Hospital revenue cycle management is the backbone of a hospital’s financial sustainability, directly impacting everything from operating margins to patient care quality. Consider this: U.S. hospitals lose billions each year because of avoidable RCM inefficiencies.
Mastering these processes not only strengthens cash flow but also reduces costly denials and enhances patient satisfaction across your organization.
This guide delivers a clear, step-by-step approach to hospital revenue cycle management, offering expert insights and practical strategies to drive results. Discover essential RCM components, key challenges, optimization techniques, compliance priorities, future trends, and actionable solutions tailored for hospitals and health systems.
Understanding the Hospital Revenue Cycle: Core Components and Key Players
Effectively managing hospital revenue cycle management is essential for financial stability and operational excellence. The process encompasses every step from patient intake to payment collection, requiring coordination, expertise, and continuous improvement. Let’s examine the building blocks, stakeholders, metrics, and financial implications that define a successful RCM program.
![]()
Defining Revenue Cycle Management in Hospitals
Hospital revenue cycle management refers to the end-to-end process of capturing, managing, and collecting patient service revenue. It starts with pre-registration, continues through registration, charge capture, coding, claim submission, payment posting, and concludes with collections. Each phase has a direct impact on cash flow and hospital margins.
Unlike physician practice RCM, hospitals manage more complex billing structures, larger patient volumes, and intricate payer contracts. These differences require specialized processes and deeper compliance oversight.
For a detailed breakdown of this process, explore the revenue cycle medical billing process. Mastering each step of hospital revenue cycle management is critical for reducing revenue leakage and supporting long-term sustainability.
Key Stakeholders and Roles in the RCM Process
Hospital revenue cycle management depends on seamless collaboration among internal and external stakeholders. Internal teams include front desk staff, billing and coding specialists, finance, IT, and compliance officers. Each group plays a pivotal role in accurate data entry, charge capture, and regulatory adherence.
Externally, payers, clearinghouses, and RCM service providers are vital partners. They help process claims, manage denials, and ensure payment is received efficiently. Regular communication and well-defined workflows between all parties are essential for smooth hospital revenue cycle management and minimized payment delays.
Critical Metrics and KPIs for Hospital RCM Success
Tracking key performance indicators is central to hospital revenue cycle management improvement. Core metrics include Days in Accounts Receivable (industry benchmark: 40–50 days), Clean Claim Rate (goal: 90%+), Denial Rate (target: under 5–10%), Net Collection Rate (aim: 95%+), and Cost to Collect (typically 3–5% of revenue).
| KPI | Benchmark |
|---|---|
| Days in A/R | 40–50 days |
| Clean Claim Rate | 90%+ |
| Denial Rate | <10% |
| Net Collection Rate | 95%+ |
| Cost to Collect | 3–5% |
Consistent monitoring of these KPIs within hospital revenue cycle management enables teams to identify bottlenecks, benchmark performance, and drive ongoing process improvements.
Financial Impact of Effective RCM on Hospitals
Inefficient hospital revenue cycle management can result in millions of dollars lost every year due to claim denials, underpayments, or delayed reimbursements. Recent studies show some hospitals experience 3–5% revenue leakage, severely impacting margins and growth.
Hospitals that invest in optimized RCM processes report substantial improvements in operating margins, often freeing up capital for patient care initiatives and facility expansion. These gains extend beyond financial health, supporting better patient experiences and organizational stability.
Current Challenges and Pain Points in Hospital Revenue Cycle Management
Hospital revenue cycle management faces a complex array of challenges that directly impact financial performance and patient care. Navigating these pain points requires a strategic, coordinated effort among hospital leaders and RCM professionals. Below, we explore the most pressing obstacles hospitals encounter in optimizing their revenue cycle.
