In 2026, healthcare organizations face mounting financial pressures, tighter regulations, and increased scrutiny from payers. Mastering revenue coding is now crucial for providers seeking to maintain profitability and compliance in this evolving landscape.
This guide is designed for healthcare leaders, practice managers, and coding professionals who want to stay ahead. Here, you will discover the latest best practices and step-by-step strategies to optimize your revenue coding processes.
Explore key regulatory changes, essential compliance updates, proven workflow improvements, technology’s growing impact, team development tips, and upcoming trends shaping 2026. Unlock actionable insights to maximize reimbursement, reduce denials, and protect your organization’s bottom line.
Ready to transform your revenue coding approach? Read on to gain the knowledge you need for sustainable success.
The Evolving Landscape of Revenue Coding in 2026
The landscape of revenue coding is evolving rapidly as healthcare organizations brace for new regulatory demands and heightened payer scrutiny. To stay competitive and compliant in 2026, organizations must understand the key changes, adapt to operational pressures, and recognize the central role of revenue coding in the revenue cycle.
Key Regulatory and Industry Changes
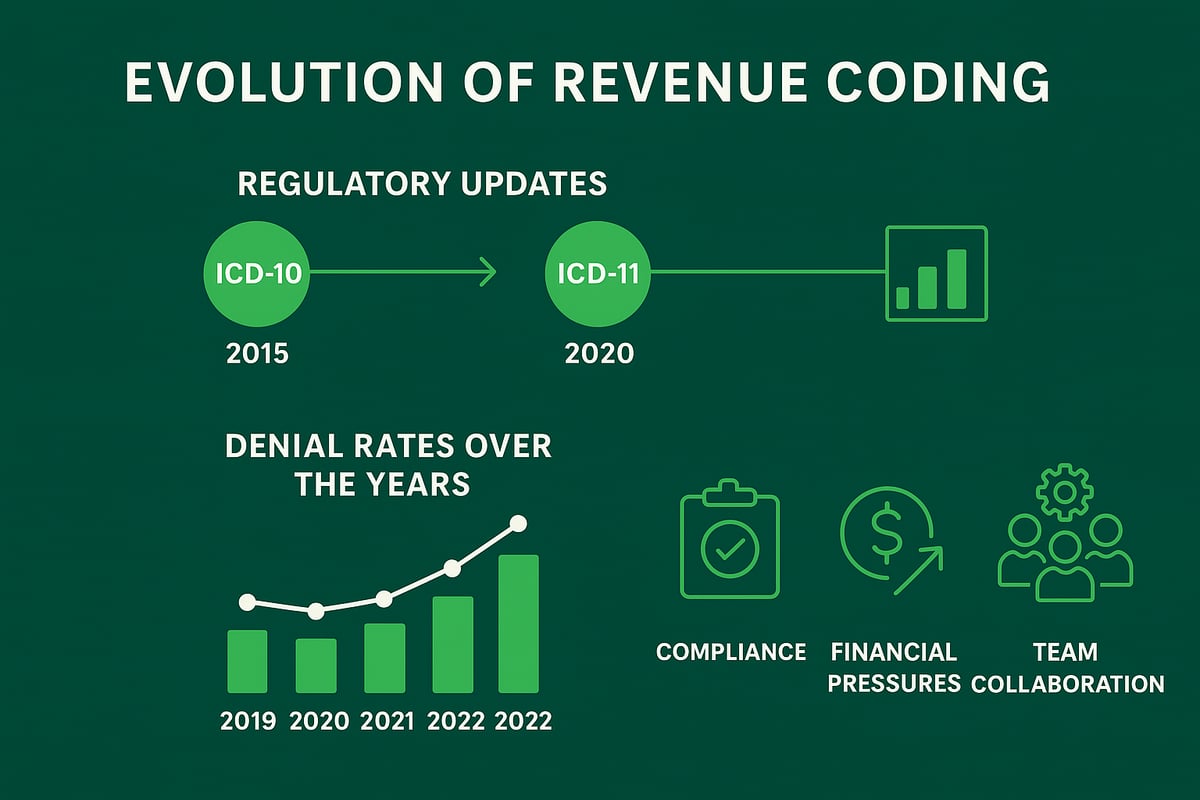
In 2026, healthcare organizations are adjusting to significant regulatory updates that directly impact revenue coding. The transition from ICD-10 to ICD-11 stands out as a major shift, requiring coders to learn new structures and adapt workflows. This change brings both challenges and opportunities, as ICD-11 offers greater specificity but demands retraining and system upgrades.
