Claim denials represent a significant financial and operational challenge for healthcare organizations, with recent data showing nearly one in five in-network claims are denied. Navigating the top 20 denial codes in medical billing can be overwhelming due to intricate policies and payer requirements. Billing teams and providers often face confusion, delays, and increased workloads as a result. However, understanding and addressing the most common denial codes can help streamline revenue cycle management, reduce administrative burdens, and accelerate cash flow. In this guide, you will discover the top 12 denial codes, proven strategies to resolve them, and best practices to minimize future denials.
Understanding Medical Billing Denial Codes
Understanding the top 20 denial codes in medical billing is crucial for healthcare organizations striving to protect revenue and streamline operations. Denial codes are more than just administrative hurdles—they are insight-rich signals that can reveal gaps in documentation, eligibility processes, and coding accuracy. For B2B healthcare providers, mastering these codes is a foundational step toward minimizing claim rejections and improving cash flow.
What Are Denial Codes and Why Do They Matter?
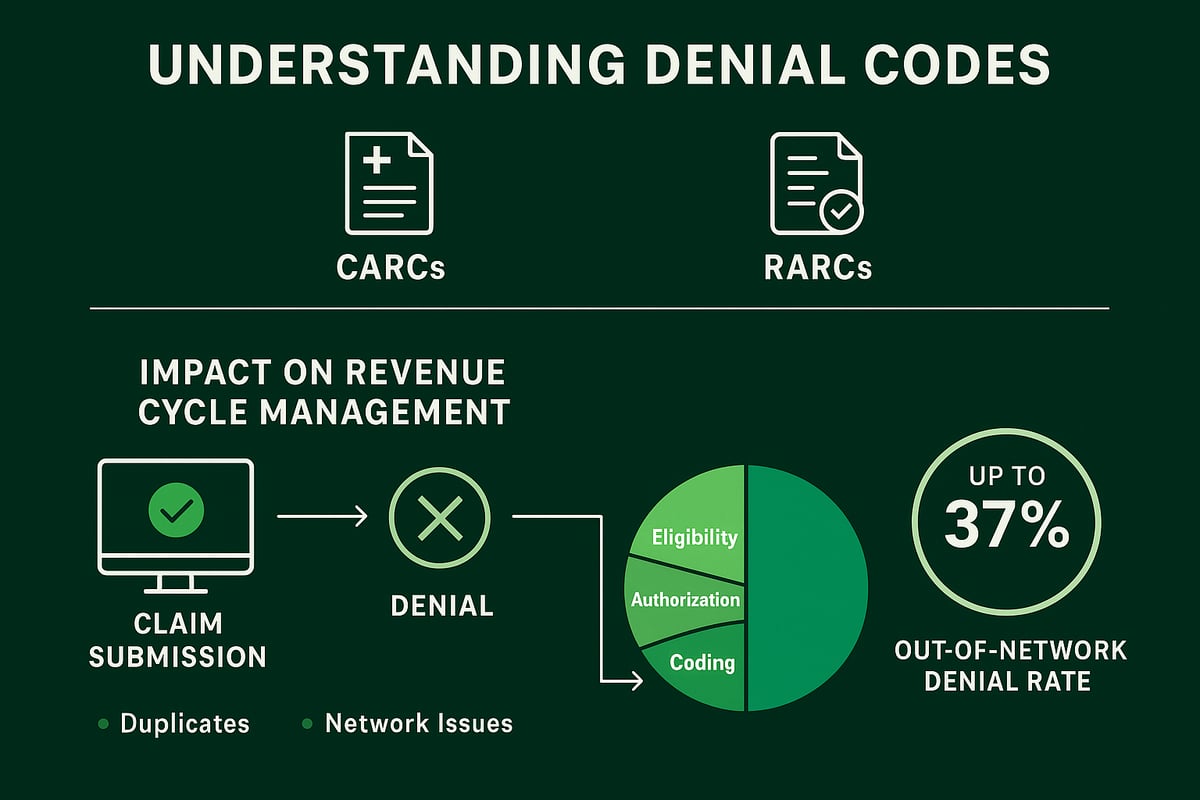
Denial codes are standardized explanations provided by payers to clarify why a healthcare claim has been rejected. The most common types are Claim Adjustment Reason Codes (CARCs) and Remittance Advice Remark Codes (RARCs), which together provide a detailed roadmap for resolving claim issues.
