Healthcare revenue cycle billing is more complex than ever, directly impacting the financial health and stability of organizations across the industry. With the revenue cycle billing market projected to exceed $238 billion by 2030, effective management is critical for healthcare providers seeking to improve collections and reduce costly denials. This guide delivers practical strategies that help optimize every stage of revenue cycle billing, ensuring faster reimbursements, fewer errors, and consistent cash flow. You will discover essential RCM components, a step-by-step workflow, proven best practices, technology insights, solutions to common challenges, and expert advice to maximize your revenue potential.
Understanding the Revenue Cycle Billing Process
Revenue cycle billing is the backbone of financial operations for any healthcare organization. As the healthcare industry grows more complex, mastering this process is essential for maintaining financial stability, reducing denials, and ensuring timely reimbursements.
Defining Revenue Cycle Management (RCM) and Billing
Revenue cycle billing refers to the end-to-end financial process that begins with patient scheduling and ends with the final payment received by the provider. While medical billing focuses on claim submission and payment posting, comprehensive RCM encompasses every interaction and transaction from the first point of contact to collections and reporting.
RCM integrates billing into broader financial workflows, ensuring that each step supports accurate reimbursement and compliance. The distinction is crucial: medical billing is a component, but true revenue cycle billing covers the entire financial journey. According to industry projections, the RCM market is expected to surpass $238 billion by 2030, underlining its growing importance for healthcare organizations. For a more detailed look at how this process operates, see the Revenue Cycle Medical Billing Overview.
Poorly managed revenue cycle billing can result in increased claim denials, payment delays, and cash flow disruptions. These issues can jeopardize a provider’s ability to deliver high-quality care and maintain operational efficiency.
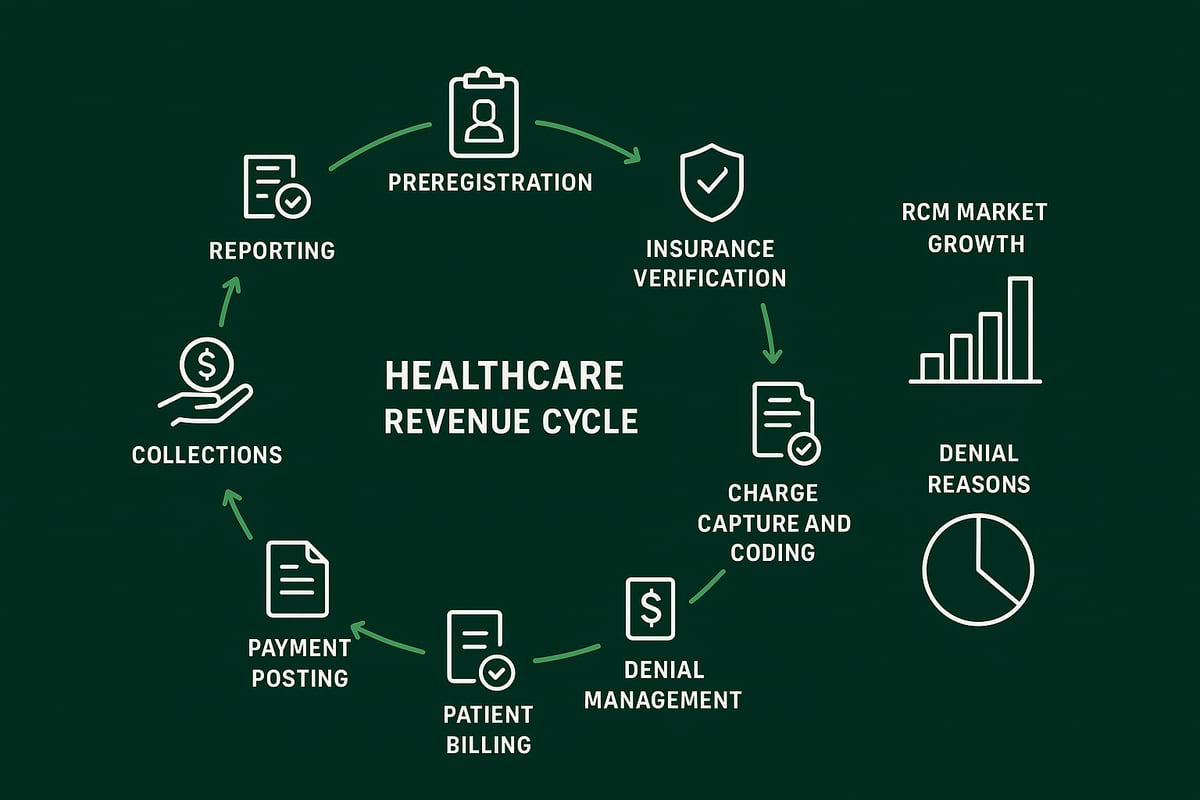
Key Stages of the Healthcare Revenue Cycle
The revenue cycle billing process consists of several interconnected stages, each with its own set of best practices:
- Preregistration: Collect patient demographics and insurance details before the visit.