Payers are increasing audit frequency and applying stricter policies to claims. The Centers for Medicare & Medicaid Services (CMS) and private payers continue to refine reimbursement policies, leading to a rise in denial rates and compliance penalties. Value-based care models are influencing coding priorities, with a stronger focus on capturing quality metrics and outcomes.
Interoperability mandates are also shaping revenue coding practices. Healthcare organizations must ensure seamless data sharing across systems, which affects how codes are documented and reported. There is a growing emphasis on coding for social determinants of health (SDOH), as these factors become more relevant for reimbursement and population health management.
Financial and Operational Pressures on Providers
Providers are facing tighter margins due to rising operational costs and increasingly complex payer contracts. Revenue coding errors can result in substantial lost revenue, increased compliance risk, and potential reputational damage. For example, recent studies show that claims rejection rates have climbed, with the average days in accounts receivable (A/R) trending upward for many organizations.
Staffing shortages and coder burnout add to the challenge. The demand for remote and hybrid coding teams is growing, which requires robust communication protocols and workflow management. Inaccurate or delayed revenue coding can jeopardize cash flow and threaten organizational sustainability.
To mitigate these pressures, healthcare organizations must prioritize accurate and efficient revenue coding. This focus not only helps reduce denials but also supports overall financial health and compliance in a competitive landscape.
The Integral Role of Revenue Coding in Revenue Cycle Management
Revenue coding is the linchpin of effective revenue cycle management. Accurate coding ensures clean claims, timely reimbursement, and strong revenue integrity. By serving as the bridge between clinical documentation and financial outcomes, revenue coding connects the efforts of providers, billing teams, and compliance officers.
Consider the impact of coding optimization: organizations that invest in coding best practices often see measurable improvements in cash flow and a reduction in denial rates. For example, targeted interventions and regular audits can streamline workflows, minimize errors, and increase the likelihood of payment on first submission.
Revenue coding also supports denial management strategies, enabling teams to identify and address root causes of rejections. Collaboration between coding professionals and other RCM functions is essential for maintaining high performance and compliance. For more insight into the foundational role of revenue codes, explore Revenue codes in medical billing, which details how these codes influence reimbursement and regulatory adherence.
In summary, mastering revenue coding in 2026 requires a proactive approach to regulatory changes, operational challenges, and collaborative revenue cycle management. Organizations that prioritize continuous improvement will be better equipped to thrive in the evolving healthcare environment.
Essential Compliance and Documentation Standards for 2026
Staying compliant in revenue coding is more challenging than ever, with 2026 bringing new layers of complexity. Healthcare organizations must not only keep up with the latest coding standards but also ensure their documentation and regulatory practices are airtight. The following best practices will help you build a strong compliance foundation and protect your revenue streams.
Staying Current with Coding Standards
Up-to-date knowledge is the bedrock of effective revenue coding in 2026. Coding professionals should pursue ongoing education through credible organizations like AHIMA and AAPC, ensuring active certifications and exposure to the latest industry updates.
