Accurate claim submission in medical billing is the backbone of financial success for healthcare organizations. Even a small error can lead to delayed payments, denied claims, and significant revenue loss.
This guide is designed for providers and billing professionals who want to master every step of claim submission in medical billing. You will gain practical strategies to streamline your workflow, avoid common pitfalls, and achieve faster reimbursements.
We will walk through the entire process, from required documentation to electronic versus paper claims and proven best practices. Discover actionable solutions to industry challenges and unlock more efficient billing that drives consistent results for your practice.
Understanding Claim Submission in Medical Billing
Accurate claim submission in medical billing is the linchpin of financial success for healthcare organizations. Without a robust process, practices risk delayed payments, denied claims, and lost revenue. Understanding the fundamental steps and requirements empowers providers and billing teams to build a stronger revenue cycle and minimize costly errors.
What is Claim Submission?
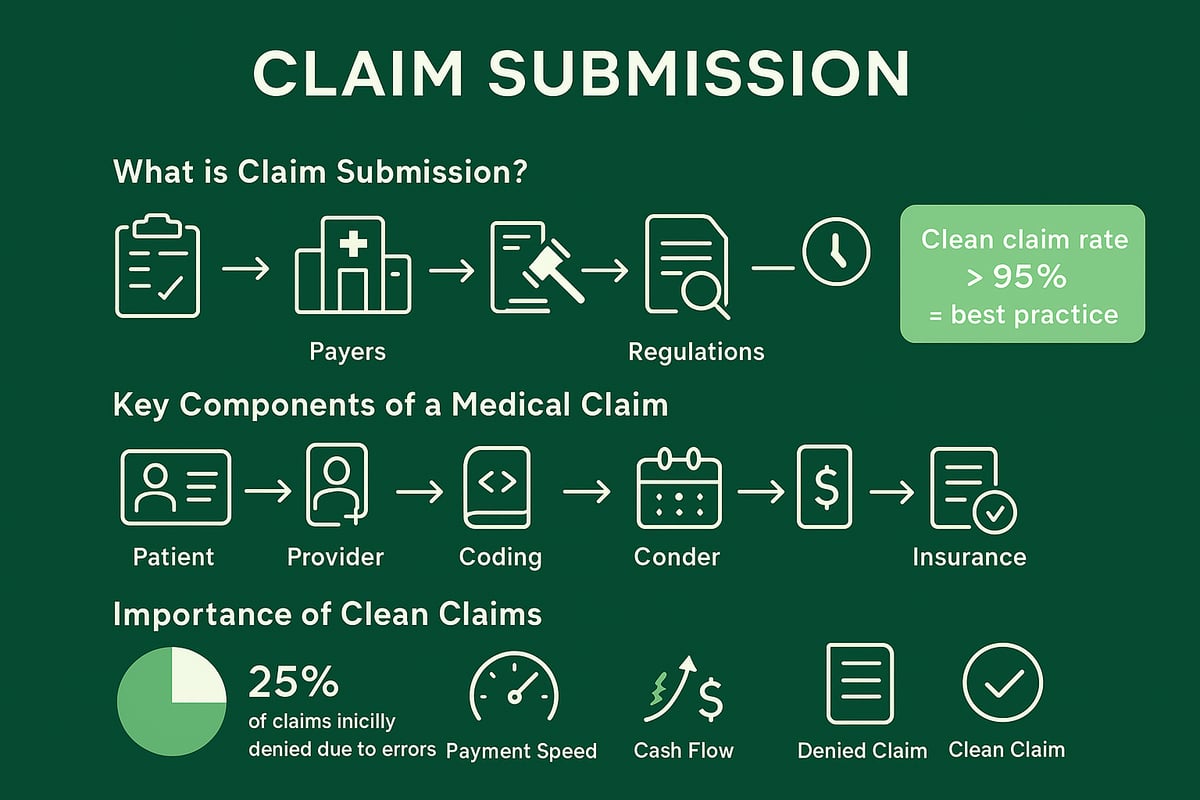
Claim submission in medical billing refers to the process of sending detailed requests for reimbursement to insurance payers after healthcare services are provided. It is the vital connection between services rendered and payment received, directly impacting cash flow and practice sustainability.
There are several claim types, including institutional and professional claims, as well as primary, secondary, and tertiary submissions. Compliance with regulations such as HIPAA and payer-specific rules is mandatory. For example, submitting a CMS 1500 form for outpatient care is routine, but accuracy is critical—over 25% of claims are initially denied or rejected because of submission errors.