When a claim is denied, the assigned code tells billing teams exactly where the problem lies. This can range from missing information and eligibility lapses to coding errors or unmet payer policies. For example, out-of-network claim denial rates can reach as high as 37 percent, according to recent data. Even in-network, nearly one in five claims face denial, leading to a potential 3 to 5 percent revenue loss for providers.
Each denial code points to a root cause, such as incomplete documentation, inaccurate patient details, or outdated insurance information. By deciphering these codes, billing teams can take targeted corrective action, improving workflow and reducing future denials. For healthcare leaders, denial code literacy is essential—it enables data-driven decisions that protect revenue and optimize resource allocation.
Partnering with an experienced RCM service provider can further enhance denial management. For a deeper dive into best practices and real-world strategies, see Denial management in medical billing.
Categories of Denial Codes in Medical Billing
To effectively address the top 20 denial codes in medical billing, it is vital to understand their categories. Grouping denial codes by root cause helps billing teams quickly identify patterns and implement targeted solutions. The main categories include:
| Category | Common Triggers | Example Denial Code |
|---|---|---|
| Eligibility/Coverage | Invalid or expired insurance, missing EOB | CO-27, CO-22 |
| Authorization | Lack of pre-approval for services | CO-197 |
| Coding/Modifiers | Incorrect or mismatched codes, missing modifiers | CO-16, CO-11, CO-97 |
| Timely Filing | Claims submitted after payer deadline | CO-29 |
| Medical Necessity | Insufficient documentation for necessity | CO-50 |
| Duplicate Claims | Multiple submissions for same service | CO-18 |
| Network Issues | Out-of-network services or coverage gaps | CO-45, CO-109 |
Typical triggers for these categories include:
- Eligibility: Failure to verify insurance at each visit.
- Authorization: Missing or outdated pre-certification.
- Coding: Use of outdated or incorrect diagnosis/procedure codes.
- Timely Filing: Internal workflow delays.
- Medical Necessity: Incomplete clinical documentation.
- Duplicates: Submitting both electronic and paper claims.
- Network: Billing out-of-network services at non-contracted rates.
Categorizing denials streamlines root cause analysis and accelerates team response. It also reduces repeat errors and improves cash flow. Competitor analysis reveals that eligibility verification gaps, missing authorizations, and coding mismatches are among the most common sources of denials.
By focusing preventive strategies on each denial category, healthcare organizations can make significant strides in reducing denials and optimizing their revenue cycle.
Top 12 Denial Codes in Medical Billing: Detailed Guide
Understanding the top 20 denial codes in medical billing is essential for healthcare business leaders aiming to strengthen revenue cycle management. By focusing on the most frequent denial codes, organizations can target root causes, streamline workflows, and accelerate cash flow. Below, you will find a unique, data-driven guide to the 12 most impactful denial codes, including practical solutions for each. Mastering these codes can help your team reduce rework, minimize lost revenue, and stay ahead of evolving payer requirements.
