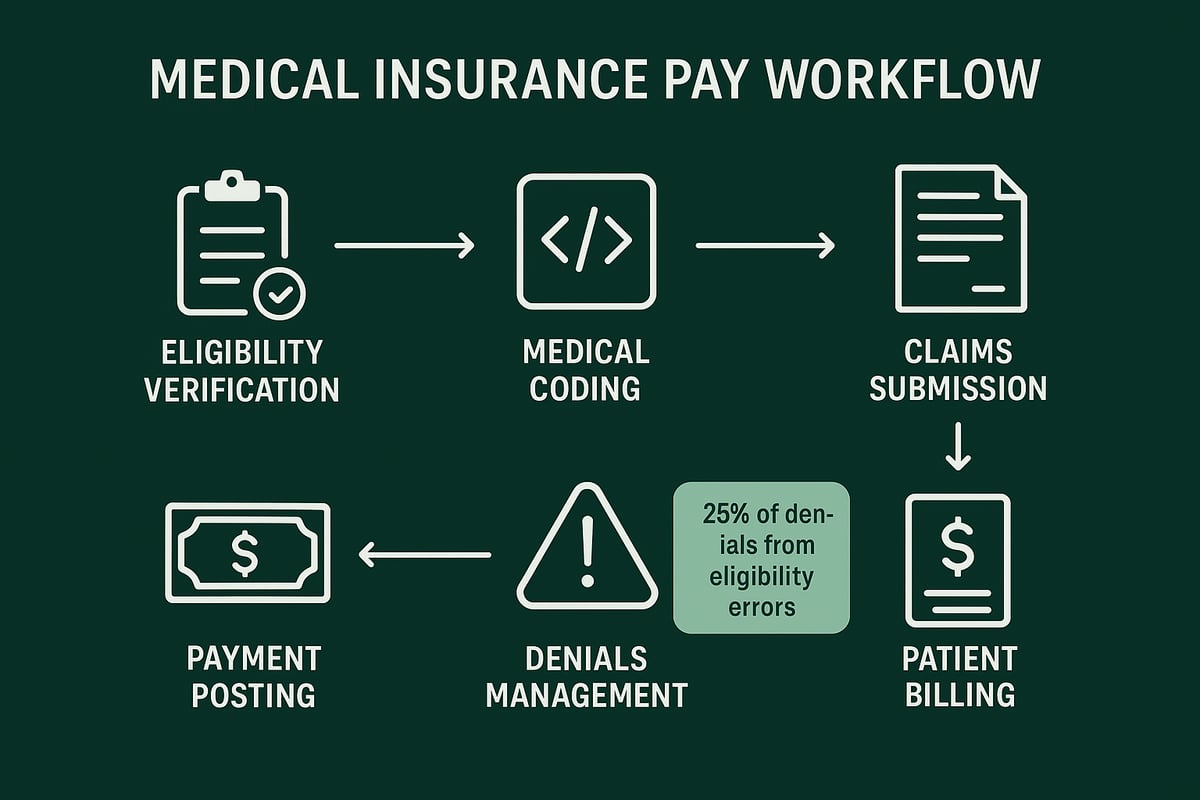
Verifying insurance eligibility is the first critical step in the medical insurance pay workflow. Before providing care, your front-office or billing team must confirm the patient's insurance details, such as active coverage, plan type, and specific benefits.
Modern methods include real-time eligibility tools, payer portals, and clearinghouses. Missing or incorrect eligibility data often leads to claim denials or delays. Industry data shows that up to 25% of medical insurance pay denials stem from eligibility errors, which can be avoided through proactive checks.
Best practices for B2B providers include:
- Verifying coverage at every visit
- Documenting verification results in the EHR
- Training staff to recognize plan changes and lapses
Regular eligibility verification not only accelerates payment but also reduces administrative rework, supporting a smoother medical insurance pay cycle.
Step 2: Accurate Medical Coding and Documentation
Accurate coding and documentation are the backbone of successful medical insurance pay processes. Each patient encounter must be coded using the correct CPT, ICD-10, and HCPCS codes to reflect the services provided.
Mistakes in coding, such as using outdated codes or omitting injury details for accident-related visits, can result in claim denials or underpayments. Documentation must support the codes billed and meet payer requirements for specificity and completeness.
Key actions for B2B organizations:
- Employ certified coders or regularly audit coding practices
- Maintain up-to-date code sets and payer guidelines
- Ensure providers document the medical necessity and details of care
Consistent, accurate coding is essential for maximizing medical insurance pay and maintaining compliance.