- Patient Registration: Confirm and update all patient information for accuracy.
- Insurance Verification and Preauthorization: Check eligibility and obtain approvals for specific procedures.
- Charge Capture and Coding: Record all billable services and apply precise ICD-10 and CPT codes.
- Claim Submission: File claims electronically, ensuring compliance and timeliness.
- Denial Management: Track denials, resolve them quickly, and appeal when necessary.
- Payment Posting and Patient Billing: Reconcile payments and send clear statements to patients.
- Collections and Reporting: Follow up on outstanding balances and analyze performance through key metrics.
By following these steps, revenue cycle billing professionals can minimize errors, speed up reimbursements, and enhance overall cash flow. Each stage builds on the previous one, making accuracy and attention to detail critical throughout the cycle.
The Financial Impact of RCM on Healthcare Organizations
Efficient revenue cycle billing directly influences a healthcare organization’s financial health and operational success. When processes are optimized, providers experience:
- Faster reimbursements, which improve cash flow and enable timely investments.
- Lower denial rates, reducing costly rework and administrative burden.
- Greater patient satisfaction, as billing is clear and transparent.
Automated workflows and real-time data validation play a significant role in accelerating payments and reducing manual intervention. For example, organizations using automated systems see fewer errors and can resolve denials more effectively.
A well-managed revenue cycle billing process not only drives profitability, it also supports sustainable growth and a positive patient experience. As the industry continues to evolve, investing in robust RCM practices is essential for long-term success.
Step-by-Step Guide to Revenue Cycle Billing Workflow
Navigating the revenue cycle billing workflow is essential for healthcare organizations aiming for financial stability and operational efficiency. Each stage in the workflow builds on the previous one, so precision and proactive management are critical. Let’s break down each step and explore actionable best practices to optimize your revenue cycle billing process.