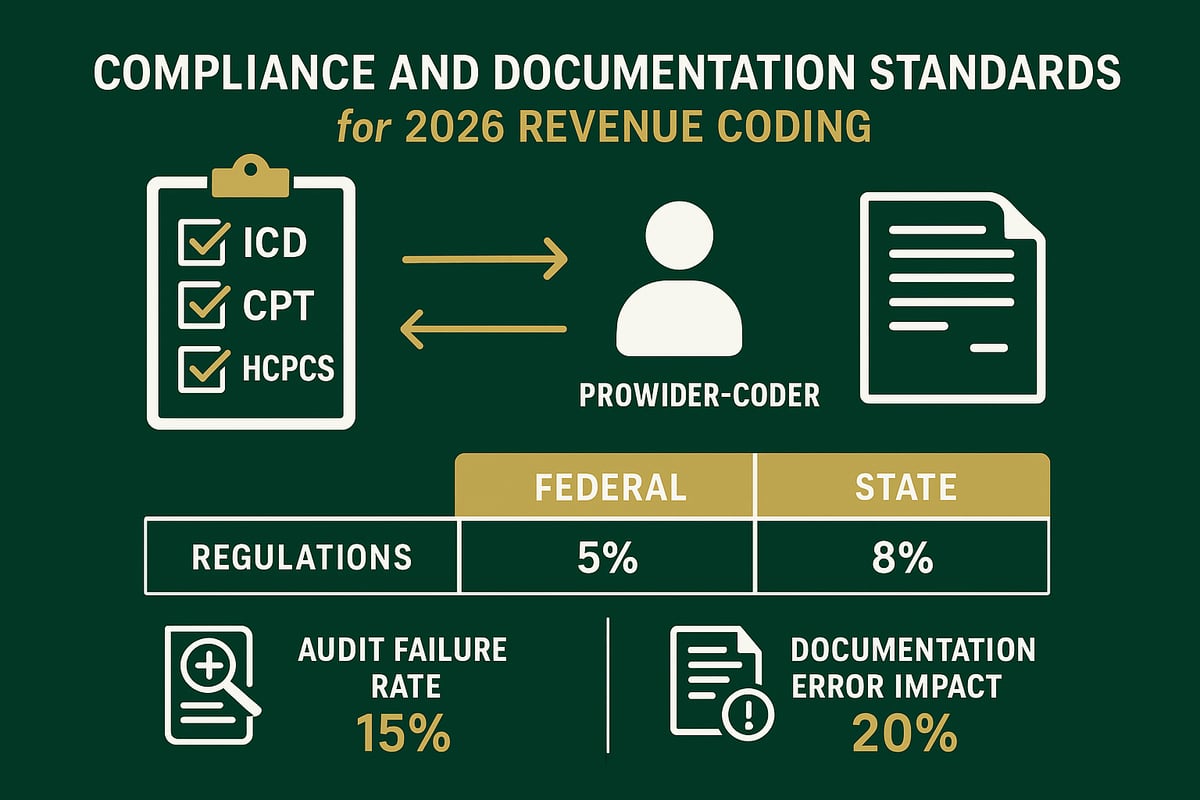
Quarterly updates to ICD, CPT, and HCPCS codes can dramatically impact billing practices. For instance, the 2026 ICD-10-CM Medical Coding Updates outline significant revisions that affect code selection and reimbursement. Missing these changes increases the risk of denials and compliance failures.
Key strategies for maintaining current standards include:
- Scheduling regular in-house or external coding workshops
- Reviewing official guidelines and payer bulletins each quarter
- Participating in webinars focused on revenue coding compliance
Recent data shows that nearly 30% of compliance audit failures are linked to outdated coding knowledge. By prioritizing continuous education, your team can avoid costly errors and maximize reimbursement.
Ensuring Thorough and Accurate Clinical Documentation
Accurate documentation is essential for supporting medical necessity and ensuring revenue coding specificity. Strong collaboration between providers and coders helps close gaps and reduce errors.
Implementing Clinical Documentation Improvement (CDI) initiatives can streamline this process. Consider using standardized templates or checklists to promote consistency across all clinical notes. This approach supports accurate code assignment and reduces variability.
Best practices for documentation excellence:
- Schedule regular provider-coder feedback sessions
- Use documentation templates tailored for specialty services
- Incorporate checklists for required data elements
Incomplete or vague documentation leads to higher claim denial rates. For example, missing details on patient status or service specifics can trigger payer rejections. Investing in documentation quality pays dividends in both compliance and financial performance.
Navigating Federal and State Regulations
Navigating the regulatory landscape is a core component of revenue coding success. Federal requirements like HIPAA, OIG, and CMS rules set the baseline for compliant coding and billing. However, state-specific regulations—including Medicaid, workers’ compensation, and commercial payer rules—add layers of complexity.
A robust compliance program should include:
- Routine internal audits of coding and billing practices
- State-by-state tracking of unique policy requirements
- Documentation retention policies and audit trails
Recent enforcement actions show a sharp increase in penalties for non-compliance, especially in telehealth coding, which has evolved rapidly since the pandemic. Audit trails are now essential for defending claim integrity and demonstrating due diligence.
Below is a summary table highlighting key differences:
| Regulatory Focus | Federal Requirements | State-Specific Nuances |
|---|---|---|
| HIPAA | Universal | May have additional privacy laws |
| CMS/OIG | National coverage determinations | Medicaid rules vary by state |
| Telehealth | Standardized codes, evolving | Varies, post-pandemic expansions |
Staying proactive with audit readiness and regulatory monitoring ensures that your revenue coding processes remain resilient, even as the landscape evolves. Compliance is not just a checkbox but a strategic advantage in the current healthcare environment.