To help you visualize the impact, here is a summary table of the top denial codes and their primary triggers:
| Denial Code | Description | Common Trigger | Impact |
|---|---|---|---|
| CO-16 | Missing/Incorrect Information | Incomplete data, missing documents | Delayed payment |
| CO-197 | Authorization Required | No pre-authorization for services | Full denial |
| CO-18 | Duplicate Claim/Service | Resubmission without status check | Increased AR days |
| CO-11 | Diagnosis/Procedure Mismatch | Diagnosis does not justify procedure | Lost revenue |
| CO-29 | Timely Filing Limit Exceeded | Claims submitted after deadline | Irrecoverable loss |
| CO-50 | Medical Necessity Not Established | Insufficient documentation | Appeals workload |
| CO-22 | Coordination of Benefits Missing | Missing primary/secondary info | Delayed payments |
| CO-97 | Service Bundled/Included | Bundling errors, modifier misuse | Reduced reimbursement |
| CO-27 | Patient Coverage Terminated | Insurance inactive on service date | Patient responsibility |
| CO-45 | Charges Exceed Fee Schedule | Billed charges too high | Adjustments needed |
| CO-96 | Non-covered Charges | Service excluded by policy | Write-offs |
| CO-109 | Claim Not Covered by This Payer | Wrong payer billed | Resubmission needed |
By addressing these common issues, your organization can effectively reduce denials and improve the overall financial health of your practice. Let’s dive into each code and how it fits within the top 20 denial codes in medical billing.
![]()
1. CO-16: Missing or Incorrect Information
CO-16 is one of the top 20 denial codes in medical billing, often triggered when essential claim details are missing or inaccurate. This includes incomplete patient demographics, invalid NPI numbers, or missing provider information. For example, a claim may be denied if the referring physician's details are omitted. The financial impact is significant, as denials delay payments and increase administrative rework. To reduce CO-16 denials, implement robust claim audits and data validation protocols before submission. Consistent staff training and EHR-billing integration can further minimize these preventable errors.
2. CO-197: Precertification or Authorization Required
Among the top 20 denial codes in medical billing, CO-197 is frequently encountered when services are provided without obtaining necessary pre-approvals. This code typically applies to high-cost imaging, surgeries, or specialty procedures, such as MRIs performed without prior authorization. The result is a full claim denial, causing frustration for both providers and patients. To address this, strengthen your front-end authorization workflows and leverage real-time tracking. Proactive communication with payers and patients prevents unnecessary denials and keeps revenue flowing.
3. CO-18: Duplicate Claim or Service
CO-18 appears regularly in the top 20 denial codes in medical billing. This denial arises when the payer system detects identical claims or services already processed. Common causes include resubmitting claims without verifying adjudication status or submitting both paper and electronic versions for the same encounter. The impact is increased accounts receivable days and potential payer scrutiny. To avoid CO-18 denials, use claim tracking tools, monitor remittance advices thoroughly, and educate billing teams on correct resubmission practices.
4. CO-11: Diagnosis Inconsistent With Procedure
Another of the top 20 denial codes in medical billing, CO-11, occurs when the diagnosis code does not support the billed procedure under the payer’s policy. For instance, submitting a preventive service with an unrelated diagnosis can trigger this denial. The result is lost revenue and the need for additional clinical documentation review. To prevent CO-11 denials, ensure strong coder-provider communication and verify that diagnosis codes align with the reported procedures. Regular chart audits can also catch discrepancies before submission.
5. CO-29: Timely Filing Limit Exceeded
CO-29 is a critical member of the top 20 denial codes in medical billing, as it results from submitting claims after payer-specific deadlines. Filing limits can range from 90 to 180 days, depending on the insurer. Delays caused by workflow bottlenecks or overlooked claims can make revenue unrecoverable. To reduce CO-29 denials, establish clear submission timelines, automate reminders, and escalate delayed claims promptly. Monitoring workflows closely ensures claims are processed within the allowable window.
6. CO-50: Medical Necessity Not Established
CO-50 is a common entry within the top 20 denial codes in medical billing, triggered when payers determine that a service is not medically necessary based on documentation or diagnosis. For example, billing cosmetic procedures as medically necessary will likely result in denial. The impact includes increased appeals workload and possible compliance risks. Strengthen clinical documentation, ensure diagnosis codes match payer criteria, and educate providers on payer requirements to minimize CO-50 denials and related financial exposure.
