Home care is transforming healthcare delivery, making it crucial for providers to master pos 12 in medical billing for accurate reimbursement and financial health in 2026.
This comprehensive guide breaks down the complexities of pos 12 in medical billing, offering clear strategies for compliance and revenue optimization.
You will discover the definition and purpose of pos 12, key reimbursement changes for 2026, credentialing essentials, steps to prevent claim denials, telehealth integration, and future-ready best practices.
As home-based care gains momentum, understanding pos 12 in medical billing is vital. Unlock expert-backed strategies to streamline billing, reduce denials, and position your practice for success.
Understanding POS 12: Definition, Purpose, and Scope
What is POS 12 in Medical Billing?
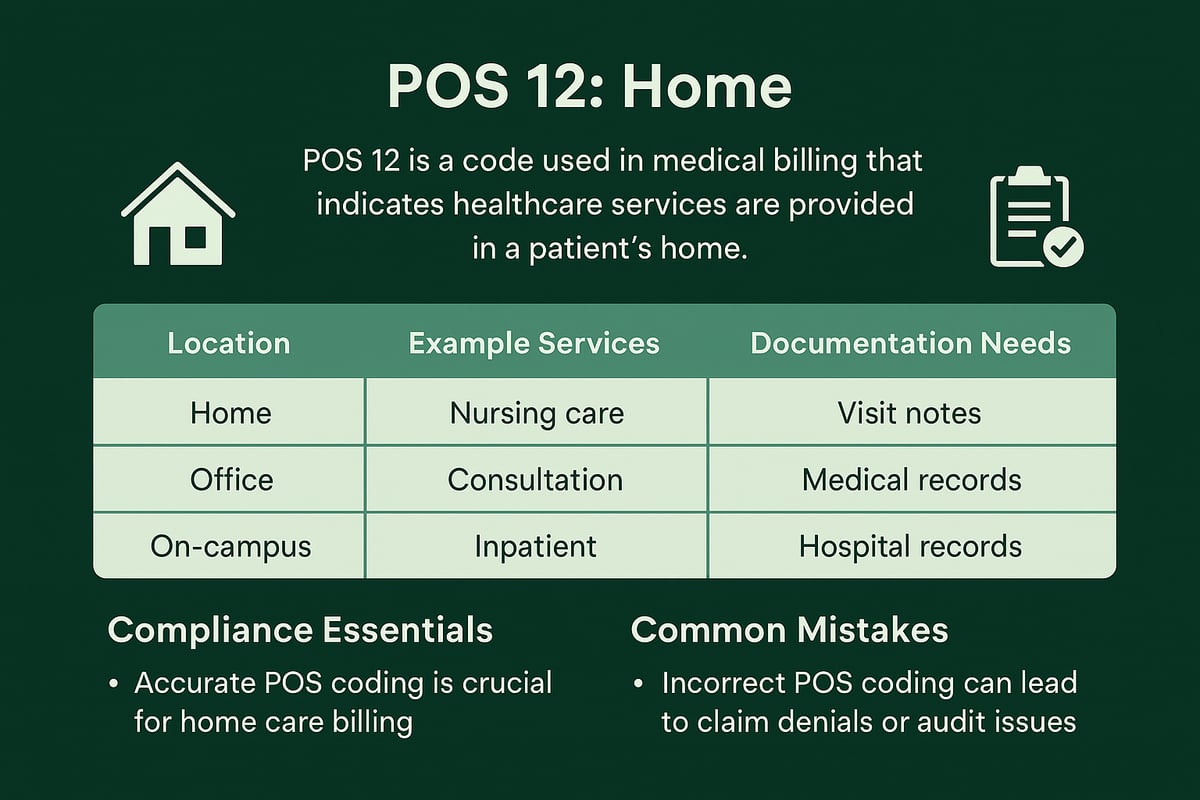
POS 12 in medical billing refers to the code used to indicate that a healthcare service was delivered in the patient’s private residence. According to CMS, POS 12 is defined as “Patient’s Home,” differentiating it from locations like offices (POS 11) or outpatient hospitals (POS 22).