For organizations seeking efficiency, Medical claim submission services can streamline this process, reduce errors, and accelerate reimbursement cycles.
Key Components of a Medical Claim
A successful claim submission in medical billing relies on complete and precise information. Each claim should include:
- Patient demographics: full name, date of birth, insurance policy details
- Provider information: NPI, address, tax ID
- Procedure and diagnosis codes: CPT, ICD-10 or ICD-11, HCPCS
- Dates and locations of services
- Charges, modifiers, and authorization/pre-authorization details
Missing or incorrect data, such as failing to include an ICD-10 code, can result in an automatic denial. Ensuring all required fields are filled and codes are correct is essential for claims to be processed without delay.
Importance of Clean Claims
A clean claim is one that is error-free, complete, and fully compliant with payer requirements. Achieving a high clean claim rate is the gold standard in claim submission in medical billing, as it speeds up reimbursement and improves cash flow.
The cost to rework a denied claim averages around $25, not including lost time and delayed revenue. Clean claims are typically paid within 30 days, while those with errors may take over 90 days to resolve. Industry leaders strive for clean claim rates above 95 percent, ensuring optimal financial performance.
Step-by-Step Claim Submission Process
Every healthcare practice relies on an efficient claim submission in medical billing to maintain healthy cash flow and reduce costly delays. A streamlined workflow not only accelerates payments but also minimizes errors that can lead to denials. Let’s break down the essential steps in the process, ensuring each phase is managed with precision and expertise.
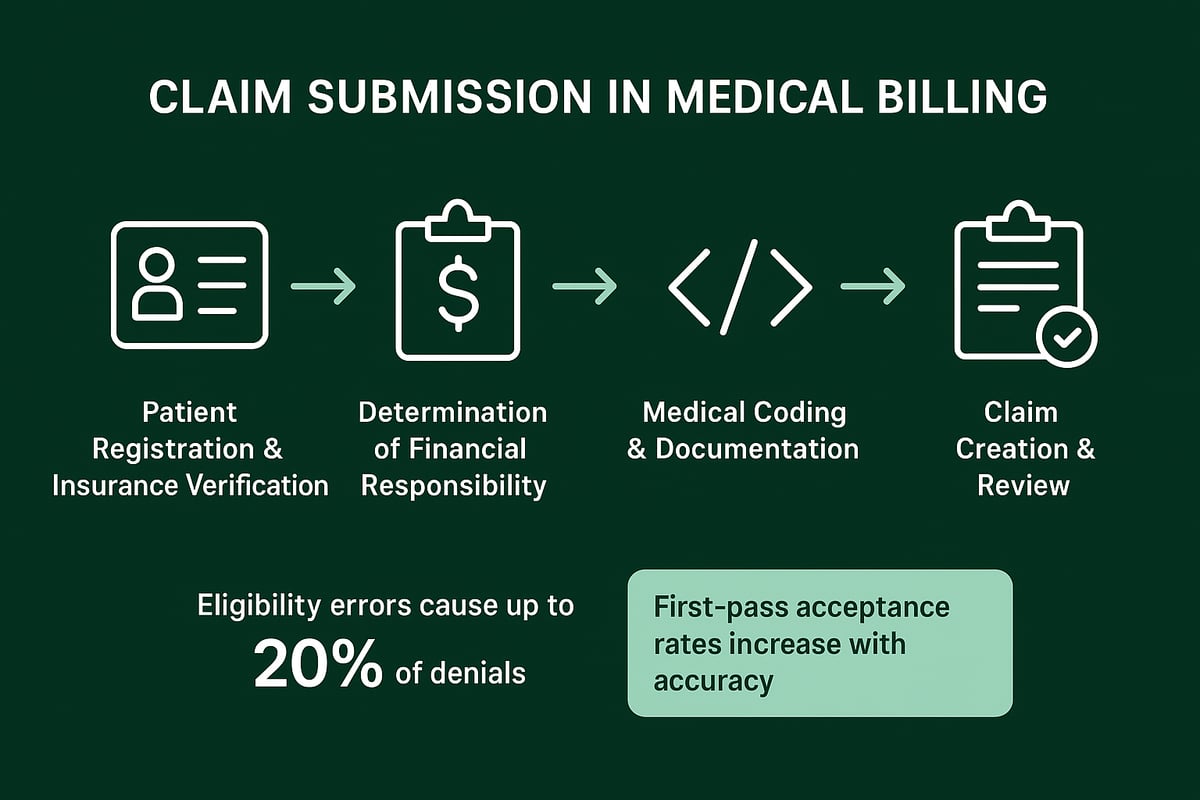
Step 1: Patient Registration and Insurance Verification
The first step in claim submission in medical billing is capturing accurate patient data and verifying insurance coverage before services are rendered. Collect essential information such as full name, date of birth, insurance details, and contact information.