Step-by-Step Best Practices for Revenue Coding Excellence
In 2026, achieving revenue coding excellence is not just about accuracy, but about building a resilient, adaptable process that aligns with both regulatory demands and organizational goals. The following five steps outline a clear roadmap for healthcare organizations to optimize revenue coding, ensure compliance, and drive financial performance.
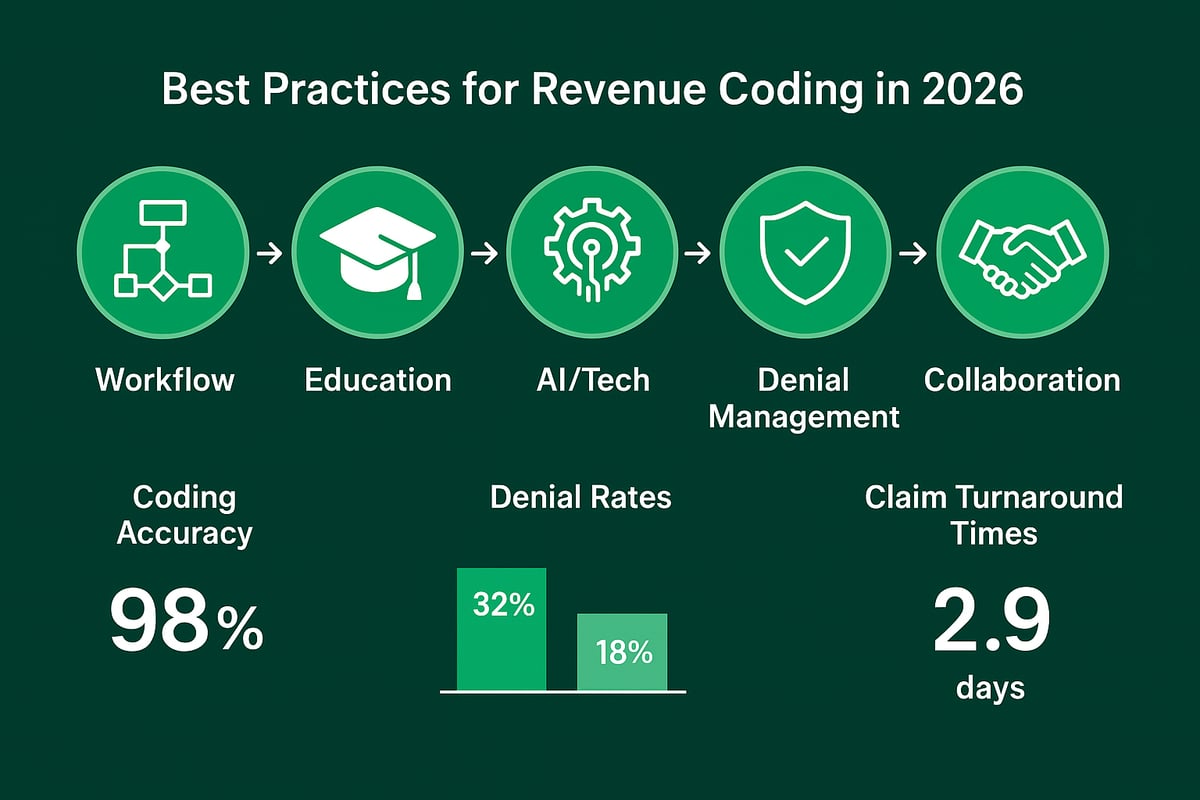
Step 1: Establish Robust Coding Workflows
The foundation of effective revenue coding is a well-defined workflow. Begin by mapping every stage from patient encounter to claim submission. This includes:
- Intake and documentation review
- Code assignment and validation
- Quality checks and edits
- Claim submission and follow-up
Assign clear responsibilities to each coder, including escalation paths for complex cases. Integrate workflows with EHRs and practice management systems to streamline data flow and reduce manual entry. For example, a small clinic may use a simple linear workflow, while a large practice benefits from branching workflows to manage specialty coding needs.
Tracking turnaround time at each stage ensures bottlenecks are identified and resolved quickly. This step is crucial for revenue coding teams aiming to maintain clean claims and predictable cash flow.