Step 3: Claims Submission and Processing
Submitting claims efficiently is vital for prompt medical insurance pay. Most payers prefer electronic claims, which speed up processing and reduce errors. Clearinghouses play a key role by performing initial edits and error checks before claims reach payers.
Payer-specific requirements, such as attachments or pre-authorizations, must be met to avoid rejections. For example, auto insurers like State Farm and Allstate often require detailed accident information for Med Pay claims.
To ensure your claims are processed quickly and accurately, review best practices for Clean Claim in Medical Billing. Clean claims typically process within 7 to 21 days, supporting faster medical insurance pay cycles.
Step 4: Payment Posting and Reconciliation
After claims are processed, payments are issued and must be posted accurately to patient accounts. This step in the medical insurance pay workflow involves interpreting Explanation of Benefits (EOBs) and Electronic Remittance Advices (ERAs).
Common tasks include:
- Identifying and resolving underpayments or overpayments
- Applying contractual adjustments
- Reconciling payments with bank deposits and patient ledgers
For Med Pay, certain expenses may be covered with no deductible or co-pay, so precise reconciliation is critical. Using detailed reports and reconciliation tools helps B2B providers track payment trends and quickly identify discrepancies in their medical insurance pay cycle.
Step 5: Denials Management and Appeals
Denials are an unavoidable part of the medical insurance pay process, but effective management can recover significant revenue. Common denial reasons include coverage limits, missing documentation, and coding errors.
A structured denials management process includes:
- Investigating the root cause
- Correcting errors and resubmitting claims
- Filing timely appeals with supporting documentation
For Med Pay, denials may occur if policy limits are exceeded or accident details are incomplete. Industry benchmarks indicate average denial rates of 5-10%, with appeal success rates varying by payer. By reducing denials, your organization can optimize medical insurance pay and improve cash flow.
Step 6: Patient Billing and Balance Collection
Once insurance payments are posted, communicating the patient's responsibility is the final step in the medical insurance pay workflow. Clear, timely patient statements and follow-up are essential for collecting outstanding balances.
Best practices include:
- Sending statements promptly after insurance adjudication
- Offering multiple payment options
- Coordinating benefits when patients have secondary insurance
Med Pay can sometimes cover co-pays or out-of-pocket expenses not paid by health insurance, reducing patient bad debt. Educating patients about their coverage and responsibilities ensures a positive experience and supports steady medical insurance pay for your organization.
Payer Rules, Coverage Limits, and Compliance Essentials
Understanding payer rules, coverage limits, and compliance is critical for any organization navigating medical insurance pay. Each step, from documentation to risk management, shapes your ability to secure timely, accurate reimbursements.
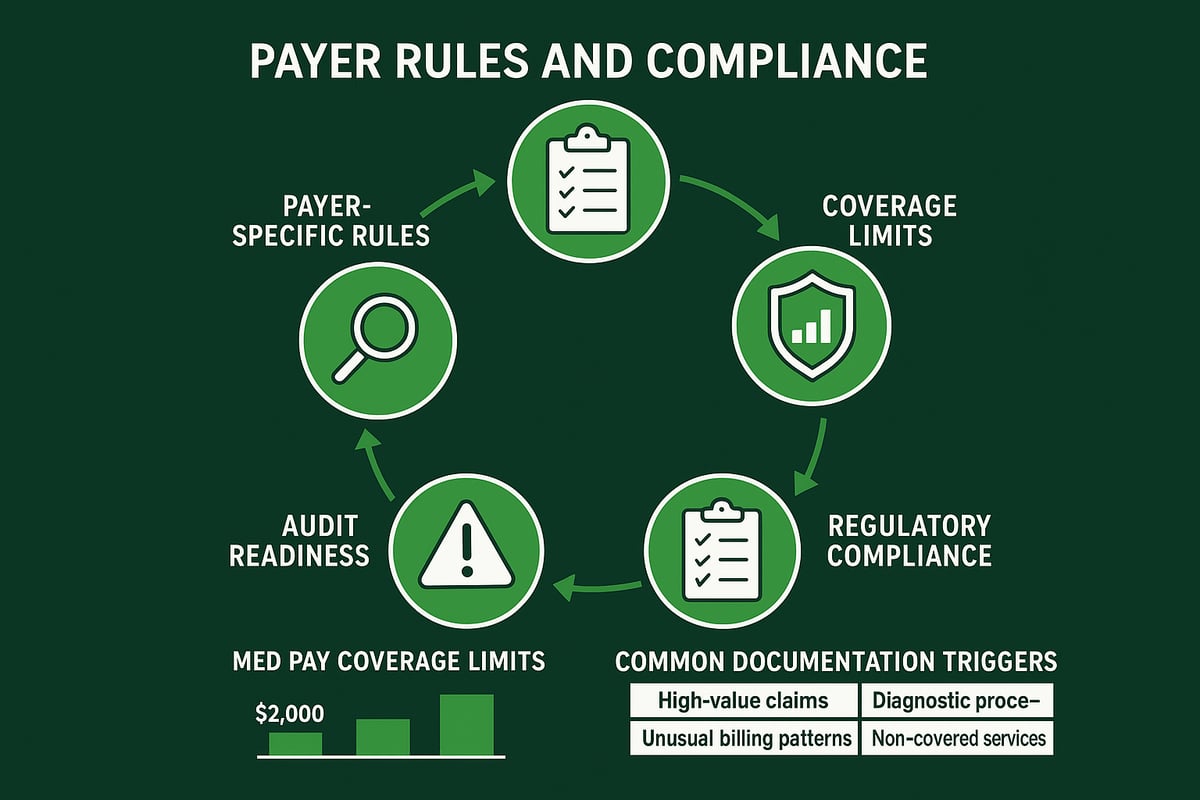
Navigating Payer-Specific Rules and Documentation
Every payer brings its own set of rules to the medical insurance pay process. Commercial, government, and auto insurers each require specific documentation, such as accident reports, provider notes, and pre-authorizations.