Always confirm the patient’s eligibility and benefits using real-time tools or direct communication with payers. Even a minor error at this stage, like a wrong policy number, can result in immediate claim rejection. In fact, eligibility errors are responsible for up to 20% of claim denials. For a deeper understanding of this foundational step, see insurance verification in medical billing.
By addressing verification early in the process, practices avoid downstream issues that can disrupt the entire claim submission in medical billing workflow.
Step 2: Determination of Financial Responsibility
After confirming insurance, the next step in claim submission in medical billing is clearly defining what the patient owes. Identify copays, deductibles, and coinsurance based on the patient’s plan. Communicate these costs upfront to prevent confusion and payment delays.
It is critical to obtain any required pre-authorizations for specific procedures. Missing authorizations often result in non-payment, even if the service was medically necessary. Transparent communication at this stage reduces future disputes and improves the likelihood of successful collections.
Practices that prioritize this step in claim submission in medical billing see fewer denied claims and a more predictable revenue stream.
Step 3: Medical Coding and Documentation
Accurate coding is at the heart of claim submission in medical billing. Assign the correct ICD-10/ICD-11 and CPT/HCPCS codes for every service performed. Ensure that all supporting documentation, such as progress notes and procedure reports, matches the codes used.
Common errors include upcoding, undercoding, or mismatched codes, which can lead to immediate denial. For example, billing for a service without proper documentation is a frequent reason for rejections. Utilizing certified coders and conducting regular audits are proven strategies to minimize mistakes and uphold compliance throughout the claim submission in medical billing process.
Step 4: Claim Creation and Review
The final step in claim submission in medical billing involves assembling all information into standardized claim forms like CMS-1500 or UB-04. Carefully review the claim for completeness, accuracy, and alignment with payer requirements.
Employ claim scrubbing tools to automatically detect errors before submission. Missing critical details, such as the provider’s NPI, can cause unnecessary payment delays. A thorough review not only increases first-pass acceptance rates but also reduces the administrative burden of reworking denied claims.
By following these steps, healthcare organizations can optimize claim submission in medical billing, leading to faster reimbursements and improved financial performance.
Methods of Claim Submission: Electronic vs. Paper
Choosing the right method for claim submission in medical billing directly impacts reimbursement speed and accuracy for healthcare providers. Understanding both electronic and paper claim workflows helps organizations streamline billing operations and minimize costly errors. Let’s examine the strengths, weaknesses, and industry standards for each approach.
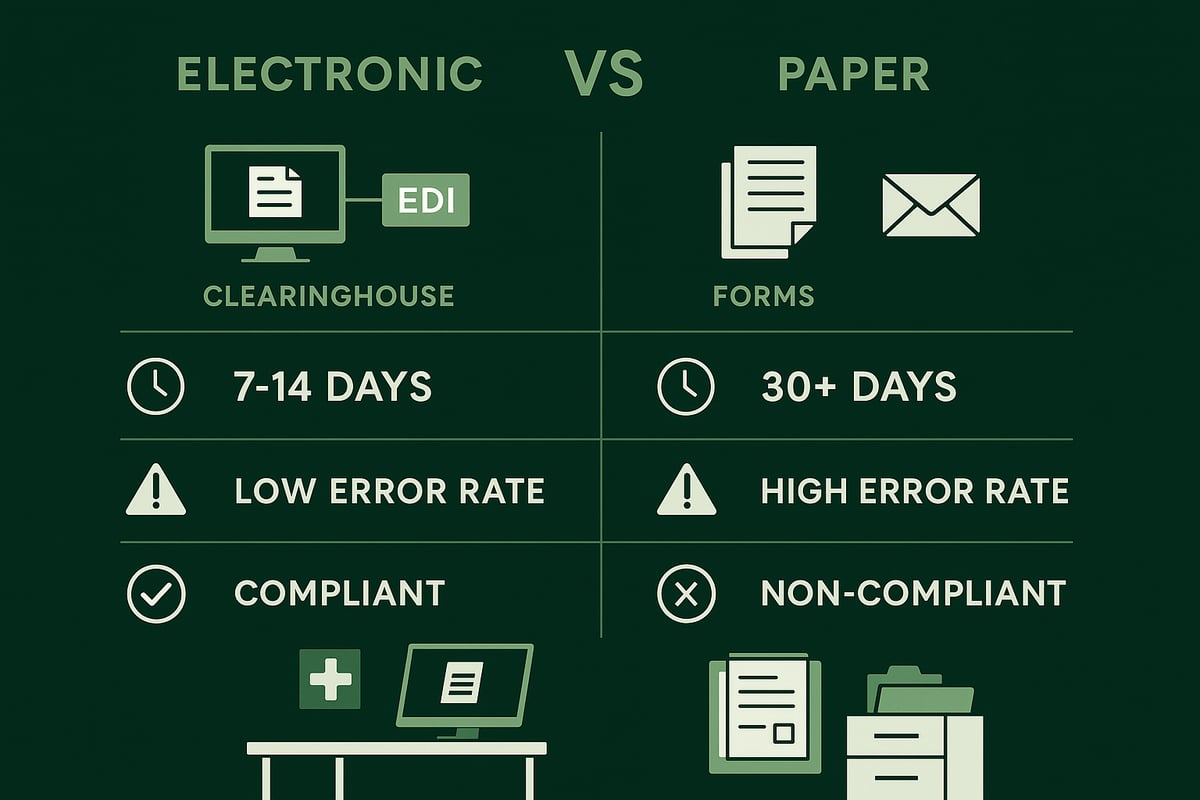
Electronic Claim Submission