This code is essential for home health services, physical therapy, rehabilitation, and certain telehealth appointments conducted at home. For example, when a nurse visits a patient’s home for wound care or a physical therapist provides in-home rehab, POS 12 must be used on the claim. Accurate use of pos 12 in medical billing ensures that claims are processed correctly and reimbursement is not jeopardized.
| POS Code | Location | Example Services |
|---|---|---|
| 12 | Patient’s Home | Home health, in-home rehab, some telehealth |
| 11 | Office | Standard office visits |
| 22 | Outpatient Hospital | Outpatient procedures, diagnostics |
Why Accurate POS 12 Coding Matters in 2026
Accurate use of pos 12 in medical billing is more important than ever as payer scrutiny intensifies. Errors in coding can lead to denials, delayed payments, or even compliance investigations. With the growing shift toward home-based care, payers and auditors are closely monitoring claims for correct POS usage.
Recent data shows that mistakes with POS codes are a leading cause of Medicare and Medicaid billing denials. In 2026, as home care expands, providers must be vigilant in using POS 12 correctly to avoid costly setbacks. Compliance risks and financial losses are significant if claims are miscoded or lack required documentation.
Common Scenarios for POS 12 Usage
Healthcare providers use pos 12 in medical billing in several scenarios:
- A credentialed clinician travels to the patient’s home for a routine checkup or chronic disease management.
- Patients with mobility challenges receive ongoing care at home.
- Post-acute rehabilitation is delivered within the patient’s residence.
- Telehealth sessions are conducted, with the patient located at home and eligible under payer guidelines.
It is crucial to avoid inappropriate use, such as assigning POS 12 for visits that occur in clinics or facilities. Each payer may have specific requirements, especially for telehealth, so staying updated on policy changes is vital.
Regulatory and Compliance Foundations
Regulatory bodies like CMS and commercial payers set strict requirements for pos 12 in medical billing. Proper documentation must include the patient’s home address, provider credentials, and medical necessity. Providers must be credentialed for home care billing and follow updated regulatory guidelines.
Recent years have seen increased penalties for errors or fraudulent POS usage. To avoid these pitfalls, reviewing common mistakes with POS codes can help providers strengthen compliance and reduce denial risks. Staying proactive with credentialing and documentation protects both financial and legal interests.
