Medical insurance denials can be a significant source of frustration for healthcare organizations, often resulting in lost revenue and increased administrative workload. Studies show that over 20% of medical claims are initially denied, creating challenges for providers and revenue cycle teams.
If you are looking for clear guidance on how to appeal medical insurance denial, this expert guide is designed for you. We offer proven strategies and insights to help you navigate the appeals process successfully in 2026.
Follow our step-by-step approach to overturn denials and secure the reimbursements your practice deserves. This comprehensive roadmap is tailored specifically for healthcare providers and revenue cycle management professionals, with a focus on B2B needs.
You will find detailed sections on understanding denials, preparing for appeal, the appeal process, documentation best practices, overcoming common challenges, and expert tips to boost your success rate.
Understanding Medical Insurance Denials in 2026
Medical insurance denials continue to challenge healthcare providers in 2026, impacting revenue cycles and operational efficiency. Understanding the evolving landscape is essential for organizations seeking to master how to appeal medical insurance denial and secure timely reimbursements.
Types of Insurance Denials
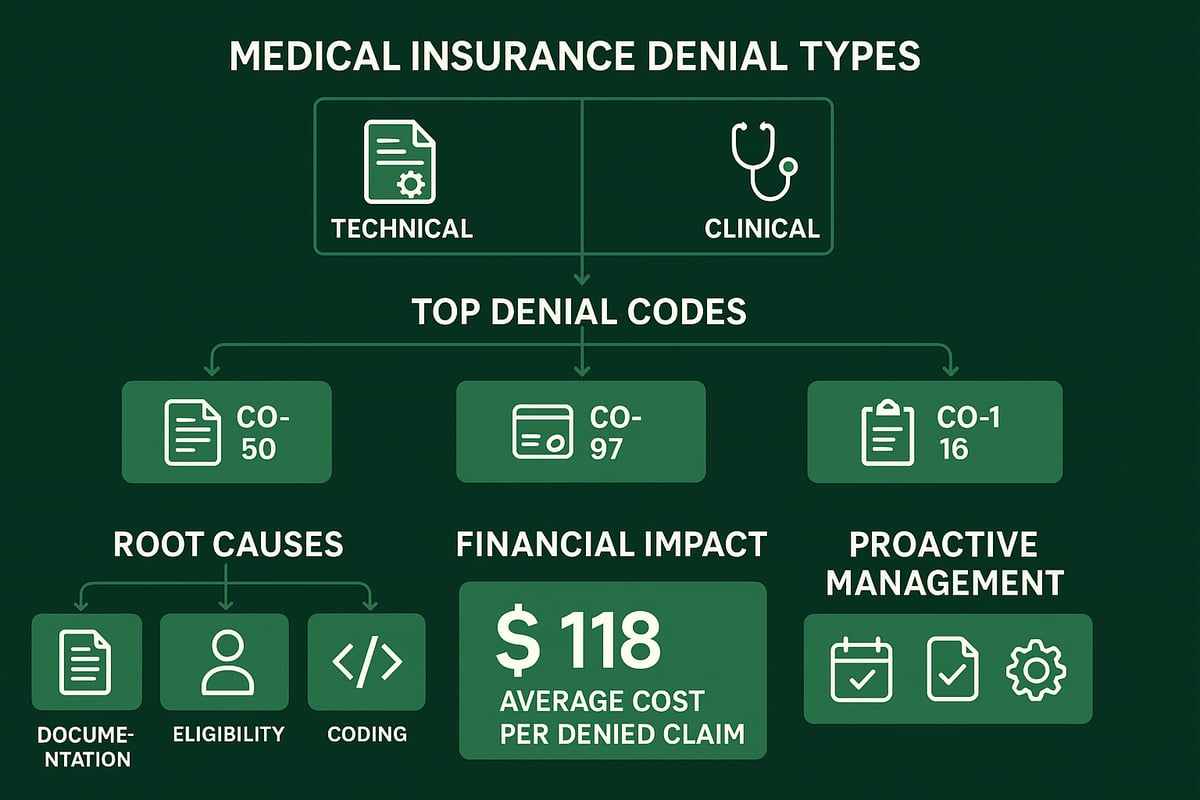
Denials fall into two main categories: technical and clinical. Technical denials stem from missing information, incorrect patient details, or eligibility errors, while clinical denials relate to medical necessity or insufficient documentation. Common denial codes in 2026 include CO-50 (non-covered services), CO-97 (service not consistent with diagnosis), and CO-16 (missing information). For example, claims may be denied due to incomplete prior authorization or incorrect coding. Recent data shows that 15–25% of denials occur because of eligibility errors, directly affecting cash flow. Recognizing these types is the first step in learning how to appeal medical insurance denial effectively.