7. CO-22: Coordination of Benefits Information Missing
CO-22 is a frequent contributor to the top 20 denial codes in medical billing. It occurs when primary or secondary insurance details are missing or outdated. For example, failing to submit the primary explanation of benefits with a secondary claim leads to delays. This denial can result in delayed or lost payments if not addressed promptly. To prevent CO-22 denials, verify coverage order and update insurance information at every patient encounter. Train front-desk staff on the importance of accurate insurance data capture.
8. CO-97: Service Included in Another Procedure/Bundling
CO-97 stands out in the top 20 denial codes in medical billing due to its link to coding and bundling errors. This denial occurs when services are billed separately but are considered part of a bundled package, such as a post-op visit within a global surgical fee. Modifier misuse is a frequent culprit. Understanding bundling rules and applying correct modifiers is vital. For deeper insights, see Common errors with modifier 59 to avoid unnecessary CO-97 denials.
9. CO-27: Patient Coverage Terminated
CO-27 is a key code among the top 20 denial codes in medical billing, triggered when a patient’s insurance coverage is inactive on the service date. For example, scheduling an appointment after policy termination shifts financial responsibility to the patient or a secondary payer. To reduce CO-27 denials, conduct real-time eligibility checks before every visit. Encourage staff to verify coverage status at scheduling and check-in to avoid surprises and protect your revenue cycle.
10. CO-45: Charges Exceed Fee Schedule/Contractual Allowance
Within the top 20 denial codes in medical billing, CO-45 is prevalent when billed charges exceed the payer’s allowable rates. This often happens with out-of-network services or when charge masters are not updated. The outcome is reduced payments and increased contractual adjustments. To mitigate CO-45 denials, regularly review payer contracts, update your charge master, and educate billing teams on allowable fee schedules. This ensures claims are submitted accurately and revenue is maximized.
11. CO-96: Non-covered Charges
CO-96 is another important code in the top 20 denial codes in medical billing, representing claims for services excluded under a patient’s insurance policy. Examples include experimental treatments or items listed as non-covered benefits. The impact is often write-offs or patient billing. To prevent CO-96 denials, verify coverage policies prior to service delivery and educate staff about non-covered services. Keeping teams informed reduces the risk of avoidable denials and patient dissatisfaction.
12. CO-109: Claim Not Covered by This Payer/Contractor
CO-109 rounds out our top 20 denial codes in medical billing, occurring when a claim is submitted to the wrong payer or a payer not responsible for the patient. For instance, sending a claim to Medicare when the patient has active commercial insurance. The result is payment delays and increased resubmission workload. The solution is to confirm payer responsibility and update insurance records regularly. Empower your team to resolve CO-109 denials quickly and keep cash flow steady.
How to Handle and Prevent Denial Codes
Managing denials efficiently is critical for healthcare organizations aiming to reduce revenue loss and administrative overhead. With the top 20 denial codes in medical billing accounting for a significant share of rejections, having a robust strategy in place is non-negotiable for business success.