2026 Reimbursement Landscape for POS 12 Home Care
Understanding the 2026 reimbursement landscape for pos 12 in medical billing is essential for home care providers aiming to secure accurate payments and stay compliant. As payer rules evolve, mastering these nuances will be crucial for financial success and audit readiness.
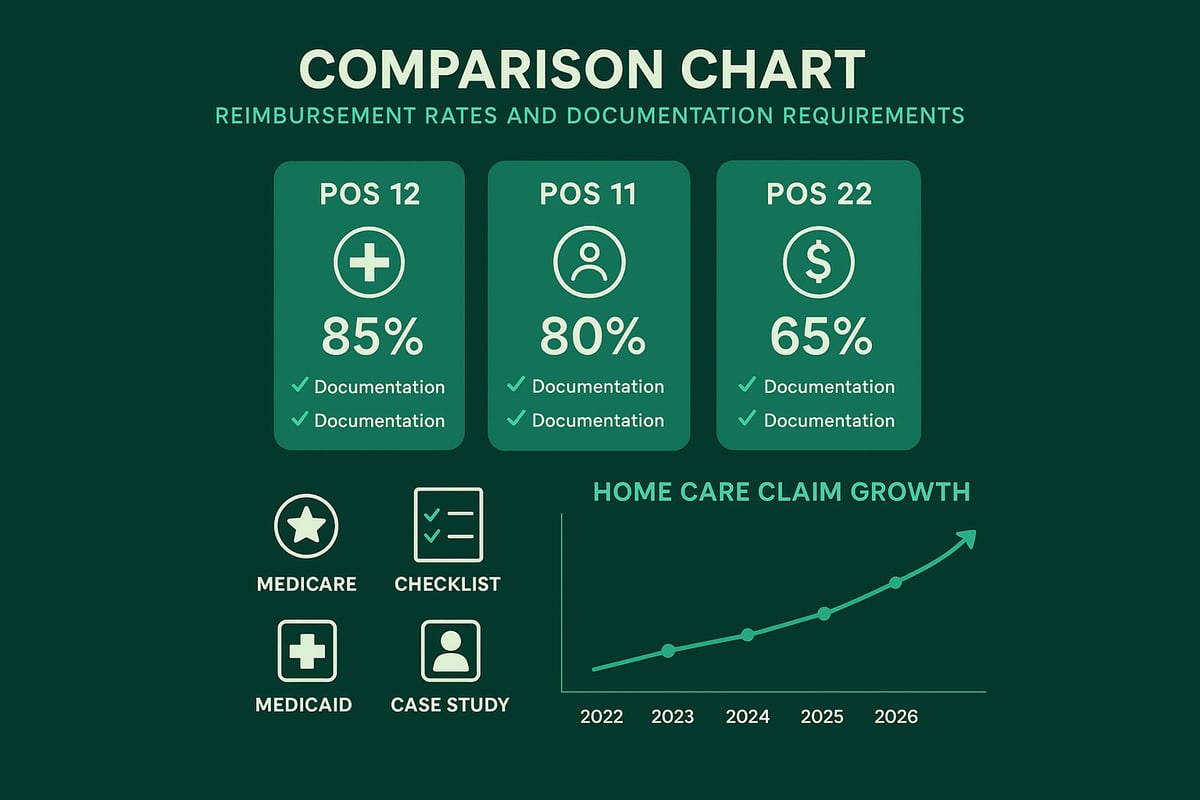
Key Differences: POS 12 vs. POS 11 and POS 22
Choosing the correct place of service code is a foundational step in pos 12 in medical billing. Each code signals a different care setting, impacting reimbursement, credentialing, and documentation.
| POS Code | Setting | Credentialing Needed | Reimbursement | Documentation Focus |
|---|---|---|---|---|
| POS 12 | Patient’s Home | Yes | Home care fee | Patient address, home care |
| POS 11 | Office | Yes | Office fee | Clinic location, visit |
| POS 22 | Outpatient Hospital | Yes | Hospital fee | Facility, procedure notes |
Billing an office or hospital code for a home visit can trigger denials, delay payment, and raise compliance flags. Ensuring correct use of pos 12 in medical billing is vital for smooth claims processing.
Medicare, Medicaid, and Commercial Payer Policies
Medicare sets a high bar for pos 12 in medical billing, demanding detailed documentation, proof of medical necessity, and active provider enrollment. Medicaid rules vary by state, with some offering expanded home care benefits and others applying stricter limitations.
Commercial payers often align with Medicare but may have unique requirements or reimbursement rates for POS 12. Some payers offer parity with office visits, while others apply lower fee schedules. Reviewing contracts annually and clarifying payer-specific policies helps avoid costly surprises and ensures compliant use of pos 12 in medical billing.
Documentation and Billing Essentials for POS 12
Accurate documentation is the backbone of successful pos 12 in medical billing. Every claim must clearly state the patient’s home address, the provider’s credentials, and specific details of the service rendered.
Common pitfalls include failing to specify the home setting, omitting proof of medical necessity, or missing required elements in visit notes. Providers can use a checklist to ensure compliance:
- Patient home address on claim
- Provider NPI and credentials
- Detailed description of service
- Signed visit note and care plan
Leveraging EHR or EMR systems to prompt for pos 12 in medical billing details reduces errors and supports clean claim submission.
