In today’s healthcare landscape, mastering rcm in medical coding is essential for financial success and ongoing compliance. Healthcare organizations rely on effective revenue cycle management to ensure accurate reimbursement, reduce delays, and maintain patient satisfaction.
With increasing claim denials, evolving payer requirements, and shifting regulations, medical practices and providers face significant challenges. Expert RCM is no longer optional, it is a necessity for sustaining profitability and operational efficiency.
This comprehensive guide will walk you through the essentials of rcm in medical coding. Discover proven strategies to optimize your revenue cycle, prevent denials, and maximize reimbursements. We will explore core concepts, practical steps, compliance standards, technology’s impact, and how to choose the right RCM partner for your practice.
Understanding Revenue Cycle Management in Medical Coding
Revenue Cycle Management (RCM) in medical coding is the backbone of every successful healthcare organization’s financial operations. It covers the entire process of tracking patient care episodes from registration through final payment, ensuring that all services are coded, billed, and reimbursed accurately.
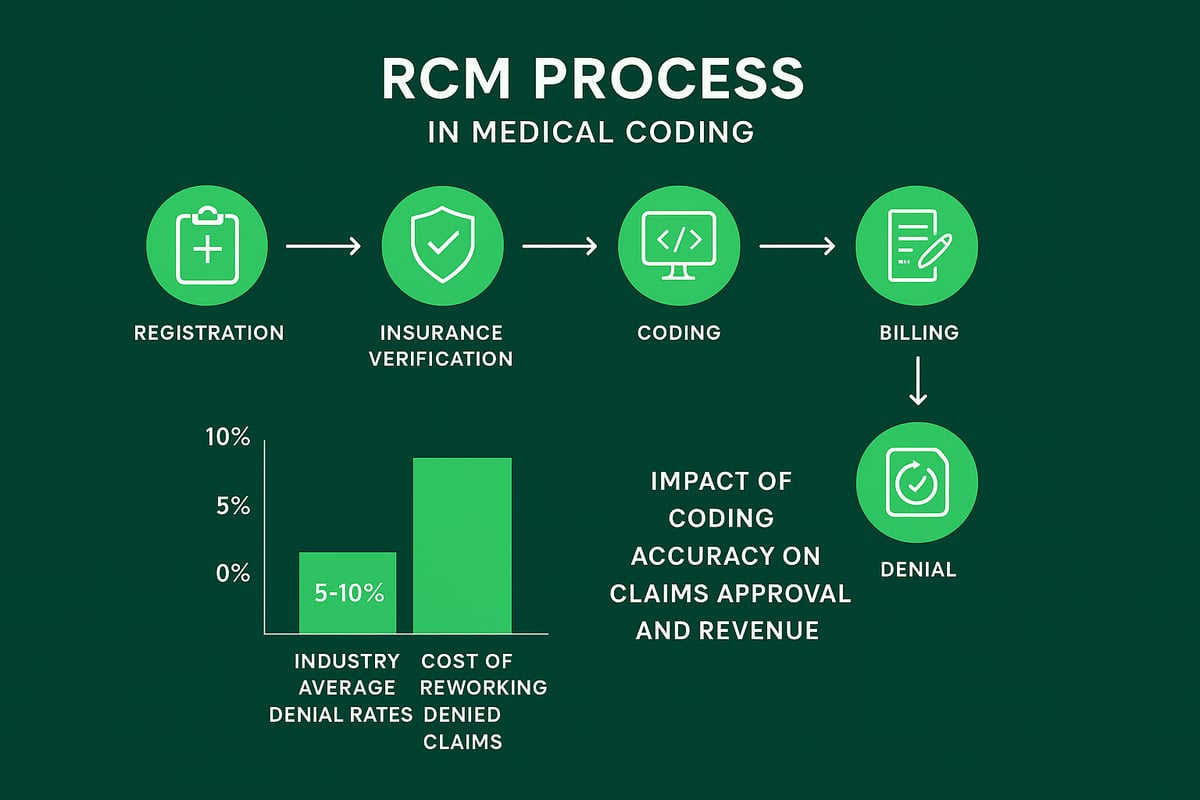
Key components of RCM include:
- Patient registration
- Insurance verification
- Medical coding
- Billing and claims submission
- Payment posting
- Denial management
Accurate medical coding is essential for effective RCM. Even a single coding error can trigger a claim denial, leading to delayed payments or lost revenue. Industry data shows that average claim denial rates range from 5% to 10%, and reworking denied claims can cost providers significant time and money.
Common pain points in rcm in medical coding include claim denials, delayed reimbursements, and compliance risks. These issues can reduce profitability, disrupt cash flow, and negatively impact the patient experience. For example, if a procedure is coded incorrectly, reimbursement may be denied, resulting in direct revenue loss.