Root Causes of Denials in Healthcare Practices
The root causes of denials are often preventable. Documentation errors, coding inaccuracies, and lapses in eligibility verification are frequent culprits. Insufficient prior authorization and failure to demonstrate medical necessity are also common. According to Change Healthcare, 86% of denials are potentially avoidable. In 2026, payer policy changes and stricter requirements further increase denial rates. Understanding these underlying reasons is vital when developing strategies for how to appeal medical insurance denial and reduce future occurrences.
The Financial and Operational Impact of Denials
The financial burden of denials is significant. On average, it costs $118 to rework each denied claim, according to MGMA. Delayed reimbursements increase A/R days and disrupt cash flow, while staff must spend additional time managing appeals. This operational strain diverts resources from patient care and other revenue-generating activities. Addressing these impacts is central to any approach focused on how to appeal medical insurance denial and protect organizational profitability.
Regulatory and Payer Policy Changes Affecting Denials
2026 brings new CMS and private payer policies, including increased automation and AI-driven claim reviews. These changes introduce stricter documentation requirements and more frequent audits. Providers must stay current with regulatory updates and adapt workflows accordingly. Failing to comply can result in higher denial rates and greater appeal complexity. Being aware of these changes is critical for organizations learning how to appeal medical insurance denial in a dynamic environment.
Importance of a Proactive Denial Management Strategy
A proactive denial management strategy is essential for sustainable success. By analyzing root causes, training staff, and optimizing workflows, practices can prevent recurring denials. For example, organizations using analytics have reduced denials by 30%. Leveraging denial management in medical billing services helps healthcare providers streamline their processes and improve appeal outcomes. Ultimately, proactive management is the foundation for mastering how to appeal medical insurance denial and maximizing revenue integrity.
Preparing for a Successful Appeal
Preparing effectively is essential for any healthcare organization seeking guidance on how to appeal medical insurance denial. A methodical approach before launching an appeal can make the difference between a denied and an approved claim. Each step below ensures your team is ready to act quickly, accurately, and with the right documentation in hand.
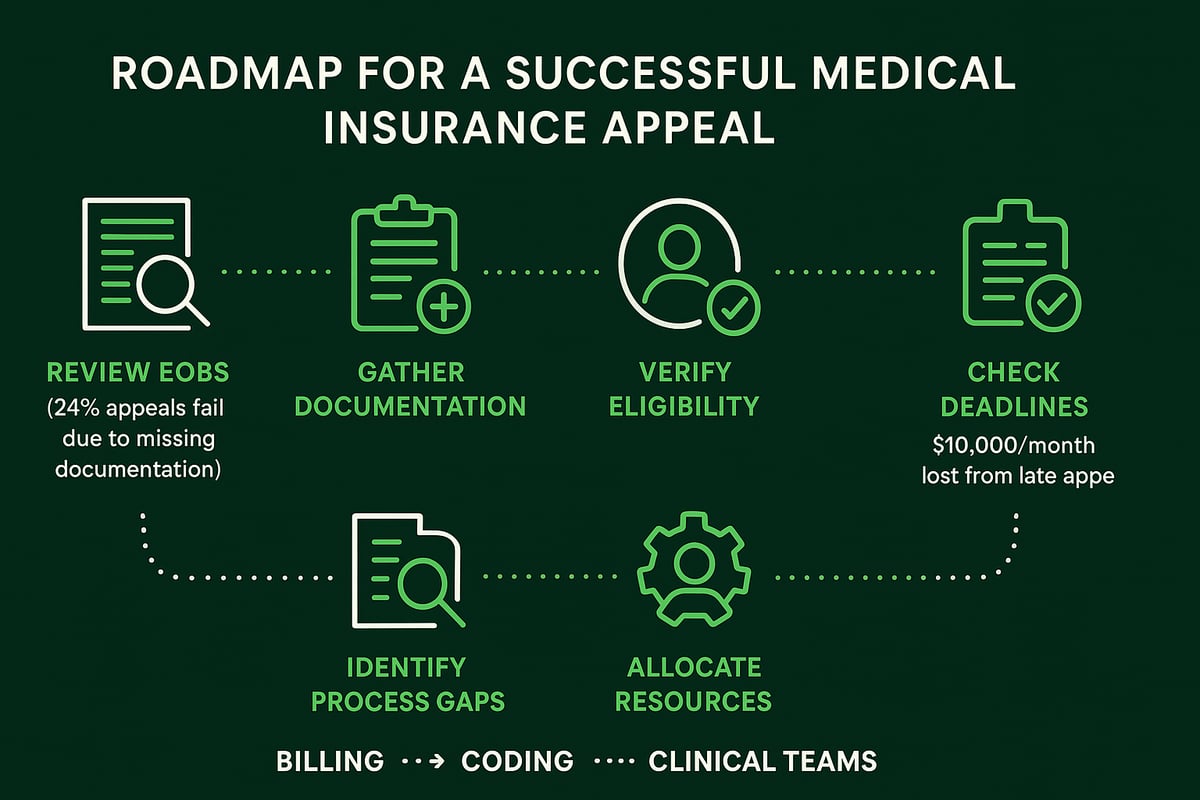
Reviewing the Explanation of Benefits (EOB) and Denial Letter
The first step in how to appeal medical insurance denial is a thorough review of the Explanation of Benefits (EOB) and denial letter. These documents detail why the claim was denied and reference specific denial codes.
Teams should interpret each code carefully. For instance, CO-16 signals missing information, while CO-50 relates to non-covered services. Misreading these can lead to fruitless appeals. For example, confusing a documentation error for a medical necessity issue often results in wasted effort and delayed reimbursement.