2026 Payment Trends and Forecasts
The financial landscape for pos 12 in medical billing is rapidly shifting as home care gains a larger share of healthcare spending. CMS projects continued growth in home health expenditures, with hybrid care models (combining in-person and telehealth) further expanding billing opportunities.
Recent updates, such as those highlighted in the CMS 2026 Home Health Final Rule Insights, include payment adjustments, quality reporting changes, and new compliance standards. Analysts expect home care claims to rise significantly by 2026, making proactive adaptation essential for providers who rely on pos 12 in medical billing.
Real-World Examples and Case Studies
A home-based physical therapy practice optimized its pos 12 in medical billing by standardizing documentation and training staff. As a result, they saw faster reimbursements and fewer denials. In contrast, a provider who incorrectly billed an office code for a home visit faced repeated denials until correcting the POS.
Audits in 2025 revealed that most denied claims stemmed from documentation gaps or credentialing issues. Key takeaways for providers include regular internal audits, ongoing education, and using technology to flag errors before submission. Mastery of pos 12 in medical billing is a proven path to more consistent revenue and fewer billing headaches.
Credentialing, Compliance, and Provider Readiness for POS 12
Ensuring readiness for pos 12 in medical billing means providers must focus on credentialing, compliance, denial prevention, and team preparedness. Home care billing in 2026 is increasingly complex, and staying current with requirements is vital for financial and regulatory success.
Credentialing Requirements for Home Care Billing
Proper credentialing is a non-negotiable step for pos 12 in medical billing. Providers must be enrolled and approved with Medicare, Medicaid, and commercial payers before billing for home care services. Missing credentialing leads to instant denials and can trigger audits.
To start, review each payer’s enrollment process and keep all documentation up to date. Most payers require periodic renewals, so tracking expiration dates is key. The credentialing timeline varies, but delays can disrupt revenue flow.
For a step-by-step guide and best practices, see these Medical credentialing essentials. Investing in credentialing ensures eligibility for reimbursement and reduces risk.
Compliance Essentials: Avoiding Costly Mistakes
Compliance forms the backbone of pos 12 in medical billing. The most common errors include missing provider enrollment, incomplete documentation, and outdated records. Each payer may have unique rules for home health credentialing, making it essential to stay organized.
Strategies for compliance:
- Maintain an updated roster of enrolled providers.
- Audit records regularly for accuracy.
- Implement checklists for required documentation.
Routine internal audits can catch problems before they impact claims. Staying compliant not only protects your revenue but also shields your practice from regulatory penalties.
Preventing Claim Denials and Revenue Loss
Denials for pos 12 in medical billing often stem from credentialing gaps, insufficient documentation, or mismatched place of service codes. According to industry data, home visit denial rates can spike when providers are not properly credentialed with payers.
A simple denial prevention workflow includes:
- Verify provider credentialing status before service.
- Double check all documentation and POS codes.
- Use denial tracking tools to spot trends.
Recurring denials can quickly erode practice revenue. By addressing root causes, providers can maintain a healthier revenue cycle and avoid cash flow disruptions.
Staff Training and Technology Integration
Continuous staff education is vital for accurate pos 12 in medical billing. Regular billing team training ensures everyone understands changing payer requirements and documentation standards.
Technology also plays a key role:
- Claim scrubbers catch errors before submission.
- EHR alerts help staff select correct POS codes.
- Automated credentialing trackers prevent lapses.
Practices that invest in staff training and technology report fewer denials and more efficient home care billing. A tech-enabled compliance checklist can drive ongoing improvements.
Greenhive Billing Solutions: Streamlining Home Care Billing
Comprehensive revenue cycle management is crucial for mastering pos 12 in medical billing. Greenhive’s solutions cover credentialing, compliance, and denial prevention from start to finish.
Key benefits include:
- Reduced accounts receivable days.
- Maximized reimbursements.
- Transparent, actionable reporting.
Practices leveraging expert RCM support achieve higher clean claim rates and fewer denials. Greenhive’s proven approach prepares providers for successful, future-ready home care billing.