Electronic claim submission in medical billing uses EDI (Electronic Data Interchange) to transmit claims through clearinghouses directly to payers. This method is fast, accurate, and now the industry standard for most healthcare organizations. Claims are formatted according to HIPAA’s ANSI X12 837 standard, ensuring compliance and interoperability.
Submitting claims electronically offers multiple advantages. Providers benefit from shorter processing times—claims are often settled in 7 to 14 days compared to over 30 days for paper claims. Real-time tracking and automated error checking reduce administrative burden and improve cash flow. In fact, over 95% of all claim submission in medical billing now occurs electronically, reflecting the industry’s shift toward digital efficiency.
Paper Claim Submission
Paper claim submission in medical billing involves completing and mailing physical forms, such as CMS-1500 or UB-04, directly to payers. While this method is less common today, it remains necessary in certain cases—such as when a payer does not accept EDI, technical issues arise, or specific rural or Medicaid programs require paper documentation.
However, paper claims introduce several disadvantages. Manual handling increases the risk of data entry errors, lost documents, and longer reimbursement cycles. Processing times can stretch beyond 30 days, which delays cash flow for clinics. For organizations striving to optimize claim submission in medical billing, minimizing paper use is essential for operational efficiency.
Comparison and Choosing the Right Method
The decision between electronic and paper claim submission in medical billing should be based on speed, accuracy, compliance, and cost. The following table summarizes key differences:
| Factor | Electronic Submission | Paper Submission |
|---|---|---|
| Processing Time | 7–14 days | 30+ days |
| Error Rate | Low | Higher |
| Compliance | HIPAA ensured | Prone to issues |
| Cost | Lower | Higher (manual labor) |
| Tracking | Real-time | Manual follow-up |
Most practices benefit from transitioning to electronic claim submission in medical billing wherever possible. This not only boosts clean claim rates but also accelerates reimbursement and reduces administrative workload.
Common Reasons for Claim Denials and How to Avoid Them
Accurate claim submission in medical billing is the foundation for consistent cash flow in any healthcare organization. Yet, even with robust processes, denials can disrupt revenue and inflate administrative costs. Understanding why claims get denied, and how to prevent and resolve these issues, is essential for every provider and billing team.
![]()
Top 10 Reasons for Claim Denials
Denials can stem from a variety of sources, but some errors are more common than others in claim submission in medical billing. The following are the top 10 reasons:
- Incorrect or incomplete patient demographics or insurance data
- Claims submitted after payer deadlines
- Coding mismatches between diagnoses and procedures
- Services not covered under the patient’s insurance policy
- Insufficient documentation for medical necessity
- Pre-existing condition exclusions
- Policy expired at the time of service
- Missing or invalid pre-authorization
- Duplicate claims submitted for the same service
- Claims lost or not received by the payer
For a deeper dive into these causes and their financial impact, refer to the Top 5 Reasons Medical Claims Get Denied for additional industry insights.