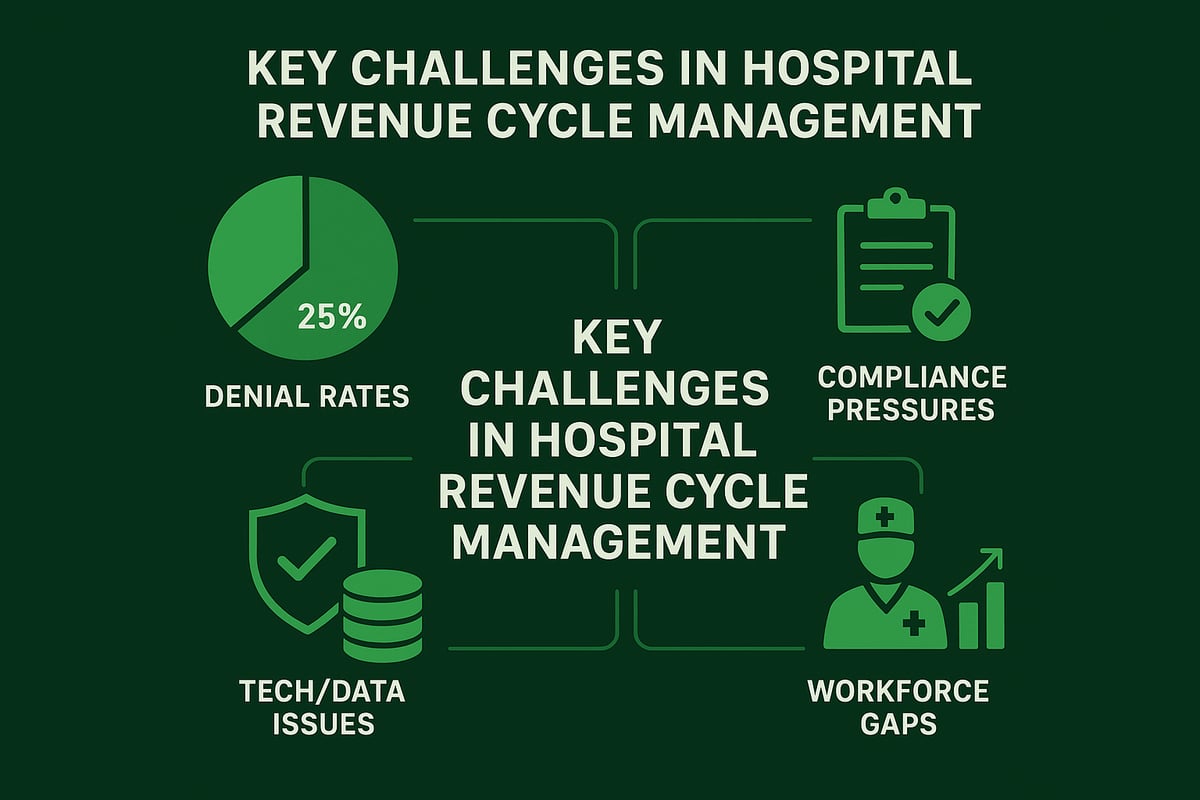
Common Operational and Financial Obstacles
One of the most significant pain points in hospital revenue cycle management is the high rate of claim denials. These denials often stem from coding errors, insurance eligibility issues, or incomplete documentation. Each denied claim not only delays reimbursement but also increases the administrative workload as teams must rework and resubmit claims.
Delayed payments can create cash flow bottlenecks, directly affecting a hospital’s ability to invest in patient care and innovation. The administrative cost to collect each dollar continues to rise, driven by manual processes and complex payer requirements. Hospitals must address these operational inefficiencies to remain financially sustainable. For deeper insights into effective denial management strategies, see Denial management strategies.
Regulatory and Compliance Pressures
Hospital revenue cycle management is under constant scrutiny due to evolving regulations such as HIPAA and CMS guidelines. Staying compliant with changing payer policies and government mandates is a persistent challenge. Hospitals must ensure accurate documentation and billing practices to avoid compliance violations.
Non-compliance can result in significant financial penalties, legal action, and reputational harm. Documentation and coding requirements frequently change, making it difficult for staff to keep up. Proactive monitoring and regular training are essential to mitigate compliance risks and maintain efficient hospital revenue cycle management.
Technology Integration and Data Management Issues
Fragmented EHR and billing systems are a major obstacle in hospital revenue cycle management. Data silos prevent seamless information sharing between departments, slowing down claim processing and increasing the risk of errors. Lack of interoperability among platforms makes end-to-end revenue cycle visibility difficult.
Cybersecurity threats are also on the rise, with hospitals becoming frequent targets of ransomware and data breaches. Protecting sensitive patient and financial data is critical for trust and regulatory compliance. Addressing these technical challenges is vital for a secure and efficient hospital revenue cycle management process.
Workforce and Training Gaps
The shortage of skilled professionals in hospital revenue cycle management continues to strain operations. High turnover rates and the ongoing need for specialized training increase costs and disrupt workflow continuity. Inexperienced staff are more likely to make mistakes in claim submission and coding, leading to higher denial rates.