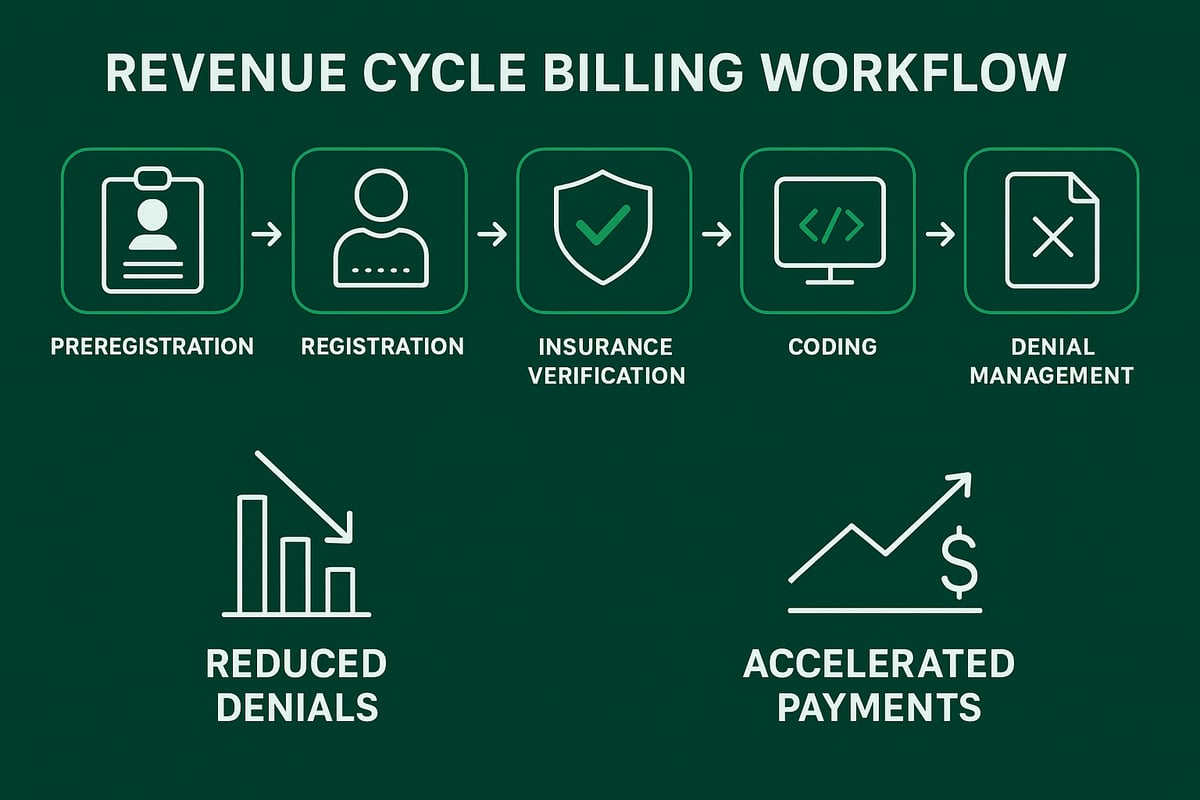
Step 1: Patient Preregistration and Registration
The first step in revenue cycle billing is accurate patient preregistration and registration. Collecting detailed demographic and insurance data upfront minimizes errors that often result in claim denials.
Best practices include:
- Using digital forms to capture patient details before the visit.
- Verifying insurance information at every encounter.
- Validating data in real time to catch discrepancies.
A streamlined preregistration process reduces administrative back-and-forth, improves patient experience, and sets a strong foundation for the entire revenue cycle billing workflow.
Step 2: Insurance Eligibility Verification and Preauthorization
Verifying insurance eligibility and securing preauthorizations are vital for successful revenue cycle billing. Real-time checks confirm the patient’s coverage, reducing the chance of rejected claims.
Key steps to follow:
- Use electronic verification tools for immediate results.
- Obtain preauthorizations for high-cost services.
- Clarify patient financial responsibility upfront.
By establishing coverage and authorization early, practices can prevent delays and improve their revenue cycle billing outcomes, while also enhancing patient satisfaction.
Step 3: Coding and Charge Capture
Accurate coding and charge capture play a pivotal role in revenue cycle billing. Certified coders ensure the correct use of ICD-10 and CPT codes, which impacts both compliance and reimbursement.
Best practices:
- Invest in ongoing coder education and training.
- Use technology to support precise code selection.
- Perform regular internal audits for quality assurance.
For a deeper understanding of the coding process in revenue cycle billing, explore Medical Coding and Revenue Cycle Management. A robust coding strategy reduces denials and supports optimal revenue capture.
Step 4: Claim Submission and Scrubbing
Timely and accurate claim submission is a cornerstone of revenue cycle billing. Automated claim scrubbing tools detect and correct errors before claims reach payers.
Best practices include:
- Submitting claims electronically for faster processing.