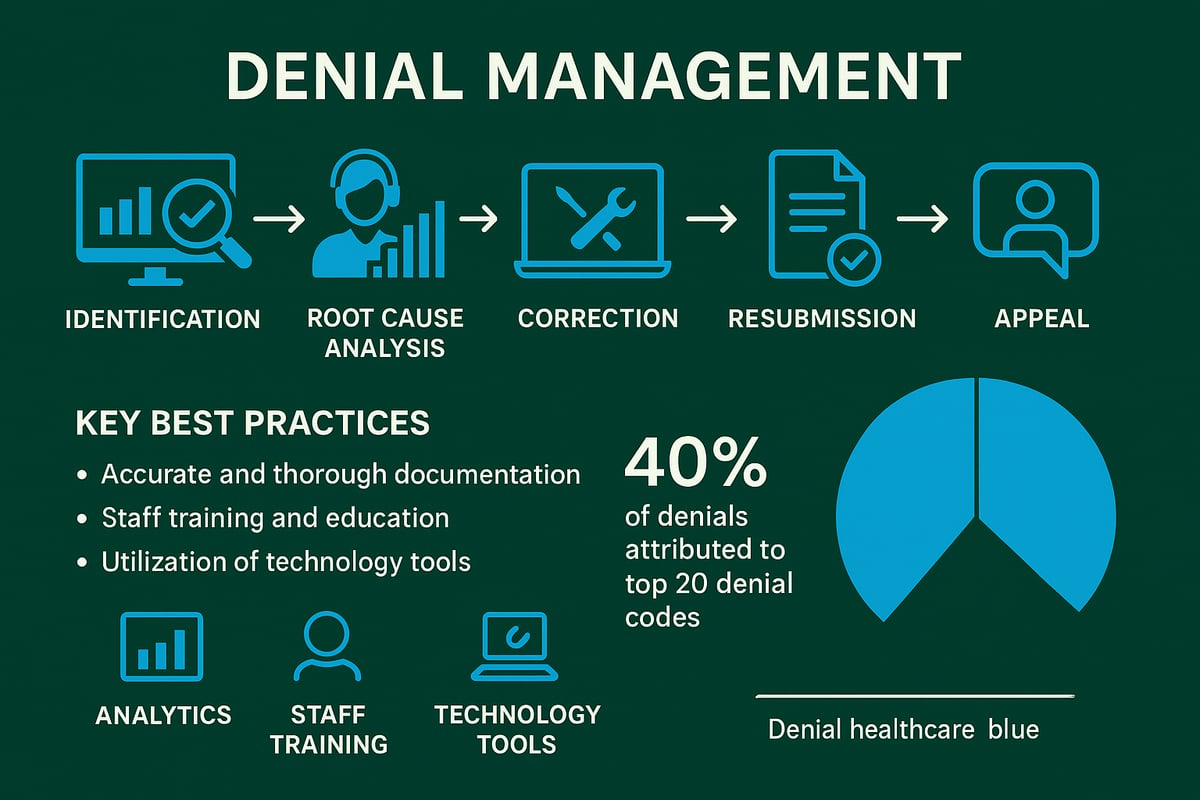
A structured denial management workflow starts with prompt identification of denials as soon as remittance advice is received. Teams should categorize each denial by type, such as eligibility, authorization, or coding, to streamline the resolution process. Assigning denial categories to specialized staff ensures expertise is applied where it matters most, especially for high-frequency issues like the top 20 denial codes in medical billing.
Root cause analysis is essential. By leveraging denial analytics, organizations can uncover patterns and systemic problems behind recurring denials. Regularly reviewing these analytics helps prioritize workflow improvements and targets the most problematic codes. This data-driven approach not only reduces the volume of the top 20 denial codes in medical billing but also supports continuous revenue cycle optimization.
Investing in ongoing staff training is equally important. Billing professionals should receive updates on payer policies, coding guidelines, and documentation standards. This minimizes errors and keeps everyone aligned with industry best practices. Utilizing technology, such as automated eligibility checks and real-time authorization tracking, further reduces manual mistakes and supports accurate claim submission for the top 20 denial codes in medical billing.
Open communication between billing teams and providers is vital. Clarifying documentation or coding questions in real time prevents unnecessary delays. When denials occur, developing standardized appeal templates and a consistent evidence collection process can significantly increase overturn rates. For a deeper dive into effective appeals, consult this resource on how to appeal medical insurance denial.
An example of best practice is integrating EHR and billing systems, which can dramatically reduce CO-16 denials by ensuring claim data is accurate and complete before submission. Proactive denial management not only improves operational efficiency but also has a direct impact on cash flow. To learn more, see this article on how denial management improves cash flow.
By implementing these strategies, healthcare organizations can address the root causes of the top 20 denial codes in medical billing, reduce rework, and maximize reimbursement. Consistent monitoring, training, and collaboration create a culture of accountability and excellence in denial prevention.