Step 2: Invest in Continuous Education and Training
Regulatory changes and payer requirements evolve rapidly, making ongoing education vital for revenue coding teams. Schedule regular coding workshops focused on the latest ICD, CPT, and HCPCS updates. Encourage certification renewals through organizations like AHIMA or AAPC.
Cross-training coders in specialty areas, such as behavioral health or orthopedics, increases team versatility. Compare in-house versus external training to determine ROI and select the best fit for your organization. Staying ahead in revenue coding knowledge directly reduces compliance risks and improves claim accuracy.
Step 3: Leverage Technology for Coding Accuracy
Technology is a powerful ally in revenue coding. Utilize computer-assisted coding (CAC) tools and AI-enabled platforms to minimize human error and accelerate code assignment. Ensure integration with client-owned EHRs for real-time edits and validation.
Data analytics can highlight coding trends, spot outliers, and support proactive improvements. For example, implementing CAC tools has shown to reduce coding error rates by up to 30 percent in some organizations. As a service provider, adapting to each client’s systems ensures consistent results and streamlined revenue coding processes.
Step 4: Implement Proactive Denial Management
Denial management is critical for protecting revenue streams. Begin with root cause analysis to identify patterns in coding-related denials. Implement automated denial tracking systems that generate real-time reports and support targeted interventions.
Establish feedback loops between coders, billers, and providers to address recurring issues. For example, a cardiology group reduced denials by 18 percent after regular review sessions and process adjustments. Specialty-specific data shows that coding-related denial rates can vary widely, underscoring the need for tailored strategies.
Explore more proven denial management tactics in Denial management in medical billing, which offers practical insights for optimizing revenue coding and reimbursement.
Step 5: Foster Interdepartmental Collaboration
Revenue coding does not exist in isolation. Schedule regular meetings between coding, billing, and clinical teams to review complex cases and share updates. Jointly reviewing documentation uncovers gaps and supports continuous clinical documentation improvement.
Set shared KPIs and accountability structures to align goals across departments. For example, healthcare organizations that implemented cross-team initiatives saw measurable improvements in claim turnaround times and overall revenue cycle performance.
Open communication channels are essential for sustaining collaboration and driving ongoing revenue coding excellence.
The Role of Technology and Automation in Modern Revenue Coding
The landscape of revenue coding is rapidly shifting, driven by technological innovation and automation. For healthcare organizations, leveraging the right digital tools is not optional, but essential for maintaining accuracy, compliance, and profitability. As the demands of 2026 increase, staying ahead with modern solutions ensures smoother workflows and better financial outcomes.
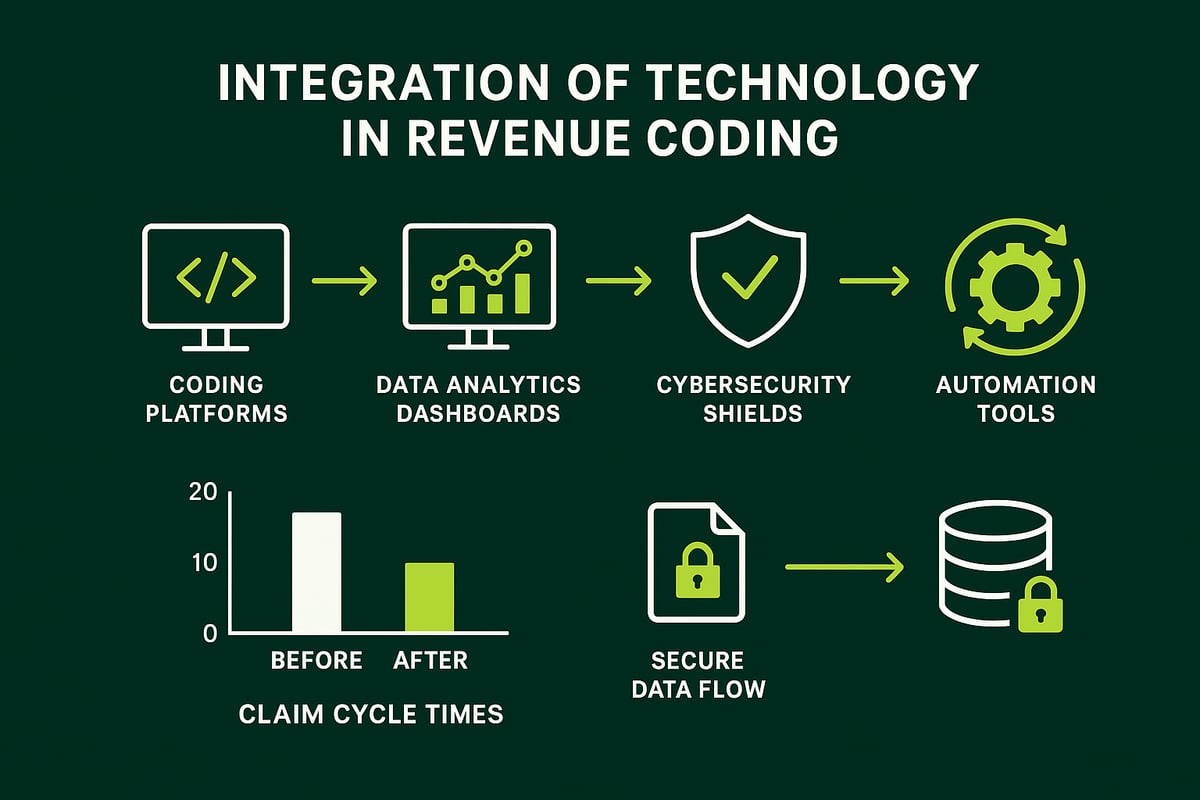
Digital Tools Transforming Revenue Coding
Healthcare providers now rely on a spectrum of digital tools to optimize revenue coding. Leading coding and revenue cycle management (RCM) platforms streamline workflows, minimize manual entry, and enable real-time claim edits. Automated coding edits and claim scrubbing help prevent errors before claims are submitted, reducing rejections and accelerating payments.