A best practice is to create a quick-reference table for the most common denial codes your organization encounters:
| Denial Code | Common Meaning | Next Step |
|---|---|---|
| CO-16 | Missing Information | Submit required documents |
| CO-50 | Not Medically Necessary | Provide supporting records |
| CO-97 | Service Not Covered | Verify plan coverage |
Careful interpretation ensures your appeal addresses the actual denial reason.
Gathering Comprehensive Patient and Claim Documentation
Accurate documentation is the backbone of any successful approach to how to appeal medical insurance denial. Gather all essential records, such as:
- Detailed clinical notes
- Coding sheets
- Prior authorization forms
- Patient insurance cards
- Referral documentation (if required)
Incomplete files are a leading reason for failed appeals. According to Becker’s Hospital Review, 24% of appeals are denied due to missing documentation. Establish a standardized checklist for every appeal to ensure nothing is overlooked.
Collaboration between billing, coding, and clinical staff is vital. A single missing note or coding sheet could undermine your efforts. Regular audits can help maintain compliance and completeness, increasing your appeal success rate.
Verifying Insurance Coverage and Eligibility
Verifying patient eligibility is a critical step in how to appeal medical insurance denial. Double-check coverage at the time of service and before submitting the appeal. Eligibility issues account for up to 25% of denials.
Common pitfalls include outdated insurance data, coverage lapses, or incorrect plan details. Utilize electronic verification tools, and keep a detailed log of all eligibility checks. For guidance, review eligibility verification services to streamline this process and reduce errors.
Create an eligibility checklist for staff:
- Confirm active coverage on date of service
- Verify plan benefits and exclusions
- Document all verification attempts
A proactive approach prevents unnecessary denials and strengthens your appeal position.
Assessing Timely Filing Limits and Appeal Deadlines
Understanding payer deadlines is essential when planning how to appeal medical insurance denial. Most payers set strict timelines—typically 30 to 180 days from the denial date—for submitting appeals.
Missing these deadlines can mean forfeiting reimbursement entirely. Practices have reported losses of up to $10,000 per month due to late appeals. Implement a tracking system to monitor pending deadlines, and assign responsibility for timely submissions.
A sample workflow could include:
- Date stamping all denial letters
- Entering deadlines into a shared calendar
- Setting automated reminders for approaching cutoffs
Timely action preserves your right to appeal and protects your revenue.
Identifying Internal Process Gaps
Every healthcare organization should assess internal workflows to support how to appeal medical insurance denial effectively. Identify common bottlenecks, such as slow information transfer between departments or incomplete denial tracking.