For Med Pay, detailed accident information is often mandatory, including date, location, and involved parties. Staying updated with payer bulletins helps avoid delays or denials. Missing even a single required document can stall the entire payment timeline.
Healthcare organizations should create checklists and workflows tailored to each payer type. This ensures claims are submitted right the first time, minimizing rework and lost revenue related to medical insurance pay.
Understanding Coverage Limits, Exclusions, and Coordination
Coverage limits and policy exclusions are central to medical insurance pay. For example, Med Pay typically covers $5,000 to $25,000 in medical expenses, but does not include lost wages or property damage. Some policies also exclude coverage for injuries to occupants of other vehicles.
Coordinating benefits is another critical aspect. When multiple policies are involved, it is essential to determine which payer is primary and which is secondary. Reviewing patient coverage at every encounter helps prevent surprises.
By clarifying these details upfront, providers can reduce payment disputes and streamline the medical insurance pay workflow.
Compliance with Federal and State Regulations
The compliance landscape for medical insurance pay is constantly evolving. Key laws like HIPAA and the ACA govern privacy, billing processes, and insurance mandates. State regulations often add requirements, especially regarding Med Pay and accident-related claims.
Healthcare organizations must implement robust data security measures and document all billing activities. Penalties for non-compliance can include audits, fines, or even exclusion from payer networks.
Staying current with regulatory updates is crucial. For example, the 2025 Marketplace Integrity and Affordability Final Rule outlines important changes impacting payer compliance and medical insurance pay requirements.
Audit Readiness and Documentation Best Practices
Audit readiness is a proactive strategy for any organization managing medical insurance pay. Audits may be triggered by high volumes of Med Pay claims or unusual billing patterns. To prepare, maintain thorough, accurate records for every claim.
Documentation checklists should include all payer-required data points, from patient eligibility to supporting clinical notes. Conducting regular internal reviews and staff training ensures ongoing compliance.
The impact of an audit can be significant. Not only can it affect reimbursement, but it may also influence your organization’s standing with payers and regulators.
Risk Management and Fraud Prevention
Risk management is essential in the medical insurance pay cycle. Common fraud schemes include billing for non-covered services or inflating claim amounts. Payers deploy anti-fraud initiatives, and providers must implement strong internal controls.
Regular monitoring and clear protocols help detect errors or suspicious activity early. Legal consequences of fraud are severe, ranging from financial penalties to contract termination.
By prioritizing compliance and transparency, healthcare organizations protect their revenue and reputation while navigating medical insurance pay complexities.
Strategies for Optimizing Medical Insurance Pay and Reducing Denials
Healthcare organizations need robust strategies to maximize medical insurance pay and minimize denials. By refining processes at every stage of the revenue cycle, B2B providers can boost financial performance, lower administrative costs, and deliver a better experience for both clients and patients.