Training programs and clear career paths are essential to attract and retain talent. Investing in staff development not only improves claim accuracy and processing speed but also enhances overall hospital revenue cycle management performance. A strong workforce is the backbone of a resilient and responsive RCM operation.
Step-by-Step Guide to Optimizing Hospital Revenue Cycle Management
A robust hospital revenue cycle management process is built on a foundation of stepwise optimization. Each stage in the revenue cycle contributes to financial stability, regulatory compliance, and patient satisfaction. By addressing every link in the chain, hospitals can minimize revenue leakage, accelerate reimbursements, and reduce costly errors.
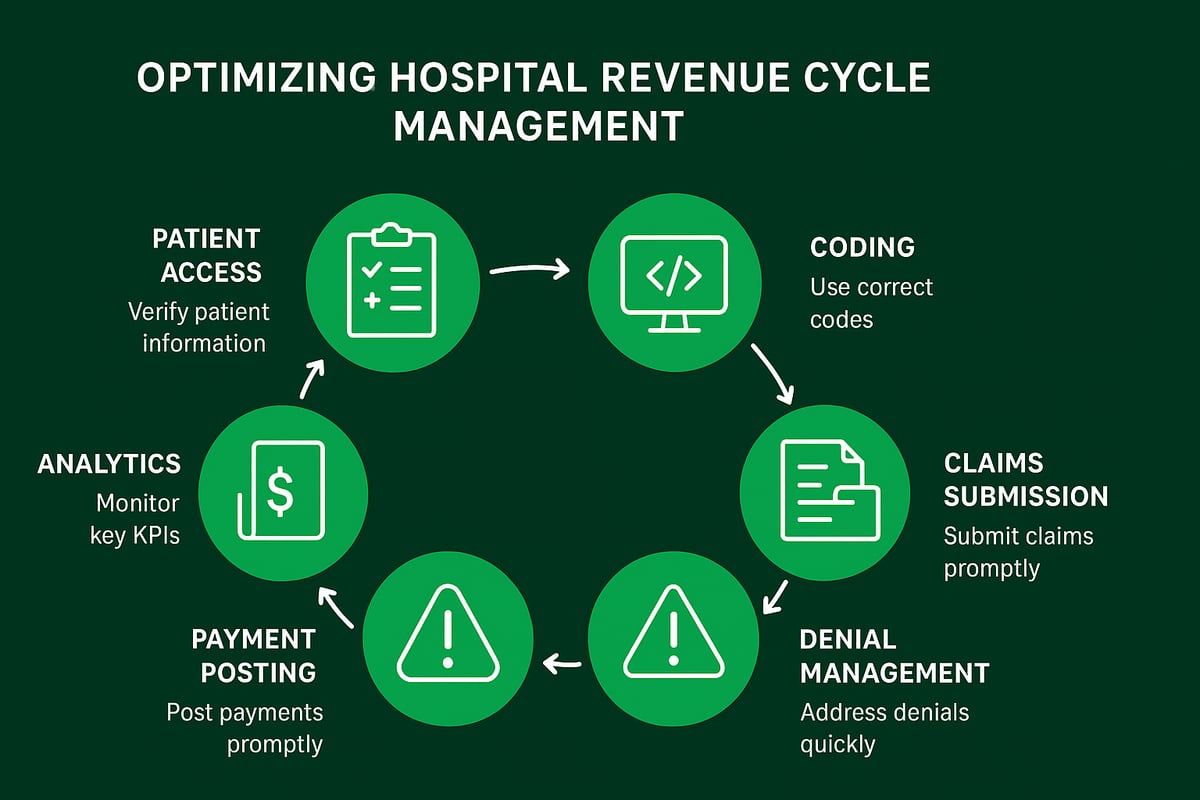
Step 1: Patient Access and Pre-Registration Optimization
The first step in hospital revenue cycle management begins before a patient arrives. Accurate insurance verification and eligibility checks are critical. Collecting demographic and financial data up front reduces the risk of errors that can lead to claim denials.
Front desk teams should confirm insurance details, capture patient information, and secure authorizations. Using standardized forms and checklists helps prevent missing data. Hospitals that streamline pre-registration see fewer billing issues and improved cash flow.
Optimizing this stage sets a positive tone for the entire hospital revenue cycle management process and supports a smoother patient experience.
Step 2: Charge Capture and Medical Documentation Best Practices
Effective hospital revenue cycle management relies on capturing all billable services accurately. Missed charges or incomplete documentation can result in significant revenue loss.