Real-time eligibility verification and prior authorization tools have become standard, helping teams avoid delays and denials. For example, automation can reduce claim cycle times by identifying missing details or flagging inconsistencies for correction before submission.
Service providers like our team adapt to client-owned software, ensuring seamless integration with existing EHRs and practice management systems. This flexibility allows for tailored solutions aligned with each organization's unique needs, enhancing overall revenue coding accuracy and efficiency.
Data Analytics and Reporting for Performance Improvement
Data analytics is a game changer for revenue coding, offering actionable insights into productivity, error rates, and denial patterns. Dashboards provide real-time visibility into key performance indicators, making it easier to monitor coder output and claim status.
Predictive analytics can identify high-risk claims before submission, enabling proactive interventions and reducing the likelihood of denials. Benchmarking performance against industry standards or peer groups highlights areas for improvement and fosters a culture of continuous growth.
According to Healthcare revenue cycle analytics, organizations using advanced analytics report higher clean claim rates and improved cash flow. By harnessing data, healthcare leaders can drive targeted training, refine processes, and maximize the financial return of revenue coding efforts.
Cybersecurity and Data Privacy Considerations
With increased digitization of revenue coding comes heightened responsibility for data privacy. Ensuring HIPAA compliance is non-negotiable, especially when handling sensitive patient information across multiple platforms.
Secure data transfer protocols and robust access controls are vital for preventing breaches and audit failures. For example, regular security audits and encrypted communications protect both clinical and financial data from unauthorized access.
Proactive cybersecurity measures not only safeguard information but also preserve the integrity and trustworthiness of revenue coding operations. In today’s regulatory environment, strong data privacy practices are essential for sustainable success.
Building and Retaining High-Performing Coding Teams
Building and retaining high-performing teams is essential for sustained excellence in revenue coding. As the landscape grows more complex, healthcare organizations must adopt strategic approaches to talent acquisition, training, performance management, and retention. Let us explore practical steps to create a robust revenue coding workforce.
Recruiting and Onboarding Top Coding Talent
Recruiting skilled professionals is the foundation of strong revenue coding teams. Focus on candidates with credentials from AHIMA or AAPC, as well as experience in multiple coding systems. When evaluating applicants, ensure they understand different types of medical coding relevant to your organization’s services.
A structured onboarding process accelerates productivity and reduces errors. Include shadowing, documentation standards training, and system-specific workflow introductions. Review onboarding progress regularly to identify knowledge gaps early. This approach leads to fewer mistakes and a smoother integration of new hires into revenue coding roles.