Strategies to Prevent Denials
Proactive prevention is the most effective approach to minimizing denials from claim submission in medical billing. Consider the following strategies:
- Implement real-time eligibility and insurance verification before services
- Invest in certified coders and schedule routine coding audits
- Stay current on payer guidelines, policy updates, and deadlines
- Utilize automated claim scrubbing to catch errors before submission
- Monitor claim status and respond quickly to rejections
By acting early and standardizing these steps, organizations can significantly reduce preventable denials and accelerate reimbursement.
Handling Denials and Resubmissions
Even with the best processes, some claims will require rework. Efficient denial management is a critical part of claim submission in medical billing. Follow these steps:
- Review all denial codes and payer feedback to pinpoint the root cause
- Correct errors, update documentation, and resubmit claims promptly
- Track each denial and resubmission using structured workflows
- Document all communications with payers for compliance
Implementing a robust denial management in medical billing process allows healthcare businesses to identify patterns, improve future submissions, and maximize recovered revenue.
How Revenue Cycle Management Services Support Clean Claim Submission
Partnering with professional RCM services provides expert support for claim submission in medical billing. RCM teams handle eligibility verification, coding, claim processing, and denial management, ensuring compliance and reducing errors. Practices that leverage RCM solutions typically see a 20–30% drop in denials, faster payments, and higher clean claim rates, all of which drive stronger financial performance.
Best Practices and Compliance in Medical Claim Submission
Staying compliant and following best practices in claim submission in medical billing is essential for organizations seeking to maximize reimbursements and reduce administrative headaches. The right approach ensures every claim moves smoothly from submission to payment, supports regulatory compliance, and protects sensitive patient data.
Staying Current with Coding and Regulatory Changes
For effective claim submission in medical billing, staying updated with the latest coding and regulatory changes is non-negotiable. Annual updates to ICD, CPT, and HCPCS codes can directly affect claim accuracy and compliance. Missing a code update or misunderstanding a payer's new policy can result in rejected claims or compliance risks.
Healthcare organizations should encourage coders and billers to participate in regular training sessions and subscribe to updates from regulatory bodies. For example, the transition from ICD-10 to ICD-11 is on the horizon, and proactive education will help teams avoid costly errors. Establishing a routine for monitoring payer bulletins and regulatory announcements ensures your claim submission in medical billing always reflects current standards.
Ensuring HIPAA Compliance and Data Security
Protecting patient information is central to claim submission in medical billing. Secure, encrypted systems must be used for all claim data, and staff should be trained on privacy and security protocols. Routine risk assessments and audits help identify vulnerabilities before they become compliance violations.
HIPAA violations can lead to significant penalties, sometimes reaching $50,000 per incident. Organizations looking to enhance their security posture may explore advanced solutions, such as Blockchain-Integrated Privacy-Preserving Medical Insurance Claim Processing Using Homomorphic Encryption, to safeguard sensitive data. Robust data security is not just about compliance, it is about building trust with patients and payers.
Performance Monitoring and Analytics
Continuous monitoring is vital for optimizing claim submission in medical billing. By tracking key performance indicators, organizations can quickly spot bottlenecks and areas for improvement. Core metrics include clean claim rate, denial rate, days in accounts receivable, and first-pass resolution rate.
| Metric | Target Benchmark | Impact on Cash Flow |
|---|---|---|
| Clean Claim Rate | >95% | Faster collections |
| Denial Rate | <5% | Fewer reworks |
| Days in A/R | <30 days | Improved liquidity |
| First-Pass Resolution | >90% | Reduced admin time |
Using dashboards and analytics tools provides real-time insights, enabling data-driven decisions that strengthen the claim submission in medical billing process.
Staff Training and Process Standardization
Standardized workflows and continuous staff training are the backbone of efficient claim submission in medical billing. Developing clear checklists for each step minimizes errors and ensures every claim meets payer requirements. Investing in certification and ongoing education fosters a culture of accountability.
For example, organizations that implement standardized processes see up to a 40% reduction in claim submission errors. This approach not only supports compliance but also drives consistent, reliable results.
Now that you understand the key steps to submitting clean claims and the impact this has on your practice’s financial health, you might be wondering how your current billing processes measure up. At Greenhive Billing Solutions, we’ve helped countless healthcare providers improve efficiency, reduce denials, and accelerate reimbursements through tailored, compliant solutions. If you’re ready to see where you stand and identify opportunities for improvement, why not take the next step? You can uncover hidden revenue and streamline your operations by taking advantage of a Claim Billing Free Audit. Let’s work together to set your practice up for lasting success.