Best practices include:
- Real-time charge entry by clinical staff
- Regular reconciliation between clinical and billing systems
- Ongoing provider education on documentation requirements
| Common Pitfall | Solution |
|---|---|
| Missed ancillary services | Implement charge audits |
| Incomplete notes | Use clinical documentation templates |
| Delayed entry | Enable point-of-care charge capture |
Strong charge capture and documentation practices reduce downstream denials and support full reimbursement.
Step 3: Accurate Medical Coding and Billing
Certified coders are essential to hospital revenue cycle management. They ensure that clinical services are translated into standardized codes (ICD-10, CPT, HCPCS) for billing.
Correct coding not only speeds up reimbursement but also minimizes compliance risks. Regular audits and double-checks catch errors before claims are submitted. For a deeper dive on this topic, see Medical coding in revenue cycle management.
Investing in ongoing coder training and leveraging coding guidelines ensures claims are clean, reducing rejections and improving hospital revenue cycle management performance.
Step 4: Efficient Claims Submission and Follow-Up
Timely and accurate claim submission is a cornerstone of hospital revenue cycle management. Electronic claims, routed through clearinghouses, accelerate the process and minimize manual errors.
Follow-up is equally important. Dedicated teams should track unpaid or denied claims, identify bottlenecks, and communicate with payers promptly. Automation tools can flag claims needing attention.
Hospitals that prioritize claims management reduce reimbursement delays and maintain a healthier cash flow, strengthening the overall hospital revenue cycle management system.
Step 5: Denial Management and Appeals Process
Denials are a persistent challenge in hospital revenue cycle management. Identifying root causes—such as coding errors or missing documentation—is the first step toward resolution.
A standardized denial management workflow typically includes:
- Categorizing denial reasons
- Assigning ownership for follow-up
- Tracking appeal outcomes
Developing effective appeals strategies and monitoring trends over time helps recover lost revenue. Proactive denial management ultimately boosts financial performance and ensures a more resilient hospital revenue cycle management operation.
Step 6: Payment Posting, Patient Billing, and Collections
Accurate payment posting is vital to hospital revenue cycle management. Automating this process reduces errors and speeds up reconciliation.
Clear, patient-friendly billing statements improve transparency and satisfaction. Offering multiple payment options and clear instructions can increase collection rates. Hospitals should monitor accounts for overdue balances and implement respectful, consistent follow-up procedures.
By refining payment posting and collections, organizations decrease bad debt and enhance the efficiency of hospital revenue cycle management.
Step 7: Continuous Monitoring, Reporting, and Improvement
Ongoing performance monitoring is essential for sustainable hospital revenue cycle management. Tracking KPIs such as Days in A/R, Clean Claim Rate, and Denial Rate provides actionable insights.
Dashboards and regular audits help identify trends, bottlenecks, and opportunities for process enhancements. Establishing feedback loops encourages staff engagement and fosters a culture of continuous improvement.
Hospitals that embrace data-driven decision making maintain financial health and are better equipped to adapt to industry changes, keeping hospital revenue cycle management strong and future-ready.
Leveraging RCM Service Providers for Hospital Success
Outsourcing hospital revenue cycle management has become a strategic move for many healthcare organizations seeking efficiency and stability. By partnering with experienced RCM service providers, hospitals can address rising administrative costs, reduce errors, and unlock access to specialized expertise. This approach enables internal teams to focus on core patient care, while external partners handle complex billing processes.
Effective outsourcing can lead to improved cash flow, faster reimbursements, and enhanced compliance. Many hospitals see measurable gains in productivity and reductions in denied claims after transitioning to professional RCM services.
The Strategic Value of Outsourcing RCM Services
Hospitals face mounting pressure to manage costs and improve outcomes. Outsourcing hospital revenue cycle management offers several compelling advantages:
- Cost savings: Reduce overhead and operational expenses.
- Scalability: Adapt quickly to volume changes without staffing bottlenecks.
- Expertise: Access RCM professionals skilled in complex payer rules and regulations.
- Error reduction: Minimize costly mistakes in coding, billing, and collections.
For many organizations, the decision to outsource is driven by the need for predictable results and the ability to respond to industry changes. Case studies consistently show that hospitals leveraging RCM service providers achieve higher clean claim rates and improved financial performance.
How to Select the Right RCM Partner
Choosing the right partner for hospital revenue cycle management requires careful consideration. Start by evaluating the provider’s track record in the hospital sector, ensuring they understand your specialty and regulatory requirements.
Key criteria include:
- Experience: Years in hospital RCM and references from similar clients.