- Utilizing claim scrubbing to minimize errors.
- Monitoring claim status to address issues promptly.
Practices that implement claim scrubbing as part of their revenue cycle billing workflow experience fewer denials and accelerated payment cycles.
Step 5: Denial Management and Payment Posting
Effective denial management and payment posting are essential to maintaining healthy revenue cycle billing. Monitor claim status closely and address denials quickly to recover lost revenue.
Key strategies:
- Track denial reasons and adjust processes to prevent recurrence.
- Implement a structured appeal process.
- Ensure accurate payment posting for financial transparency.
A proactive approach to denial management ensures steady cash flow and clear financial reporting throughout the revenue cycle billing process.
Step 6: Patient Billing and Collections
Clear patient billing and collections complete the revenue cycle billing workflow. Transparent statements and flexible payment options encourage timely patient payments.
Best practices:
- Provide easy-to-understand billing statements.
- Offer multiple payment methods and payment plans.
- Follow up on outstanding balances with empathy and professionalism.
A patient-centered approach in the final stage of revenue cycle billing increases collection rates and builds long-term trust with your patient community.
Best Practices for Optimizing Revenue Cycle Billing
Optimizing revenue cycle billing requires a disciplined, strategic approach to every stage of the process. Healthcare organizations that excel in this area combine robust data management, clear communication, and ongoing performance monitoring. Let’s explore essential best practices to drive stronger financial outcomes and operational efficiency for your practice.
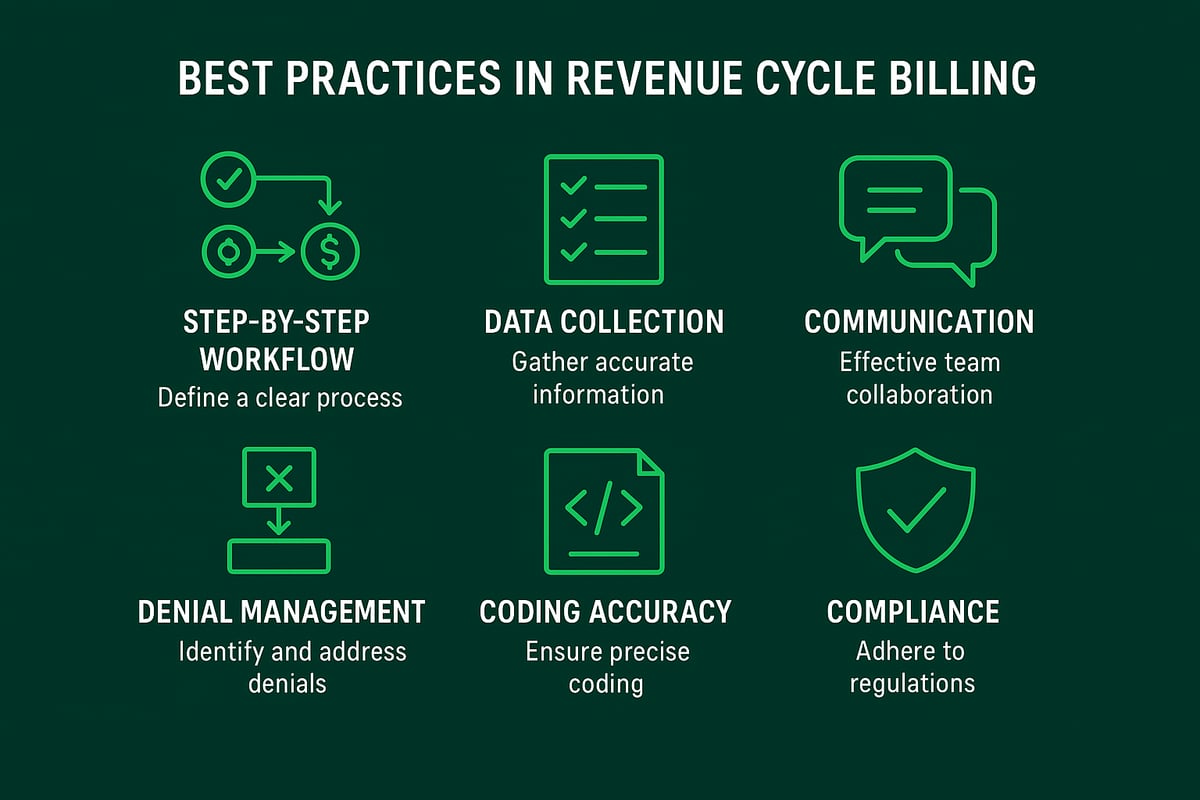
Comprehensive Data Collection and Verification
Accurate data collection is the backbone of effective revenue cycle billing. Every patient encounter must begin with capturing detailed demographic and insurance information. Digital intake forms and real-time validation tools can reduce manual errors and accelerate registration.