Cross-department collaboration is crucial. Billing, coding, and clinical teams must communicate efficiently to resolve issues quickly. Use denial trend reports to spot recurring problems and develop targeted solutions.
Consider a brief root cause analysis after each denied claim. This helps uncover systemic issues—such as incorrect use of modifiers or incomplete clinical notes—that can be corrected to prevent future denials.
Allocating Resources for Appeal Management
Strategic resource allocation is the final step in preparing for how to appeal medical insurance denial. Assign dedicated staff or a specialized team to manage appeals, ensuring expertise and accountability.
For complex or high-volume denials, consider partnering with experienced revenue cycle management (RCM) professionals. A cost-benefit analysis can help determine if outsourcing appeals is more efficient than handling them internally.
Key options include:
- In-house appeals team
- Cross-trained multi-role staff
- External RCM partners for specialized support
Clear roles and responsibilities, combined with regular performance reviews, ensure your appeal process remains robust and responsive.
Step-by-Step Process to Appeal Medical Insurance Denials
Appealing denied claims is a critical process for healthcare organizations seeking to protect revenue and maintain operational efficiency. Understanding how to appeal medical insurance denial effectively is vital for revenue cycle teams in 2026. Below is a detailed, actionable guide to help your practice overturn denials and secure rightful payments.
![]()
Step 1: Initial Claim Review and Validation
Begin your process by thoroughly reviewing the original claim. Audit all submitted data for completeness, accuracy, and alignment with payer requirements. Common errors, such as mismatched CPT and ICD codes or missing modifiers, are frequent reasons for denial.
Ensure that clinical documentation supports the billed services. If you are learning how to appeal medical insurance denial, validating the coding and supporting documents is a foundational step. For example, missing a required modifier or submitting outdated codes can trigger immediate rejections.
Create a checklist to verify:
- Patient demographics
- Coding accuracy
- Service dates and authorizations
Address discrepancies before moving to the appeal phase.
Step 2: Contacting the Payer for Clarification
Once errors are ruled out, reach out to the payer for clarification. Efficient communication can uncover the specific reason for denial and clarify any ambiguous points in the Explanation of Benefits.
Prepare a list of targeted questions before calling. Document every conversation with payer representatives, including names, dates, and details discussed. This documentation is essential when learning how to appeal medical insurance denial, as it creates a record that may support your case if issues escalate.
If you encounter unresolved issues or unclear denial codes, request escalation to a supervisor or specialist for further guidance.
Step 3: Preparing the Appeal Letter and Supporting Documents
Drafting a compelling appeal letter is central to how to appeal medical insurance denial successfully. Your letter should clearly state patient and claim details, the denial reason, and a concise argument supported by evidence.
Key elements include:
- Patient and provider information
- Original claim details
- Explanation of why the denial should be overturned
- References to medical records, coding guidelines, and payer policies
Customize templates for each payer. Attach all relevant documentation such as clinical notes, authorizations, and coding sheets. A strong, organized submission increases your chances of success.
Step 4: Submitting the Appeal via Correct Channels
Submit your appeal through the payer’s preferred channel, whether electronic or paper. Each payer may have specific submission methods and forms, so following instructions precisely is essential.
Track every submission and obtain confirmation receipts. This step in how to appeal medical insurance denial is often overlooked, leading to lost appeals. Refer to Internal appeals process guidelines for a detailed overview of required steps and timelines.
Avoid common errors such as missing attachments or incomplete forms. Use tracking systems or logs to ensure all appeals are accounted for and can be followed up efficiently.
Step 5: Following Up and Monitoring Appeal Status
After submission, set reminders to follow up within the payer’s specified timeframe. Regular monitoring through payer portals or revenue cycle dashboards ensures you stay informed about the status of each appeal.
If you do not receive a timely response, escalate the issue according to payer protocols. Keeping a structured follow-up schedule is a key component of how to appeal medical insurance denial with higher success rates.
Document all updates, correspondence, and outcomes for every appeal. This practice not only aids in current appeals but also helps refine your future processes.
Step 6: Responding to Additional Information Requests
Payers may request supplemental documentation to process your appeal. Respond promptly and coordinate with clinical staff to gather all necessary records.
Timely, accurate responses demonstrate diligence and professionalism. Delayed or incomplete submissions can result in outright rejection, so this step is crucial in the overall strategy of how to appeal medical insurance denial.