Proactive Denial Prevention and Revenue Cycle Best Practices
The foundation of optimizing medical insurance pay lies in preventing denials before they occur. Common root causes include eligibility errors, incomplete documentation, and incorrect coding. Implementing real-time eligibility checks and pre-billing audits can drastically reduce errors.
It is essential to keep staff trained on payer requirements and utilize denial management dashboards to monitor key performance indicators. Industry benchmarks suggest average denial rates range from 5 to 10 percent. For a detailed guide on reducing and managing denials, see Denial Management in Medical Billing.
By investing in front-end verification and fostering a culture of continuous improvement, practices can ensure more claims are paid promptly. This proactive approach directly impacts overall medical insurance pay outcomes.
Advanced Claims Management and Follow-Up
Efficient claims management is crucial for optimizing medical insurance pay. Automated tracking systems help prioritize high-value and aged claims, ensuring timely follow-up and resolution.
B2B healthcare providers benefit from centralized claims management, which streamlines workflows across multiple sites or specialties. Payer portals and electronic status updates allow teams to monitor claim progress and act quickly when issues arise.
Timely appeals are vital, especially for denials related to missing information or accident details. By standardizing follow-up processes, organizations can recover more revenue and keep medical insurance pay cycles moving smoothly.
Maximizing Reimbursements Through Payer Contract Analysis
Analyzing and negotiating payer contracts is a key strategy for maximizing medical insurance pay. Understanding each payer’s fee schedule, reimbursement methodologies, and policy exclusions helps identify underpayments and recoup lost revenue.
Regular contract reviews enable B2B practices to align rates with current market trends, ensuring competitiveness. Comparing Med Pay rates with standard health insurance reimbursements reveals opportunities for better terms.
Effective contract management also supports compliance and reduces disputes. By maintaining clear documentation and open dialogue with payers, organizations can secure optimal payment terms and strengthen financial stability.
Leveraging Data Analytics for Revenue Improvement
Data analytics transforms how organizations approach medical insurance pay. Custom dashboards highlight payment bottlenecks, denial trends, and payer performance, offering actionable insights for revenue cycle leaders.
By tracking metrics such as average payment cycles and denial reasons, providers can quickly identify areas for improvement. Predictive analytics also support cash flow forecasting, helping organizations plan for fluctuations in revenue.
Comparing Med Pay with traditional insurance payment cycles reveals valuable patterns. These insights empower B2B teams to make informed decisions, optimize workflows, and ultimately boost medical insurance pay outcomes.
Staff Training, Communication, and Process Alignment
Well-trained staff are essential for optimizing medical insurance pay. Cross-training teams on payer rules and documentation requirements ensures consistency at every stage of the revenue cycle.
Regular meetings and open communication channels keep everyone updated on policy changes and challenges. Educating front desk staff to handle Med Pay eligibility questions can prevent errors early in the process.
Aligning revenue cycle management processes with organizational goals fosters accountability and efficiency. When teams are empowered with the right knowledge, medical insurance pay results improve across the board.
The Role of Technology and Professional Services in Medical Insurance Pay
The landscape of medical insurance pay is evolving rapidly, and technology now sits at the heart of efficient revenue cycle management. For healthcare organizations, leveraging modern tools and professional services is essential for timely reimbursements, reduced denials, and sustained financial health.
Technology Tools for Efficient Claims and Payment Management
Modern healthcare organizations depend on robust technology platforms to manage the complexities of medical insurance pay. Industry-standard revenue cycle management (RCM) tools streamline critical processes, from eligibility checks to claim edits and payment posting. Integration with EHR and practice management systems enables seamless data flow, reducing manual entry and errors.
Automation is key. Real-time eligibility verification, automated claim scrubbing, and electronic remittance advice (ERA) posting accelerate payment cycles. For example, using automated Med Pay eligibility tools helps minimize denials and ensures prompt reimbursement. Adopting technology not only increases efficiency but also supports compliance efforts, as highlighted in Emerging Medical Billing Trends in 2026.
Partnering with Revenue Cycle Management (RCM) Service Providers
Outsourcing RCM functions to specialized service providers has become a strategic move for many healthcare organizations seeking to optimize medical insurance pay. Professional RCM partners bring deep expertise in payer rules, denial management, and compliance, which is critical in today’s regulatory environment.