- Regularly update patient records at each visit
- Leverage secure digital platforms for data entry
- Validate insurance details before service
When practices prioritize comprehensive data verification, downstream claim denials and payment delays are significantly minimized.
Transparent Patient Communication
Clear, early communication with patients about their financial responsibilities is a game changer for revenue cycle billing. Providing cost estimates and outlining payment expectations before services are rendered builds trust and improves collections.
- Share upfront estimates for procedures
- Explain billing processes in simple terms
- Offer multiple channels for patient inquiries
Practices that invest in transparent communication report higher patient satisfaction and better collection rates.
Proactive Denial Prevention and Management
Denials can disrupt cash flow and require significant resources to resolve. Proactive management begins with analyzing denial trends and addressing root causes. Training staff on common denial triggers and using systematic tracking tools are vital steps.
- Monitor top denial reasons regularly
- Implement real-time pre-submission checks
- Establish a structured appeal process
For an in-depth look at industry strategies, explore Denial Management in Medical Billing to further strengthen your revenue cycle billing approach.
Accurate and Compliant Medical Coding
Precision in coding is essential for compliant, optimized revenue cycle billing. Certified coders must stay current with ICD-10, CPT, and payer-specific guidelines. Ongoing education and technology-assisted code selection reduce costly errors.
- Schedule regular coder training sessions
- Use audit tools to review code accuracy
- Address discrepancies through feedback loops
Accurate coding not only ensures reimbursement but also protects against compliance risks.
Performance Monitoring and Reporting
Continuous performance tracking is fundamental for sustainable revenue cycle billing. Key performance indicators (KPIs) such as days in accounts receivable, denial rates, and net collection rates provide actionable insights.
| KPI | Target Benchmark | Why It Matters |
|---|---|---|
| Days in A/R | < 40 days | Indicates payment speed |
| Denial Rate | < 5% | Reflects claim quality |
| Clean Claim Rate | > 90% | Shows process efficiency |
| Net Collection Rate | > 95% | Measures actual recovery |
Dashboards and analytics platforms enable real-time monitoring, supporting data-driven decision-making for your team.
Regulatory Compliance and Data Security
Compliance with HIPAA and related regulations is non-negotiable in revenue cycle billing. Regular staff training and secure handling of patient data protect your organization from financial penalties and reputational damage.
- Conduct routine compliance audits
- Encrypt all electronic health information
- Update policies as regulations evolve
A strong compliance culture not only safeguards data but also gives peace of mind to both providers and patients.
Greenhive Billing Solutions: Your RCM Partner
Greenhive Billing Solutions delivers tailored revenue cycle billing services to healthcare organizations seeking reliable results. Our certified professionals handle insurance verification, coding, claim submission, denial management, payment posting, and analytics while working seamlessly with your existing systems.
We emphasize HIPAA compliance, transparent reporting, and specialty expertise. Practices partnering with Greenhive see up to 30 percent cost savings and measurable improvements in claim acceptance. Request a free practice audit to identify new opportunities for revenue cycle billing optimization today.