A real-world example: a practice submitted additional physician notes within the required window, leading to a favorable overturn of the denial. Always verify payer timelines for supplemental requests.
Step 7: Documenting Outcomes and Updating Internal Processes
Finally, record the outcome of each appeal, whether successful or not. Analyze trends in overturned or upheld denials to identify root causes and areas for improvement.
Integrate lessons learned into your denial prevention strategy. Sharing knowledge across billing, coding, and clinical teams ensures everyone understands how to appeal medical insurance denial more effectively in the future.
Regularly update internal workflows, train staff on new payer requirements, and use denial analytics to drive continuous process improvement.
Best Practices for Documentation and Compliance
Robust documentation and compliance practices are at the heart of mastering how to appeal medical insurance denial. Healthcare organizations that prioritize accuracy, audit readiness, and data security can significantly reduce denial rates and increase appeal success. Let us break down the essential best practices every revenue cycle team should follow in 2026.
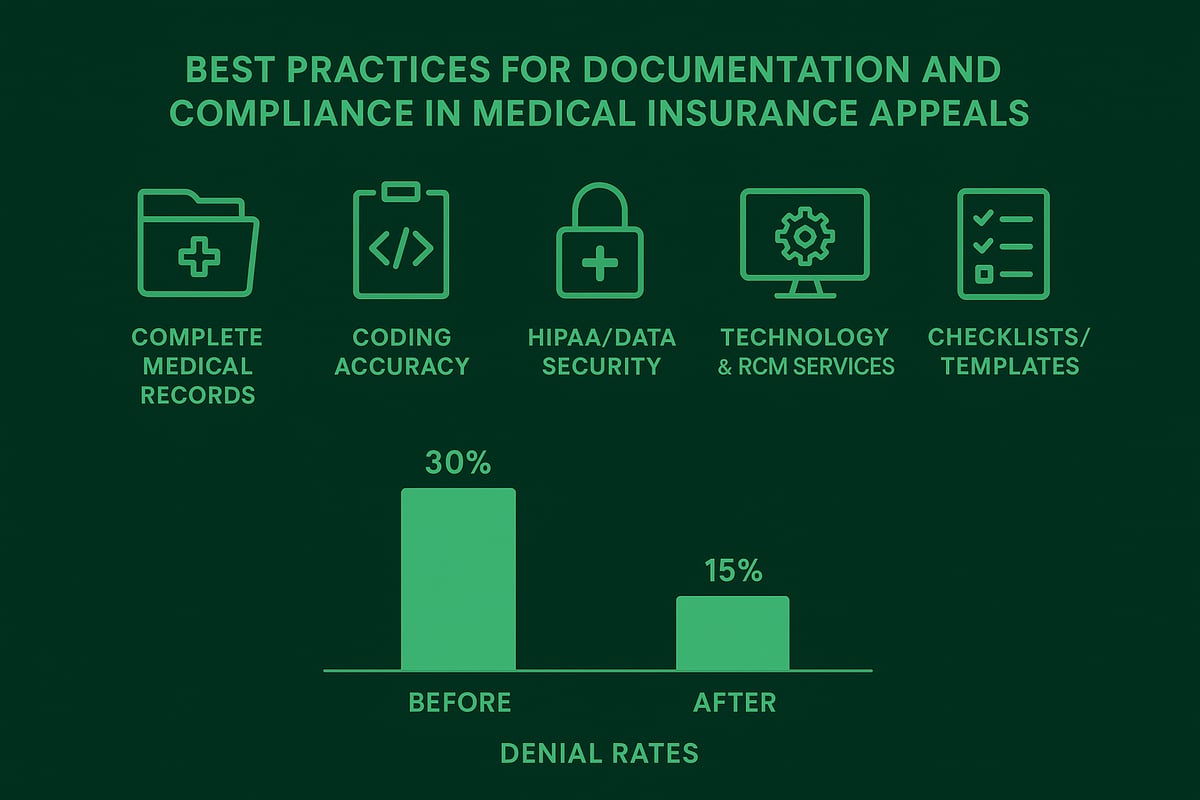
Ensuring Complete and Accurate Medical Records
Complete and accurate medical records are fundamental when learning how to appeal medical insurance denial. Missing or vague documentation is a leading cause of denied claims and failed appeals.