Step-by-Step Guide: Billing Home Care Services with POS 12 in 2026
Navigating pos 12 in medical billing requires a structured approach for compliance and optimal reimbursement. This step-by-step guide breaks down each phase of the billing process, helping providers avoid common pitfalls and ensure financial success for home care in 2026.
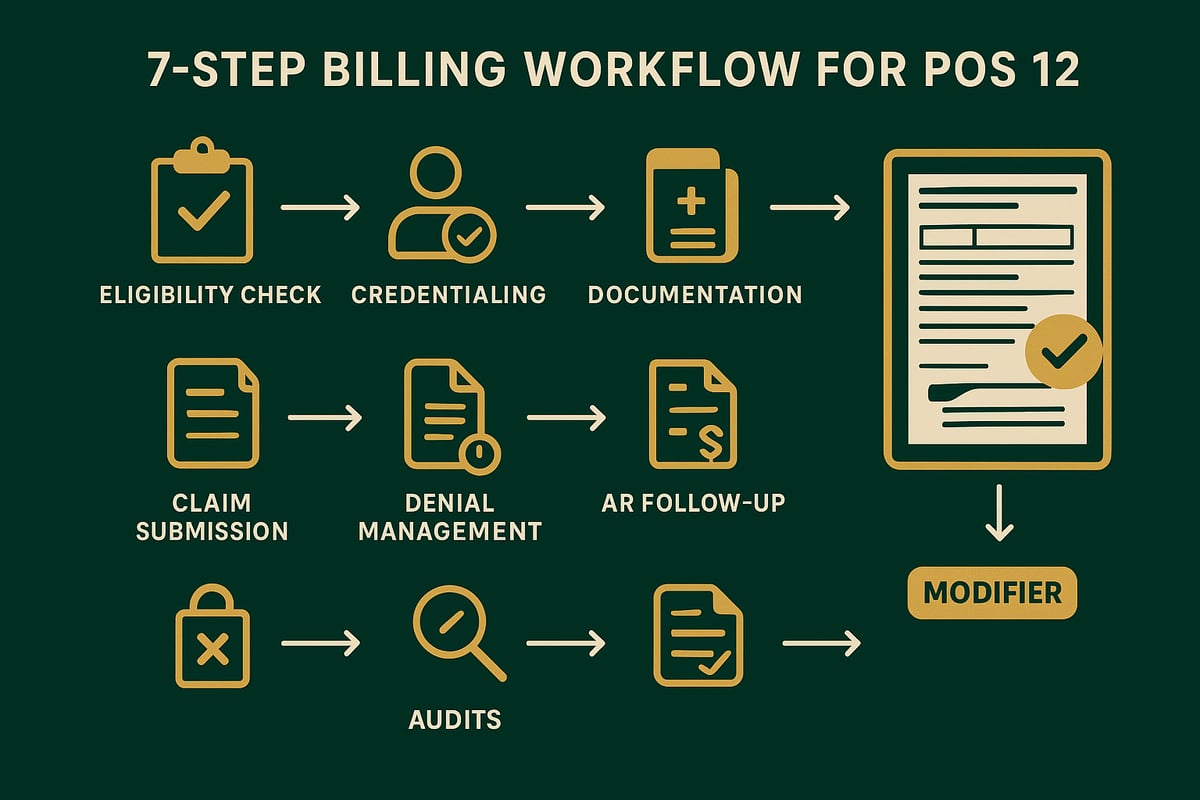
Step 1: Patient Eligibility Verification and Pre-Authorization
Start by confirming patient eligibility for home care services under pos 12 in medical billing. Contact payers to verify coverage, including any limitations on home-based care.
Check for pre-authorization requirements, which can vary by payer and service type. Always obtain authorization before scheduling the visit to prevent denials.
- Confirm insurance coverage for home care.
- Identify payer-specific rules for POS 12.