These providers offer scalability for growing practices and multispecialty groups, adapting to client-owned software and existing workflows. By handling everything from Med Pay claims to complex payer negotiations, RCM partners free up internal resources to focus on patient care. When selecting an RCM service provider, consider their experience, transparency, and ability to manage diverse payer requirements efficiently.
How Greenhive Billing Solutions Enhances Medical Insurance Pay Processes
Greenhive Billing Solutions stands out by delivering comprehensive revenue cycle management tailored to healthcare providers. Our team manages every aspect of the medical insurance pay process, including eligibility verification, claims processing, denial management, and payment posting.
We prioritize HIPAA compliance and maintain open, transparent communication with clients. Our expertise covers Med Pay, auto insurance, government, and commercial payers, ensuring practices maximize reimbursements and minimize delays. By partnering with Greenhive, organizations benefit from faster payment cycles, reduced denial rates, and improved financial performance across the board.
Security, Compliance, and Data Privacy in Technology Adoption
Adopting technology for medical insurance pay requires a steadfast commitment to security and compliance. All tools and platforms must align with HIPAA guidelines, ensuring secure data transmission and storage. Role-based access controls and comprehensive audit trails are vital for protecting patient information and supporting regulatory audits.
Healthcare organizations should establish robust protocols for breach response and reporting. Balancing innovation with regulatory requirements is essential for long-term success in managing medical insurance pay. Staff training and regular system reviews reinforce a culture of compliance and data privacy across the revenue cycle.
Trends, Challenges, and the Future of Medical Insurance Pay
The landscape of medical insurance pay is rapidly evolving, presenting both challenges and opportunities for B2B healthcare organizations. As payer policies shift, technology advances, and patient responsibilities increase, revenue cycle teams must remain agile to optimize financial performance. Understanding these trends is crucial for staying competitive and compliant in the years ahead.
Evolving Payer Policies and Reimbursement Models
Payer policies for medical insurance pay are shifting toward value-based reimbursement and bundled payment models. Instead of traditional fee-for-service, payers increasingly reward outcomes and efficiency. This trend requires providers to document care more thoroughly and collaborate across specialties.
Automation and artificial intelligence are also being adopted by payers to streamline claims adjudication. As a result, requirements for supporting documentation are rising, and timelines for payment may fluctuate. B2B healthcare organizations must monitor these changes closely, adapting workflows to ensure all medical insurance pay claims meet the latest criteria.
Increasing Patient Financial Responsibility and Its Impact
Patient financial responsibility continues to grow, with high-deductible health plans and cost-sharing arrangements becoming more common. According to projected industry data, employer health care costs are expected to rise significantly, putting added pressure on patients and providers alike.
Medical insurance pay options like Med Pay can help bridge gaps for accident-related care, but practices must educate patients and streamline billing to improve collections. As out-of-pocket expenses rise, clear communication and proactive patient engagement become vital in reducing bad debt and maintaining revenue.
Technology-Driven Innovation and Automation
Technology is revolutionizing medical insurance pay processes. AI-powered claims scrubbing, real-time eligibility checks, and robotic process automation are making tasks more efficient and reducing manual errors. Telehealth services are also integrating with insurance workflows, enabling faster reimbursement for virtual visits.
B2B healthcare organizations benefit from these innovations by improving claim accuracy, accelerating payment cycles, and freeing staff to focus on complex cases. Staying updated on the latest tools and ensuring all technology aligns with compliance standards will be key to maximizing medical insurance pay outcomes.
Preparing Your Organization for the Future of Medical Insurance Pay
To remain resilient, organizations should build agility into their medical insurance pay operations. Invest in continuous staff training, scenario planning for reimbursement changes, and regular process reviews. Engage with payer forums and industry associations to anticipate policy shifts and regulatory updates.
A proactive approach—combining technology adoption, data-driven decision-making, and strong payer relationships—will position B2B healthcare providers for sustained success. By focusing on adaptability and compliance, your organization can turn medical insurance pay challenges into opportunities for growth.
As you’ve seen throughout this guide, understanding the ins and outs of medical insurance pay is essential for maximizing reimbursements and staying compliant in today’s healthcare landscape. Whether you’re looking to reduce denials, improve your billing workflow, or simply gain peace of mind about your practice’s financial health, it helps to have expert eyes on your processes. If you’re curious about how your current approach measures up, or want tailored advice on optimizing your revenue cycle, I invite you to Get Your Free Audit. Let’s work together to set your organization up for success in 2026 and beyond.