Key components of thorough medical records:
- Detailed clinical notes supporting the billed services
- Clear signatures and dates for all encounters
- Inclusion of prior authorization and referral documents
For example, a denial was overturned after a physician added specific notes clarifying medical necessity, demonstrating the power of precise documentation.
Coding Accuracy and Audit Readiness
Coding errors can undermine your efforts on how to appeal medical insurance denial. Staying current with ICD-10, CPT, and HCPCS code updates is essential. Internal audits help teams catch and correct errors before submission.
Common coding pitfalls include:
- Use of outdated or incorrect codes
- Mismatched CPT and ICD codes
- Misuse of modifiers, such as modifier 59
For a deeper understanding, review common errors with modifier 59 to avoid preventable denials and strengthen your appeal process.
HIPAA and Data Security Considerations
When addressing how to appeal medical insurance denial, compliance with HIPAA and data security standards is non-negotiable. Protecting patient data throughout the appeal process is critical for avoiding regulatory penalties.
Best practices include:
- Using secure, encrypted channels for document transmission
- Limiting access to sensitive information
- Regularly updating policies to reflect evolving regulations
A single data breach can compromise appeal efforts and damage organizational reputation.
Leveraging Technology and RCM Services
Leveraging technology and professional RCM services streamlines how to appeal medical insurance denial. Industry-standard RCM tools accelerate documentation gathering, submission, and tracking. B2B RCM partners bring expertise, reducing denial turnaround time by up to 40 percent for many practices.
Consider the benefits of outsourcing complex appeals:
- Access to experienced professionals familiar with payer requirements
- Seamless integration with client-owned software
- Greater focus on core clinical operations
This approach allows healthcare organizations to optimize resources and enhance compliance.
Documentation Checklists and Templates
Standardized checklists and templates are vital for teams learning how to appeal medical insurance denial. By using these tools, organizations reduce errors and omissions, ensuring each appeal is comprehensive.
Key items to include:
- Appeal letter templates tailored to payer requirements
- Itemized documentation checklists for each claim type
- Shared resources for consistent team-wide practices
Consistent use of checklists leads to fewer missed elements and higher appeal success rates.
Overcoming Common Challenges in the Appeal Process
Overcoming obstacles in the medical insurance denial appeal process is a top priority for healthcare providers. Mastering how to appeal medical insurance denial requires a proactive and strategic approach. Below, we address the most common challenges revenue cycle teams face and share solutions to boost your appeal success rates.
Dealing with High-Volume Denials
The surge in claim denials has created a significant challenge for healthcare organizations. According to recent data, the rate of initial denials of medical insurance claims continued to rise in 2024, leading to increased workloads and delayed revenue. To master how to appeal medical insurance denial in these conditions, prioritize claims by dollar amount and deadline.
Utilize automation tools to identify batch denial trends and process bulk appeals efficiently. Establish a triage system to ensure high-value claims receive prompt attention. Regularly review denial analytics to prevent backlog accumulation.
Navigating Complex Payer Requirements
Every payer has unique policies, documentation standards, and appeal forms. Understanding how to appeal medical insurance denial means staying current with payer-specific rules and updating internal reference guides regularly.
Develop a centralized resource for payer guidelines accessible to all staff. Train teams to interpret policy nuances and submit compliant appeals. Use checklists to confirm all required documents are included, minimizing rework due to incomplete submissions.
Complex requirements often cause confusion. Encourage staff to attend payer webinars and maintain open communication with payer representatives to clarify evolving standards.
Managing Limited Internal Resources
Staffing constraints can slow down the appeal process and lead to missed opportunities. Knowing how to appeal medical insurance denial efficiently involves cross-training teams so multiple staff members can handle appeals during peak periods.
Consider partnering with experienced RCM service providers for support on complex or high-volume cases. Evaluate the cost-benefit of outsourcing versus internal processing. Use process mapping to identify bottlenecks and streamline workflows, ensuring appeals are prepared and submitted within required timelines.
Documented procedures and clear role assignments help prevent gaps and maintain continuity during staff transitions.
Handling Repeated or Recurring Denials
Recurring denials signal underlying issues that need immediate attention. Addressing how to appeal medical insurance denial for persistent problems requires thorough root cause analysis.