- Request pre-authorizations as needed.
A proactive eligibility check reduces the risk of rejected claims, setting a solid foundation for the rest of the billing process.
Step 2: Provider Credentialing Confirmation
Providers must be properly credentialed to bill using pos 12 in medical billing. Verify that all clinicians delivering home care are enrolled with Medicare, Medicaid, and commercial payers.
Keep credentialing documents up to date and track renewal dates. Integrate credentialing checks into your scheduling and billing workflows to avoid last-minute surprises.
- Confirm provider enrollment status.
- Maintain digital credentialing records.
- Set reminders for renewals.
Billing without valid credentialing leads to automatic denials and compliance issues, so make this step non-negotiable.
Step 3: Accurate Documentation and Coding
Accurate documentation is essential for pos 12 in medical billing. Always record the patient’s home address as the service location and include detailed visit notes supporting medical necessity.
Use the correct CPT or HCPCS codes in combination with POS 12 for each service provided. Ensure your EHR captures all required data fields.
Documentation Checklist:
- Patient’s home address
- Provider credentials
- Detailed service notes
- Medical necessity justification
Thorough documentation supports compliance and expedites claim approval.
Step 4: Claims Submission and Modifier Use
When submitting claims with pos 12 in medical billing, always indicate POS 12 clearly on the form. For telehealth services performed from the patient’s home, append the appropriate modifier, such as 95, to the CPT code.
Double-check all data for accuracy before submission. For more on correct modifier application, see Types of modifiers in billing.
- Select POS 12 as the place of service.
- Attach required modifiers for telehealth.
- Review claims for completeness prior to submission.
Proper modifier use is crucial for compliance and reimbursement.
Step 5: Monitoring and Managing Denials
Vigilant denial management is vital for pos 12 in medical billing. Monitor claims status regularly and identify any denials related to POS 12.
Analyze denial codes to spot patterns, such as credentialing lapses or documentation gaps. Develop a workflow to correct and resubmit denied claims promptly.
Denial Management Workflow:
- Track claim status daily.
- Identify root causes of denials.
- Initiate timely corrections and resubmissions.
Effective denial management preserves revenue and highlights process improvement opportunities.
Step 6: Accounts Receivable Follow-up and Appeals
Strong AR follow-up is crucial in pos 12 in medical billing. Review accounts receivable (A/R) reports to identify outstanding POS 12 claims.
Prioritize follow-up for denied or delayed payments. Prepare appeals with robust supporting documentation, including visit notes and pre-authorization records.
- Review A/R for POS 12 claims.
- Follow up with payers on delays.
- Submit detailed appeals as needed.
Timely follow-up and appeals can recover significant revenue that might otherwise be lost.
Step 7: Ongoing Process Improvement and Compliance Audits
Continuous improvement ensures long-term success with pos 12 in medical billing. Schedule regular audits of your home care billing processes to stay aligned with changing payer rules.
Update policies based on audit findings and payer bulletins. Invest in staff training and technology upgrades to streamline workflows.
Performance Benchmarks:
| Metric | Target Value |
|---|---|
| Clean Claim Rate | ≥ 95% |
| Denial Rate | < 5% |
| Days in A/R | < 30 days |
Benchmarking against industry standards keeps your billing future-ready and compliant.
Telehealth, Hybrid Care, and POS 12: 2026 Policy Updates
As telehealth and hybrid care models continue to expand, pos 12 in medical billing is at the center of these changes. Providers must stay informed on evolving rules to ensure accurate claims and maximize reimbursement for services delivered in the patient’s home.
Telehealth Billing from the Patient’s Home
Recent CMS policies confirm that pos 12 in medical billing must be used when telehealth services originate from the patient’s residence. Providers are required to include the correct place of service code and append modifiers such as 95, which designates a telehealth encounter.