Actionable Strategies to Reduce Future Denials
Reducing claim denials requires a proactive, systematic approach. For organizations seeking to minimize the impact of the top 20 denial codes in medical billing, prevention starts at the front end and continues throughout the revenue cycle. Below are proven, actionable strategies designed to help healthcare businesses lower denial rates, accelerate payments, and maintain financial health.
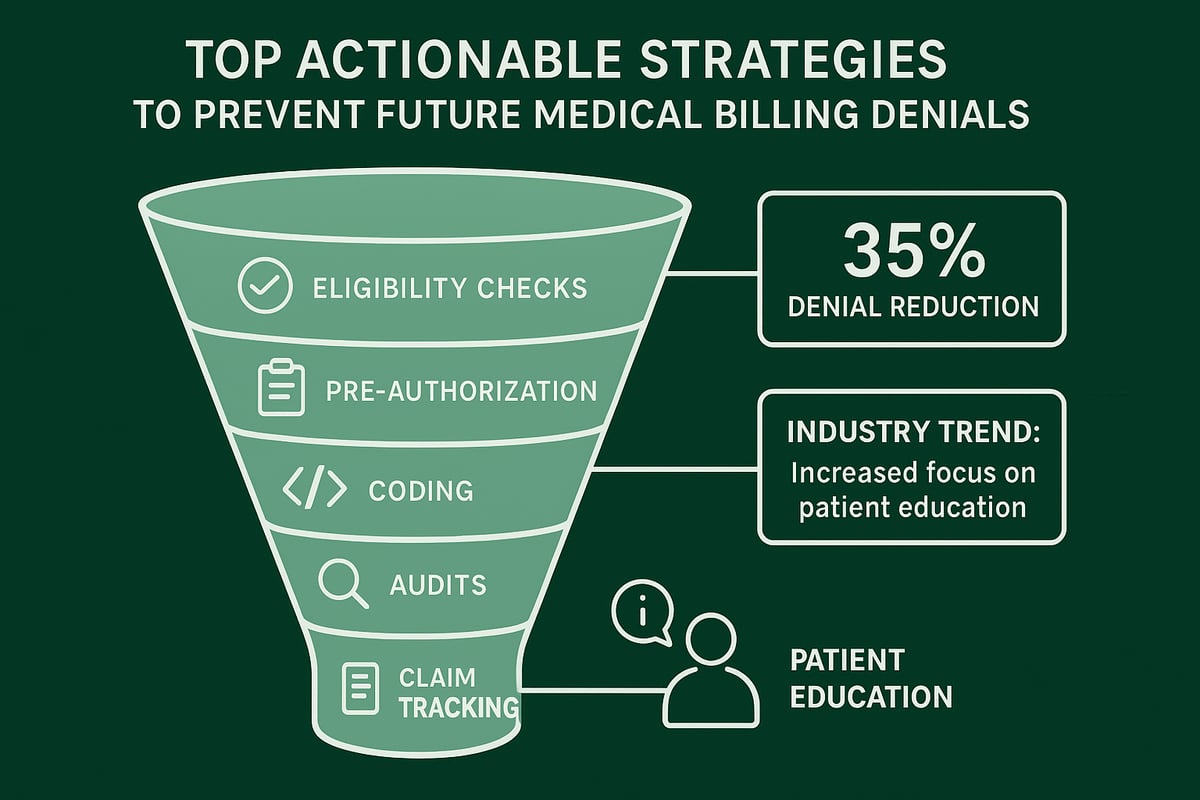
1. Conduct Eligibility and Benefits Verification Before Every Encounter
Verifying patient insurance eligibility and benefits before each visit is the foundation of denial prevention. This step helps catch inactive coverage, outdated information, and plan limitations early, reducing denials related to eligibility and coverage. Practices that perform robust eligibility checks see up to 30 percent fewer eligibility-related denials, a significant improvement when tackling the top 20 denial codes in medical billing.