The importance of employing trained professionals and certified coders cannot be overstated. Their expertise ensures compliance, reduces errors, and supports a seamless revenue cycle. For a deeper look at how accurate coding drives RCM success, explore this Medical coding and RCM connection.
The Step-by-Step RCM Process for Healthcare Providers
Navigating the step-by-step process of rcm in medical coding ensures healthcare organizations maintain financial stability and regulatory compliance. Each phase plays a critical role in maximizing revenue, reducing errors, and supporting a healthy cash flow. Here’s how each stage breaks down for providers and practice leaders.
![]()
Patient Access and Pre-Authorization
Accurate patient registration and insurance verification are the first lines of defense in rcm in medical coding. Collecting complete demographic and insurance data upfront prevents errors that can delay claims or lead to denials.
Pre-authorization is especially important for certain procedures. If pre-authorization is missed, claims may be rejected, causing lost revenue and administrative burden.
- Always verify insurance eligibility before services
- Obtain and document required pre-authorizations
- Educate front-desk staff on payer requirements
A single oversight at this stage can cascade into denied claims and longer reimbursement cycles. For a comprehensive overview of each phase, explore revenue cycle management in billing.
Medical Coding and Charge Capture
The next critical step in rcm in medical coding is assigning precise ICD-10, CPT, and HCPCS codes to every service provided. Certified medical coders help ensure accuracy, compliance, and proper reimbursement.
Charge capture involves recording all billable services. Missing charges or incorrect codes can lead to substantial revenue leakage.
- Use coding audits to spot common errors
- Train staff regularly on code updates
- Implement dual review for complex cases
Improper coding not only delays payment, it also increases compliance risks and the administrative cost of reworking denied claims.
Claims Submission, Payment Posting, and Denial Management
Timely, accurate claims submission is the backbone of rcm in medical coding. Submitting clean claims to payers minimizes delays and rejections.
Once payments arrive, they must be posted promptly to reconcile accounts and identify discrepancies or underpayments. Denial management involves analyzing root causes, appealing denied claims, and resubmitting as needed.
- Track clean claim rates and days in A/R
- Use denial codes to identify recurring issues
- Set up alerts for underpayments
Proactive denial management can dramatically reduce accounts receivable days, improving cash flow and overall performance.
Revenue Reporting and Performance Analysis
Regular revenue reporting and analytics are essential to monitor the effectiveness of the rcm in medical coding process. Dashboards and key performance indicators (KPIs) help identify trends, bottlenecks, and areas for improvement.
- Review KPIs monthly with billing teams
- Analyze denial patterns and root causes
- Use analytics to inform training and workflow changes