- Compliance: Adherence to HIPAA, CMS, and payer policies.
- Technology compatibility: Ability to integrate with your EHR and billing systems.
- Transparency: Clear communication and reporting protocols.
Ask potential partners about their approach to denial management, data security, and ongoing staff training. A detailed service-level agreement and regular performance reviews help foster a transparent, accountable relationship.
Greenhive Billing Solutions: Comprehensive RCM Services for Hospitals
Greenhive delivers tailored hospital revenue cycle management services designed to boost operational efficiency and financial health. Our offerings span end-to-end billing, certified coding, claims processing, denial management, and in-depth analytics.
We prioritize HIPAA compliance and provide transparent, value-based pricing to ensure measurable ROI for hospital clients. Leveraging a skilled team, we adapt to the client’s existing systems and workflows, minimizing disruption.
For example, by implementing robust denial management in medical billing, Greenhive has helped hospitals lower denial rates and accelerate reimbursements. Clients report significant cost savings and improved claim accuracy after transitioning to our services.
Ensuring a Smooth Transition and Maximizing ROI
A successful transition to outsourced hospital revenue cycle management starts with a structured onboarding plan. Key steps include open communication, clear documentation handoff, and collaborative workflow mapping.
Change management is essential: provide training for both internal and external teams to ensure seamless integration. Regular check-ins and performance tracking help identify early wins and areas for improvement.
Measure ROI through key metrics such as days in A/R, denial rates, and net collection percentages. Ongoing collaboration with your RCM partner is vital for sustained financial performance and compliance.
Compliance, Security, and Regulatory Considerations in Hospital RCM
Healthcare regulations are constantly evolving, and their impact on hospital revenue cycle management cannot be overstated. Regulatory frameworks such as HIPAA, HITECH, and CMS rules set rigorous standards for data privacy, billing, and claims integrity. Recently, government mandates and payer policies have become more complex, placing increased pressure on hospitals to adapt their processes. According to hospital RCM market growth projections, the industry’s expansion is tightly linked to compliance readiness and the ability to implement regulatory changes quickly. Staying up-to-date with new rules and payer requirements is essential for maintaining operational efficiency and protecting revenue streams.
Navigating Evolving Healthcare Regulations
The regulatory landscape for hospital revenue cycle management is both dynamic and demanding. Hospitals must comply with HIPAA for patient privacy, HITECH for health IT security, and CMS rules for billing and reimbursement. Each year, new payer policies and government mandates require hospitals to update their procedures and documentation. Failure to comply can result in audits, denied claims, and significant financial penalties. Proactive monitoring of regulatory updates, along with clear internal communication, helps organizations minimize risk and maintain compliance. Having designated compliance officers and regular policy reviews supports a sustainable approach.
Data Security and Patient Privacy in the Revenue Cycle
Protecting sensitive patient data is a cornerstone of hospital revenue cycle management. The increasing volume of digital health information, coupled with frequent cyber threats, demands robust security measures. Hospitals must safeguard electronic health records, billing data, and all points of data exchange. Best practices include encrypting data, implementing role-based access controls, and performing regular vulnerability assessments. Staff training is critical, as human error remains a leading cause of breaches. For an in-depth look at recent cybersecurity threats and mitigation strategies, see cybersecurity challenges in hospital RCM. Effective data security not only ensures compliance but also builds patient trust and protects financial outcomes.
Auditing, Documentation, and Risk Management
Regular audits are vital for identifying gaps in hospital revenue cycle management processes and ensuring regulatory compliance. Internal and external audits help validate billing accuracy, coding integrity, and adherence to payer requirements. Maintaining comprehensive documentation for all services, claims, and communications is essential for audit readiness. Risk management also involves monitoring for potential fraud or abuse, as well as responding quickly to identified issues. By integrating audit findings into ongoing process improvements, hospitals can prevent revenue leakage and avoid costly penalties. A robust risk management framework supports both compliance and long-term financial sustainability.
Building a Culture of Compliance Across the Hospital
Creating a culture of compliance is foundational to successful hospital revenue cycle management. Leadership must set the tone, prioritizing regulatory adherence and ethical practices. This commitment should be reflected in clear policies, ongoing staff education, and open channels for reporting concerns. Regular training programs keep teams current on new regulations, documentation standards, and security protocols. Encouraging accountability at every level ensures that compliance is a shared responsibility. Hospitals that foster this culture not only reduce risk but also enhance operational performance and patient satisfaction.