Track denial types and frequencies, then implement corrective action plans for the most common issues such as eligibility errors or missing prior authorizations. Involve clinical, billing, and coding teams in regular reviews to share insights and solutions. Adjust workflows and staff training based on denial trends.
For example, clinics have reduced recurring eligibility denials by 50% after revising verification processes and enhancing staff education.
Tracking and Measuring Appeal Success Rates
Continuous improvement depends on tracking key performance indicators (KPIs) like overturn rates, appeal turnaround times, and denial reduction percentages. Benchmark your results against industry standards and leverage strategic denial management best practices to refine your approach.
Implement RCM dashboards to monitor real-time progress and generate actionable reports. Share performance data with stakeholders to foster accountability and encourage a culture of excellence. Use data-driven insights to adjust strategies and maintain a competitive edge in denial management.
Expert Tips and Strategies for Higher Appeal Success Rates
Achieving a high rate of successful appeals is essential for healthcare organizations aiming to optimize revenue and reduce administrative burden. To master how to appeal medical insurance denial, your team needs proven, practical strategies. The following expert tips, tailored for B2B healthcare providers, will help you navigate payer complexities, build stronger processes, and improve outcomes.
Customizing Appeals for Different Payers
Understanding payer-specific requirements is central to how to appeal medical insurance denial effectively. Medicare, Medicaid, and commercial insurers each have unique documentation standards and communication preferences.
Customize each appeal by:
- Reviewing the payer’s latest guidelines
- Adjusting language and evidence to address payer criteria
- Including prior authorization details when relevant (Authorization in medical billing)
Even minor differences in payer rules can determine whether an appeal is approved or denied, so always tailor your submission.
Building Collaborative Appeal Teams
A multidisciplinary approach is vital when considering how to appeal medical insurance denial. Involve billing, coding, and clinical staff from the outset.
Benefits of collaborative teams:
- More comprehensive documentation
- Accurate coding validation
- Stronger clinical justifications
Hold regular cross-department meetings to review appeal outcomes and share lessons learned. This approach fosters accountability and speeds up resolution times.
Continuous Staff Training and Education
Keeping your staff trained is a cornerstone of how to appeal medical insurance denial with success. Payer policies, coding standards, and regulatory requirements evolve rapidly.
Implement these strategies:
- Schedule ongoing workshops and webinars
- Distribute policy updates and cheat sheets
- Encourage certification in medical billing and coding
Well-trained teams reduce errors and improve first-pass appeal rates, leading to fewer lost reimbursements.
Leveraging Data Analytics for Denial Trends
Data-driven insights reveal patterns in claim denials and help refine how to appeal medical insurance denial. Use RCM dashboards and denial analytics to identify root causes and recurring issues.
Key actions include:
- Monitoring KPIs such as overturn rates and appeal timeliness
- Segmenting denials by payer, service type, and denial code
- Benchmarking against industry data (Claims Denials and Appeals in ACA Marketplace Plans in 2023)
This information enables targeted improvements, reducing future denials and increasing appeal efficiency.
Staying Updated on Regulatory and Industry Changes
To stay ahead with how to appeal medical insurance denial, monitor CMS, state, and private payer updates. Regulatory changes can shift appeal deadlines, documentation needs, or submission formats.
Recommended practices:
- Subscribe to industry newsletters
- Assign a compliance lead to track policy changes
- Update internal protocols promptly
Proactive adaptation ensures your organization remains compliant and competitive in a changing landscape.
Utilizing Professional RCM Services for Complex Appeals
Complex or high-value denials often require advanced expertise in how to appeal medical insurance denial. Consider partnering with professional RCM services for these cases.
Advantages include:
- Access to seasoned appeal specialists
- Faster resolution of challenging cases
- 25% higher overturn rates for outsourced appeals
Outsourcing enables your internal team to focus on patient care and routine billing while experts manage intricate appeals and maximize financial recovery.
Navigating medical insurance denials can feel overwhelming, especially with evolving regulations and tighter documentation requirements in 2026. But with the right strategies, clear processes, and expert insights, you can turn denials into opportunities for improved reimbursement and operational efficiency. If you’re ready to take control of your revenue cycle, address recurring challenges, or simply want to ensure your appeals process is as effective as possible, let’s connect. We can review your unique situation and discuss tailored solutions for your practice.
Book Your Free Consultation
Together, we’ll help you secure the reimbursements your organization deserves.