Continuous performance analysis enables practices to adapt quickly and maintain a competitive edge.
Ensuring Compliance and Reducing Risk in RCM
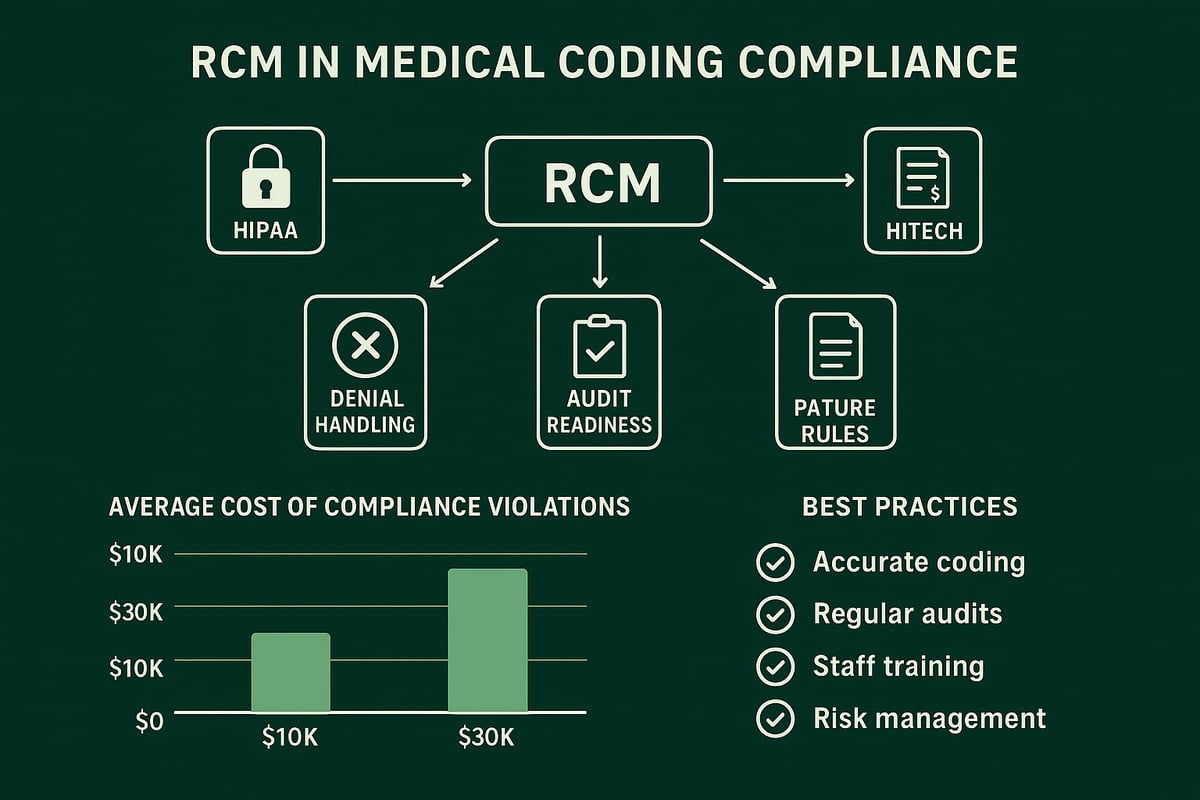
Navigating compliance is fundamental for any organization involved in rcm in medical coding. The healthcare industry faces strict regulations, with HIPAA and HITECH setting the standards for patient data privacy, security, and electronic health information management. Payer-specific rules further complicate the landscape, making it essential for providers to stay updated and agile.
Accurate clinical documentation is the foundation of audit readiness. Every code and patient record must align with regulatory requirements. Inaccuracies not only trigger claim denials but also increase the risk of audits and penalties. Non-compliance can result in steep fines, lost revenue, and significant reputational damage. According to industry data, the average cost of a single compliance violation can reach tens of thousands of dollars, emphasizing the financial impact of errors.
To mitigate risks in rcm in medical coding, organizations should implement ongoing training and regular internal audits. Keeping coding standards and payer policies current is vital. A strong compliance program, supported by routine education, helps reduce coding errors and supports audit preparedness. For a deeper dive into best practices, explore these denial management strategies.
Secure data handling is non-negotiable. Protecting patient information with robust access controls, encryption, and monitoring is necessary for HIPAA compliance. External reviews can provide an additional safety net, ensuring all processes align with the latest regulatory expectations. Proactive compliance fosters trust, reduces legal risk, and supports long-term financial health.
The Role of Technology and Outsourcing in Modern RCM
Modern RCM in medical coding demands agility, accuracy, and efficiency. To meet these standards, healthcare organizations increasingly turn to advanced technology and expert outsourcing partners. These strategies help streamline workflows, boost compliance, and drive measurable financial results.
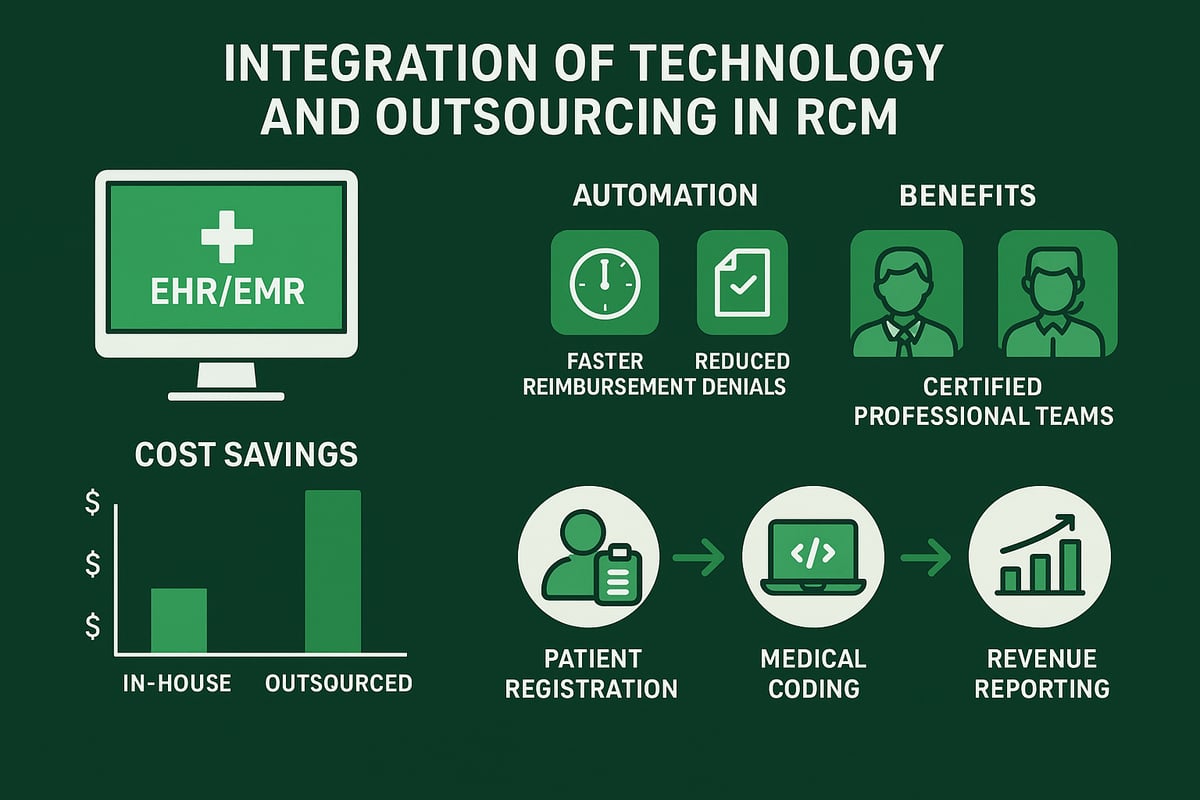
Leveraging RCM Platforms and Automation
Integrating EHR or EMR platforms with RCM in medical coding optimizes every step, from eligibility checks to claim status tracking. Automation tools speed up data entry, suggest accurate codes, and flag errors before claims are sent. According to AI and Automation in RCM, organizations leveraging automation report faster reimbursement cycles and higher first-pass acceptance rates.
Automation not only reduces manual errors but also gives teams more time to focus on complex cases. Real-time edits and alerts help minimize denials, supporting greater revenue integrity.
Outsourcing RCM Services to Certified Experts
Many healthcare providers choose to outsource RCM in medical coding to specialized teams. Outsourcing brings access to certified professionals, proven processes, and scalable support for growing practices. By partnering with experts, organizations can cut administrative costs, lower denial rates, and improve collections.