For 2026, many payers are increasing scrutiny on these claims, making accurate coding and documentation essential. Hybrid care, which blends in-person and virtual visits, is also growing. For example, a patient may have an initial assessment at home, followed by virtual follow-ups, all billed with pos 12 in medical billing when appropriate.
2026 Regulatory Changes and Payer Updates
The regulatory landscape for pos 12 in medical billing is shifting, with new CMS and commercial payer updates extending telehealth reimbursement parity for home-based visits. Providers must follow the latest compliance requirements, including thorough documentation and correct use of place of service codes.
Recent data shows a steady increase in telehealth claims billed with pos 12 in medical billing between 2024 and 2026. For detailed insights into compliance pitfalls and billing errors, the OIG Audit on Home Health Compliance highlights the importance of precise coding and adherence to policy changes.
Billing Challenges and Solutions for Hybrid Care
Hybrid care introduces unique documentation demands for pos 12 in medical billing. Providers must clearly differentiate between in-person and telehealth encounters, using the right modifiers and codes. Common errors include missing modifiers, incorrect place of service entries, or incomplete visit notes, all of which can trigger denials.
To overcome these challenges, many practices are adopting integrated scheduling and billing platforms. These tools help ensure accurate code selection, automate modifier assignment, and flag incomplete records before claims are submitted. A recent case study showed that automated compliance checks led to a 15% reduction in hybrid care claim denials.
Preparing for Future Telehealth and Home Care Trends
Looking ahead, payer policies for remote and hybrid services will continue to evolve, making it vital to keep pos 12 in medical billing workflows up to date. Best practices include regular staff training, frequent policy reviews, and timely technology upgrades to adapt to regulatory shifts.
Staying informed through payer bulletins and industry resources is essential. For 2026, providers should prioritize action steps such as enhancing documentation protocols and leveraging analytics to monitor claim outcomes, ensuring future-ready billing for home-based and telehealth care.
Best Practices and Strategies for POS 12 Success in Home Care Billing
Achieving success with pos 12 in medical billing requires a proactive, multi-faceted approach. Providers must stay vigilant in every aspect of the billing cycle, from initial eligibility checks to ongoing process improvement. The following best practices will help ensure accurate claims, optimize reimbursement, and keep your home care billing future ready.
AR Management and Denial Prevention
Effective AR management is the backbone of pos 12 in medical billing. Begin by verifying patient eligibility for home care services before each visit. Regularly audit claims for accurate POS coding and watch for patterns in denials. Use denial codes to identify root causes and implement targeted solutions.
Practices that leverage Denial management best practices report fewer denials and faster payment cycles. Create a workflow that includes prompt follow up on outstanding claims, regular payer communication, and a system for tracking appeals. This approach helps maintain cash flow and reduces revenue leakage.
Staff Training and Process Automation
Staff education is essential for accurate pos 12 in medical billing. Schedule ongoing training sessions to keep billing teams updated on payer rules, documentation standards, and regulatory changes. Encourage staff to attend webinars, read payer bulletins, and participate in coding workshops.
Process automation can further reduce manual errors. Use claim scrubbers and automated POS selection tools to standardize workflows. Implement EHR alerts for missing documentation and credentialing gaps. Practices that automate key steps often see a significant drop in denials and increased billing efficiency.
Technology and Data Analytics in Home Care Billing
Leveraging technology is critical for optimizing pos 12 in medical billing. Integrate EHR and EMR systems to capture accurate POS data and streamline documentation. Set up dashboards to track denial rates, payment timelines, and clean claim rates.
Utilize analytics to pinpoint bottlenecks in your billing cycle and uncover new revenue opportunities. Incorporating Electronic Visit Verification Overview can further support compliance and ensure services are billed for the correct location. Data-driven improvements lead to more reliable reimbursement and fewer audit risks.
Patient Communication and Address Verification
Clear patient communication is a must for pos 12 in medical billing, especially when verifying addresses for home visits. Confirm the patient’s home address at every encounter to avoid mismatches and claim rejections. Provide patients with information about home care eligibility and billing procedures.