Leveraging Technology and Professional Services in RCM
The landscape of revenue cycle billing is rapidly evolving as healthcare organizations embrace new technologies and professional services. Efficient use of tools and expert support can transform financial operations, drive down costs, and increase collections. For optimal results, healthcare providers need strategies that integrate automation, analytics, security, and flexible service models.
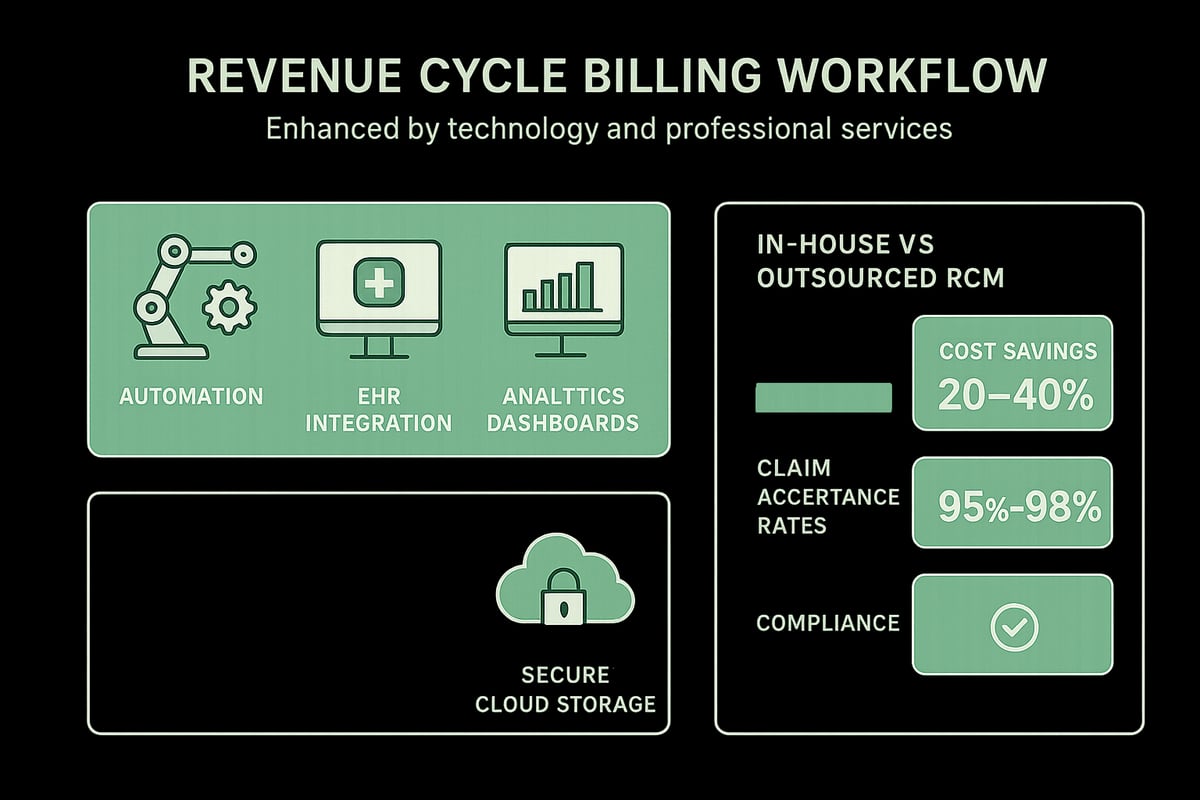
Role of Technology in Revenue Cycle Billing
Technology is pivotal in streamlining revenue cycle billing. Automation tools handle repetitive tasks like claim submission, eligibility verification, and payment posting, resulting in fewer errors and accelerated payments. Integration with EHR and practice management systems ensures that patient data flows seamlessly between clinical and billing teams.