Selecting a reliable RCM partner ensures your billing aligns with current regulations and payer requirements. Outsourcing also enables providers to focus on patient care while experts handle the revenue cycle.
Greenhive Billing Solutions: Your RCM Partner
Greenhive Billing Solutions delivers end-to-end, HIPAA-compliant RCM services tailored for healthcare organizations. Our certified professionals manage coding, billing, denial management, and analytics, all while working within your existing software systems.
Clients benefit from reduced denials, measurable cost savings, and improved revenue outcomes. With Greenhive, practices nationwide experience seamless integration and results-driven RCM support.
Key Metrics and Best Practices for RCM Success
To achieve financial stability and compliance, healthcare organizations must track critical performance metrics and implement best practices for rcm in medical coding.
Key Performance Indicators (KPIs) in RCM
Success in rcm in medical coding depends on monitoring essential KPIs. The most valuable metrics include clean claim rate, denial rate, days in accounts receivable (A/R), and net collection rate. Clean claim rate, for instance, measures the percentage of claims accepted by payers on the first submission. Industry leaders target rates above 95 percent, as highlighted in Clean claim rates in billing.
Regularly benchmarking these figures allows organizations to identify gaps and set measurable goals. Tracking trends over time helps teams act quickly when performance dips, ensuring consistent cash flow and fewer payment delays.
Best Practices for RCM Optimization
Top-performing organizations in rcm in medical coding prioritize regular staff training and workflow standardization. Certified coders stay up to date on payer rules and regulatory changes, reducing errors and denials. Proactive denial prevention, such as root cause analysis and targeted feedback, further boosts clean claim rates and shortens A/R cycles.
Real-time analytics and actionable reporting are essential for making data-driven decisions. Dashboards provide instant visibility into bottlenecks, allowing leaders to respond with agility.
Continuous Improvement and Communication
Continuous process improvement relies on open communication between billing teams, providers, and patients. Sharing insights and feedback ensures everyone is aligned on documentation, coding, and claims management practices. By fostering a culture of transparency and accountability, healthcare organizations can adapt to changes and maintain excellence in rcm in medical coding.
Now that you understand how effective revenue cycle management can transform your practice’s financial health and ease administrative burdens, it’s a great time to take the next step toward measurable improvement. If you’re curious about where your revenue cycle might be leaking value or how your current processes stack up to industry benchmarks, we’re here to help. Let’s identify opportunities for increased efficiency, reduced denials, and better reimbursement—tailored to your unique needs. Ready to see how expert guidance can make a real difference? Get Your Free Audit