2. Establish Clear Pre-Authorization Protocols
For services requiring prior approval, implement a standardized pre-authorization workflow. Assign responsibility for checking authorization status, track requests in real time, and document approvals in patient records. Missing or delayed authorizations are a leading cause among the top 20 denial codes in medical billing, especially for specialty care and high-cost procedures.
3. Standardize Charge Entry and Coding Processes
Accurate coding and charge entry are essential. Use standardized templates, cross-check codes with current payer guidelines, and provide ongoing coder education. Common mistakes, such as mismatched diagnosis and procedure codes or missing modifiers, frequently trigger denials. Referencing Top Medical Coding Errors and Audit Trends, coding errors are a consistent driver behind high-volume denials.
4. Regularly Audit Claims for Completeness and Accuracy
Before submitting claims, conduct audits to check for missing information, invalid data, and documentation gaps. Automated claim scrubbing tools can flag errors, but a skilled review by billing professionals adds an extra layer of protection. This approach directly addresses several of the top 20 denial codes in medical billing, including those related to incomplete or incorrect information.
5. Stay Current on Payer Policy Changes and Communicate Updates
Payer policies evolve frequently. Designate a team member to monitor payer communications, update internal protocols, and relay changes to all relevant staff. Keeping everyone informed prevents outdated practices from causing unnecessary denials.
6. Implement Claim Tracking and Avoid Duplications
Use claim tracking systems to monitor submission status, quickly identify rejections, and prevent duplicate filings. Duplicates are a common reason claims appear in the top 20 denial codes in medical billing, often resulting from resubmissions without proper follow-up.
7. Educate Patients About Coverage Limitations and Financial Responsibilities
Transparent communication with patients regarding their benefits and out-of-pocket costs reduces confusion and the likelihood of denied services. Provide written estimates and clarify non-covered services upfront.
8. Leverage Denial Trend Reports for Workflow Improvement
Analyze denial data regularly to identify patterns. Focus on high-frequency denial types, root causes, and recurring process gaps. Industry-wide, practices that use data-driven denial management see measurable improvements in cash flow and administrative efficiency.
9. Foster a Culture of Accountability and Continuous Improvement
Encourage team members to take ownership of their role in the revenue cycle. Set clear performance metrics, provide regular feedback, and celebrate reductions in denial rates. Continuous process improvement is vital for long-term success, especially as the landscape of the top 20 denial codes in medical billing evolves.
10. Measure Impact and Benchmark Against Industry Data
Track key performance indicators such as denial rate, days in accounts receivable, and first-pass resolution rate. Compare your results with national benchmarks. According to Medical Billing Errors Statistics 2025, up to 80 percent of medical bills contain errors, highlighting the importance of robust prevention strategies.
| Strategy | Common Denial Types Impacted | Expected Result |
|---|---|---|
| Eligibility Verification | Eligibility, Coverage Terminated | Fewer eligibility denials |
| Pre-Authorization Protocols | Authorization, Medical Necessity | Reduced auth-related denials |
| Coding Standardization | Coding, Bundling, Non-covered | Fewer coding errors |
| Claim Audits | Missing/Incorrect Info, Timely Filing | Lower rework, faster payment |
| Patient Education | Non-covered, Charges Exceed | Improved patient collections |
By implementing these strategies, healthcare organizations can significantly reduce the frequency and impact of the top 20 denial codes in medical billing. Proactive management not only improves cash flow but also strengthens relationships with payers and patients.
Now that you’ve seen how the top 12 denial codes impact your revenue cycle and learned practical strategies for tackling them, you might be wondering how your current billing processes stack up. At Greenhive Billing Solutions, we believe every healthcare provider deserves clarity and confidence when it comes to claim management. If you’re ready to uncover hidden denial trends and discover opportunities to boost your reimbursements, let’s take the next step together. You can get a clear, actionable picture of your billing performance with a complimentary review—simply Get Your Free Audit.