Analytics platforms deliver real-time KPI tracking, making it easier for providers to monitor financial performance and identify bottlenecks. For example, organizations using automated claims processing often see reduced administrative workload and faster reimbursements. To learn more about how analytics can transform your financial outcomes, explore Healthcare Revenue Cycle Analytics.
The adoption of these solutions not only improves accuracy but also gives healthcare professionals the insights needed to make informed decisions and optimize collections.
Outsourcing RCM: Benefits and Considerations
Many healthcare organizations are choosing to outsource revenue cycle billing to specialized partners. Outsourcing can lead to significant cost savings, often reducing billing expenses by up to 30 percent compared to maintaining in-house teams. It also gives access to certified experts who stay updated on the latest regulations and payer requirements.
Professional RCM services offer scalability, adapting to the needs of practices of all sizes and specialties. When evaluating a partner, look for transparent pricing, proven results, and a strong track record in HIPAA compliance.
| In-House Billing | Outsourced RCM |
|---|---|
| Higher staffing costs | Lower overhead |
| Requires ongoing training | Access to certified experts |
| Limited scalability | Flexible service levels |
| Greater risk of errors | Proven processes and quality checks |
Outsourcing enables providers to focus on patient care while experts handle the complexities of revenue cycle billing.
Adapting to Client-Owned Systems
A key advantage of professional RCM services is the ability to work within client-owned software and established workflows. Skilled teams adapt to various EHR and practice management platforms, ensuring a seamless transition and minimal disruption to daily operations.
This flexibility means that healthcare organizations retain full control over their data and systems while leveraging external expertise for improved financial outcomes. Practices benefit from tailored solutions that fit their unique needs, from specialty coding to custom reporting.
By choosing a partner that adapts to your existing setup, you can enhance revenue cycle billing without the need for major system changes.
Security and Compliance in Technology Adoption
Security and regulatory compliance are non-negotiable in revenue cycle billing. All tools and platforms must meet industry security standards to protect sensitive patient data. Regular audits and encrypted data transfer processes are essential for maintaining privacy and demonstrating compliance with HIPAA and other regulations.
Staff training on compliance best practices further reduces risk and ensures adherence to evolving guidelines. When adopting new technologies or professional services, prioritize vendors with a proven commitment to security and regulatory excellence.
A secure, compliant approach safeguards your organization’s reputation and financial health while supporting efficient, accurate revenue cycle billing.
Overcoming Common Challenges in Revenue Cycle Billing
Healthcare organizations face a range of obstacles in revenue cycle billing that can quickly impact financial performance. Addressing these challenges is essential for maintaining a steady cash flow and supporting operational growth. Let’s explore the most common hurdles and proven solutions.
Reducing Claim Denials and Rejections
Claim denials are a persistent challenge in revenue cycle billing, often stemming from incomplete data, eligibility issues, or coding errors. To reduce denials:
- Implement real-time eligibility verification tools.
- Use automated claim scrubbing to catch errors before submission.
- Train staff on the latest coding standards.
For example, practices using automated scrubbing tools have seen a noticeable drop in denial rates and faster payment cycles. Leveraging AI Adoption in RCM can further streamline denial prevention by flagging high-risk claims before they reach payers.
Managing Regulatory Changes and Payer Requirements
The regulatory environment for revenue cycle billing is constantly evolving. Staying up to date with payer guidelines and coding updates is critical to avoiding compliance penalties and payment delays.
- Schedule regular training sessions for billing staff.
- Monitor payer bulletins for policy changes.
- Update internal processes promptly when regulations shift.
By proactively managing compliance, organizations can protect revenue and reduce risk. Staff who are well-informed respond faster to market changes, ensuring claims stay compliant.
Improving Patient Collections and Financial Experience
Patient responsibility continues to grow, making collections a key focus in revenue cycle billing. Improving the patient financial experience requires:
- Offering multiple payment channels, including online options.
- Providing clear, itemized billing statements.
- Setting up payment plans for larger balances.
Effective communication boosts patient satisfaction and increases the likelihood of full payment. Transparent billing builds trust and encourages prompt resolution of outstanding balances.