Develop a checklist for front office and clinical staff to ensure all address and service details are captured accurately. This step prevents denials linked to address errors and strengthens your documentation for audits. Strong communication builds trust and helps resolve billing questions quickly.
Continuous Improvement and Industry Benchmarking
Continuous improvement is crucial for staying ahead in pos 12 in medical billing. Set measurable KPIs such as clean claim rates, average days in AR, and denial percentages. Benchmark your performance against industry standards and peer organizations.
Regularly update internal policies based on changes from CMS and payers. Encourage a culture of feedback and learning within your billing team. By prioritizing ongoing education, policy reviews, and technology upgrades, your practice remains agile and ready for upcoming regulatory shifts.
Frequently Asked Questions: POS 12 in Medical Billing for 2026
Navigating pos 12 in medical billing can be challenging as home care regulations evolve. Below, you will find clear answers to the most common questions providers face about pos 12 in medical billing, helping ensure compliance, maximize reimbursement, and avoid costly errors in 2026.
When Should Providers Use POS 12?
Providers should use pos 12 in medical billing when delivering services in a private residence, not in a clinic or facility. Common scenarios include in-home nursing visits, physical therapy, and certain telehealth sessions where the patient is at home. Always confirm payer guidelines to ensure compliance. For example, Medicare and most commercial payers define pos 12 as the patient’s home, but state Medicaid rules may have additional requirements.
Review the 2026 Comprehensive Accreditation Manual for Home Care to stay updated on official standards for documentation and compliance. Avoid using pos 12 in medical billing for office-based or facility care, as this can result in claim denials.
What Are the Most Common POS 12 Billing Mistakes?
The most frequent mistakes with pos 12 in medical billing include:
- Submitting claims without proper provider credentialing for home care.
- Missing essential documentation, such as the patient’s home address.
- Failing to use required modifiers for telehealth claims.
- Confusing home care with office or facility visits and using the wrong POS code.
To prevent these errors, always verify credentialing status, update patient addresses at each encounter, and double-check coding rules before submitting pos 12 in medical billing claims.
How Do Reimbursement Rates Compare for POS 12?
Reimbursement rates for pos 12 in medical billing can differ significantly depending on the payer. Medicare typically offers a set fee schedule for home health, which may be higher or lower than office (POS 11) or outpatient hospital (POS 22) rates. Medicaid reimbursement varies by state, and commercial payers may provide parity or reduced rates for home visits.
| POS Code | Location | Typical Reimbursement* | Common Use |
|---|---|---|---|
| POS 12 | Patient’s Home | Varies (Medicare/Medicaid/Commercial) | Home health/telehealth |
| POS 11 | Office | Often baseline | Clinic/office |
| POS 22 | Outpatient Hosp | May be higher | Hospital outpatient |
*Always check specific payer contracts for current rates. Documentation, credentialing, and contract terms all influence the final payment for pos 12 in medical billing.
What Are the Latest Telehealth Changes for POS 12?
In 2026, telehealth policy updates continue to impact pos 12 in medical billing. CMS allows use of pos 12 for telehealth sessions when the patient is at home, with modifier 95 required to indicate virtual care. Commercial and Medicaid payers may have additional documentation standards or parity policies.
Telehealth claims using pos 12 in medical billing have grown since 2024, reflecting increased demand for remote care. Stay informed on each payer’s bulletins and update billing workflows to ensure correct coding and modifier use for telehealth originating from the patient’s home.
As you navigate the evolving landscape of home care billing, having a clear understanding of POS 12, compliance, and payer updates is crucial for securing accurate reimbursements and minimizing denials. If you want to make sure your billing processes are future ready and tailored to the latest 2026 requirements, you don’t have to do it alone. At Greenhive Billing Solutions, we’re here to help you streamline credentialing, prevent costly mistakes, and maximize your revenue cycle. If you’d like expert guidance specific to your practice, Book Your Free Consultation today.