Training, Upskilling, and Career Development
Continuous education is vital in the ever-changing world of revenue coding. Schedule regular internal workshops and encourage coders to pursue advanced certifications. Offer cross-training for specialties such as radiology or behavioral health to expand team capability.
Mentorship programs and peer review sessions foster a culture of learning and accountability. Track the impact of training investments by monitoring accuracy rates and audit outcomes. Supporting ongoing development not only strengthens expertise but also boosts employee engagement and retention in revenue coding teams.
Performance Management and Incentives
Effective performance management ensures that revenue coding teams consistently deliver high-quality results. Set clear productivity and quality metrics, such as clean claim rates and average coding turnaround times. Use dashboards to visualize progress and address issues promptly.
Implement recognition programs to reward top performers, whether through bonuses, public acknowledgment, or career advancement opportunities. Incentive structures tied to measurable outcomes drive motivation and foster a results-oriented culture. By aligning incentives with organizational goals, you help revenue coding professionals stay focused and committed.
Addressing Burnout and Retention Challenges
Burnout can undermine the effectiveness of revenue coding teams. To combat this, offer flexible work arrangements, such as remote or hybrid schedules, which accommodate different lifestyles. Promote wellness through access to counseling, stress management resources, and reasonable workloads.
Regularly assess team morale and solicit feedback to identify potential issues early. Supportive policies, open communication, and a focus on work-life balance contribute to lower turnover rates. Investing in coder well-being ensures long-term stability and excellence in revenue coding.
Future Trends and Strategic Recommendations for 2026 and Beyond
The landscape of revenue coding is shifting faster than ever as 2026 approaches. B2B healthcare organizations must stay ahead of regulatory, technological, and operational changes to secure their financial future. Here, we explore the most critical trends and offer actionable strategies for ongoing excellence.
Anticipated Regulatory and Industry Shifts
By 2026, revenue coding will be shaped by sweeping regulatory changes. The shift to ICD-11, expanded value-based care models, and increased payer requirements demand constant vigilance. Coding for social determinants of health (SDOH) and telehealth continues to grow in importance, requiring teams to adapt rapidly. Staying updated on coding revisions is essential, and official sources such as the ICD-10 & Other Coding Revisions from CMS provide crucial updates. Organizations that prioritize compliance and responsiveness to these shifts will reduce denials and maximize reimbursement.
The Expanding Role of Artificial Intelligence
Artificial intelligence is rapidly transforming revenue coding, improving both accuracy and efficiency. AI-powered tools can flag coding discrepancies, automate repetitive tasks, and help coders focus on complex cases. However, human oversight remains essential to ensure ethical use and to interpret nuanced clinical scenarios. As explored in AI Medical Coding: The Future of RCM in 2026, AI is most effective when integrated with skilled professionals who understand both technology and compliance. Forward-thinking organizations are using AI to gain a competitive edge in revenue coding while maintaining rigorous quality controls.
Preparing for Increased Audit and Compliance Demands
Audit activity is expected to intensify in the coming years, making audit readiness a top priority for revenue coding teams. Internal audit programs, regular documentation reviews, and external partnerships can help organizations stay ahead of payer and government scrutiny. Recent trends show an uptick in both the frequency and complexity of audits, especially in areas like telehealth and SDOH coding. Establishing clear audit trails and robust documentation retention policies is essential. By proactively addressing compliance risks, healthcare organizations can safeguard revenue and reputation.
Strategic Recommendations for Healthcare Organizations
To excel in revenue coding through 2026 and beyond, healthcare organizations must invest in people, process, and technology. This means upskilling coding professionals, refining workflows, and leveraging advanced tools while adapting to client systems. Building organizational agility is critical to respond to ongoing regulatory and payer changes. Success stories show that organizations leading in revenue coding innovation achieve better denial rates and faster reimbursement. By focusing on continuous improvement and collaboration, B2B healthcare providers can secure sustainable growth and operational excellence.
As you navigate the complexities of revenue coding in 2026, you understand how vital it is to stay ahead of regulatory shifts, evolving payer requirements, and the increasing demands on your team. Mastering best practices not only strengthens compliance but also positions your organization for greater financial success. If you’re ready to put these strategies into action and want expert guidance tailored to your unique needs, let’s connect. We can discuss how to streamline your processes, boost accuracy, and maximize reimbursements for your practice.
Book Your Free Consultation