Future Trends and Innovations in Hospital Revenue Cycle Management
Staying ahead in hospital revenue cycle management requires awareness of emerging trends and innovations. Hospitals and healthcare organizations must continually adapt to evolving technology, patient preferences, and regulatory shifts to maintain financial health and operational efficiency.
The Rise of Automation and Artificial Intelligence in RCM
Automation and artificial intelligence are transforming hospital revenue cycle management by streamlining complex processes like claims management, coding, and collections. These technologies help minimize human error, accelerate task completion, and reduce administrative costs.
Hospitals leveraging advanced AI tools can automate routine tasks, such as eligibility verification and claim status checks, freeing staff to focus on higher-value activities. For a deeper dive into how organizations are utilizing these innovations, explore AI and automation in RCM.
Key benefits include:
- Faster claim processing and payment cycles
- Improved accuracy in coding and billing
- Reduced denial rates and rework
Adopting automation strengthens hospital revenue cycle management and positions organizations for future growth.
Value-Based Care and Its Impact on RCM
The shift from fee-for-service to value-based care models is reshaping hospital revenue cycle management. Hospitals must now align financial processes with quality metrics, patient outcomes, and bundled payments.
This approach rewards efficiency and quality rather than service volume. It requires new RCM strategies, such as tracking performance against outcome-based contracts and adjusting billing workflows to accommodate risk-sharing arrangements.
Hospitals succeeding under value-based models:
- Integrate clinical and financial data for comprehensive reporting
- Monitor patient outcomes alongside revenue metrics
- Adapt to changing payer requirements and incentive structures
Value-based care challenges traditional hospital revenue cycle management, but it also unlocks opportunities for sustainable financial performance and improved patient care.
Patient Financial Experience and Consumerization
Today’s patients expect transparency, convenience, and digital-first experiences from their healthcare providers. Hospital revenue cycle management must evolve to meet these consumer demands and improve satisfaction.
Enhancements in patient billing include:
- Clear, itemized statements and upfront cost estimates
- Digital payment options and self-service portals
- Flexible payment plans and real-time support
By prioritizing the patient financial journey, hospitals can increase collections, reduce bad debt, and foster loyalty. Investing in a patient-centric hospital revenue cycle management strategy not only benefits the bottom line but also elevates the overall care experience.
Interoperability and Data Analytics in RCM
Seamless data exchange and robust analytics are critical for modern hospital revenue cycle management. Integrating electronic health records (EHR) with billing systems enables real-time access to accurate data, streamlining claim submission and reducing delays.
Advanced analytics tools help organizations:
- Track key performance indicators (KPIs) and uncover revenue opportunities
- Identify root causes of denials or payment bottlenecks
- Benchmark results against industry standards
For actionable insights on leveraging analytics in RCM, visit Healthcare revenue cycle analytics. Embracing interoperability and analytics empowers hospitals to make informed decisions, optimize workflows, and drive continuous improvement in hospital revenue cycle management.
Workforce Evolution and RCM Talent Management
The workforce supporting hospital revenue cycle management is undergoing rapid change. As automation takes over routine tasks, the demand for skilled professionals who can manage complex cases, interpret data, and ensure compliance is rising.
Key trends include:
- Upskilling staff to use new technologies and analytics tools
- Increasing adoption of remote and hybrid work models
- Implementing retention programs to reduce turnover
Effective talent management ensures hospital revenue cycle management teams are adaptable, knowledgeable, and ready to navigate industry shifts. Investing in workforce development secures long-term organizational resilience.
Preparing for the Next Wave: Regulatory, Technological, and Market Shifts
Regulatory updates, technological advancements, and shifting market dynamics will continue to shape hospital revenue cycle management. Hospitals need to anticipate these changes and build flexible strategies to stay compliant and competitive.
Action steps for future readiness:
- Monitor evolving compliance requirements and payer models
- Invest in adaptable RCM infrastructure and external partnerships
- Promote continuous learning and proactive planning
Building a culture of innovation ensures hospital revenue cycle management remains agile, responsive, and effective. By embracing change and prioritizing strategic investment, organizations can secure both financial stability and operational excellence.
After exploring the key strategies and future trends in hospital revenue cycle management, you might be wondering how your own processes measure up. With so many moving parts—compliance, technology, patient experience, and more—it's crucial to know where you stand and where you can improve. That's why taking the next step with a free audit can be so valuable. You'll get a clear, expert perspective on your current strengths and areas for growth, helping you maximize reimbursements and streamline your operations for 2026 and beyond. Ready to gain actionable insights? Get Your Free Audit