Addressing Staffing and Training Gaps
Staffing shortages and skill gaps can disrupt revenue cycle billing workflows. Investing in ongoing training and professional development is essential.
- Cross-train team members to cover critical functions.
- Bring in external RCM experts to address complex cases.
- Use mentorship programs to accelerate staff learning.
A well-trained team minimizes errors and adapts quickly to industry changes, supporting consistent billing performance.
Monitoring and Responding to Performance Metrics
Continuous monitoring of revenue cycle billing performance is vital for improvement. Key metrics include:
| Metric | Description |
|---|---|
| Days in A/R | Average time to collect payments |
| Denial Rate | Percentage of claims denied |
| Clean Claim Rate | Percentage of claims accepted on first submission |
| Net Collection Rate | Revenue collected vs. expected |
Implement dashboards for real-time tracking and regular reviews to identify issues quickly. For more strategies on optimizing RCM performance, see Strategies to Optimize RCM.
Case Example: Impact of Strategic RCM Improvements
Consider a multispecialty clinic that struggled with high A/R days and frequent denials. By automating eligibility checks, retraining staff, and outsourcing complex billing tasks, the clinic reduced A/R from 55 to 32 days and increased collections by 18 percent within six months.
Strategic improvements in revenue cycle billing deliver measurable, lasting results.
Future Trends and Strategies in Revenue Cycle Billing
As healthcare evolves, so does the landscape of revenue cycle billing. The market's rapid expansion, fueled by digital transformation and strategic collaborations, underscores the need for forward-thinking strategies. According to the RCM Market Growth Projections, the sector is set for substantial growth, highlighting the increasing importance of innovation in billing processes.
Embracing Automation and Artificial Intelligence
Automation and artificial intelligence are reshaping revenue cycle billing by streamlining tasks such as coding, claim scrubbing, and denial prediction. AI-powered solutions can flag high-risk claims before submission, reducing errors and expediting reimbursements. Practices leveraging these technologies benefit from lower manual workloads, faster payment cycles, and improved accuracy across the billing process.
Value-Based Care and RCM Alignment
The shift from fee-for-service to value-based care requires new approaches in revenue cycle billing. Organizations must adapt RCM processes to support quality metrics and bundled payments. Aligning billing strategies with value-based models helps practices track patient outcomes, meet payer requirements, and optimize financial performance in a changing reimbursement environment.
Data-Driven Decision Making
Advanced analytics are becoming essential tools in revenue cycle billing. By using real-time dashboards and predictive modeling, healthcare organizations can identify revenue leakage, monitor key performance indicators, and guide process improvements. Data-driven insights foster more informed decisions and support continuous optimization of billing operations.
Evolving Patient Expectations and Digital Payments
Patients increasingly expect digital billing, online payments, and transparent statements from their healthcare providers. Meeting these expectations with secure, user-friendly platforms enhances patient satisfaction and accelerates collections. Practices that embrace digital payment solutions can streamline processes, reduce administrative burdens, and stay competitive in a modern healthcare market. The RCM Market Trends Report highlights these trends as critical for future success.
Preparing for Regulatory and Market Changes
Staying agile in the face of regulatory updates and evolving payer models is vital for sustainable revenue cycle billing. Continuous process improvement, ongoing staff education, and proactive compliance strategies help organizations maintain financial resilience. Monitoring industry changes and adapting quickly ensures that billing operations remain effective and compliant in an ever-changing landscape.
If you’re ready to take your revenue cycle billing to the next level, now is the perfect time to put these strategies into action. By focusing on accuracy, proactive denial management, and leveraging technology, you can strengthen your financial performance and streamline your operations. At Greenhive Billing Solutions, we’re committed to helping healthcare practices like yours uncover hidden opportunities for growth and efficiency. Let’s work together to identify areas where you can improve collections and reduce denials—our team is here to support your goals every step of the way.
Get Your Free Audit