Navigating the evolving landscape of healthcare billing is more complex than ever. Practices face mounting financial pressures and shifting regulatory landscapes, prompting many to question if their processes are truly prepared for what lies ahead.
This comprehensive guide delivers essential insights and actionable strategies, designed specifically for healthcare professionals and organizations seeking to optimize their billing health. Understanding the fundamentals, staying ahead of new regulations, and leveraging emerging technology trends are now vital for sustained success.
Recent changes in payer requirements and rising patient expectations have made billing cycles more intricate. Yet, with the right knowledge, clarity and efficiency become attainable goals.
Apply the insights from this guide to streamline your billing processes and support a healthier, more resilient revenue cycle for your practice.
The Foundations of Healthcare Billing
Building a strong foundation in billing health processes is essential for any healthcare organization aiming to streamline revenue and maintain compliance. Understanding each step, from patient intake to reconciliation, sets the stage for successful outcomes. Mastery of terminology, billing types, and regulatory requirements is what separates efficient operations from costly errors.
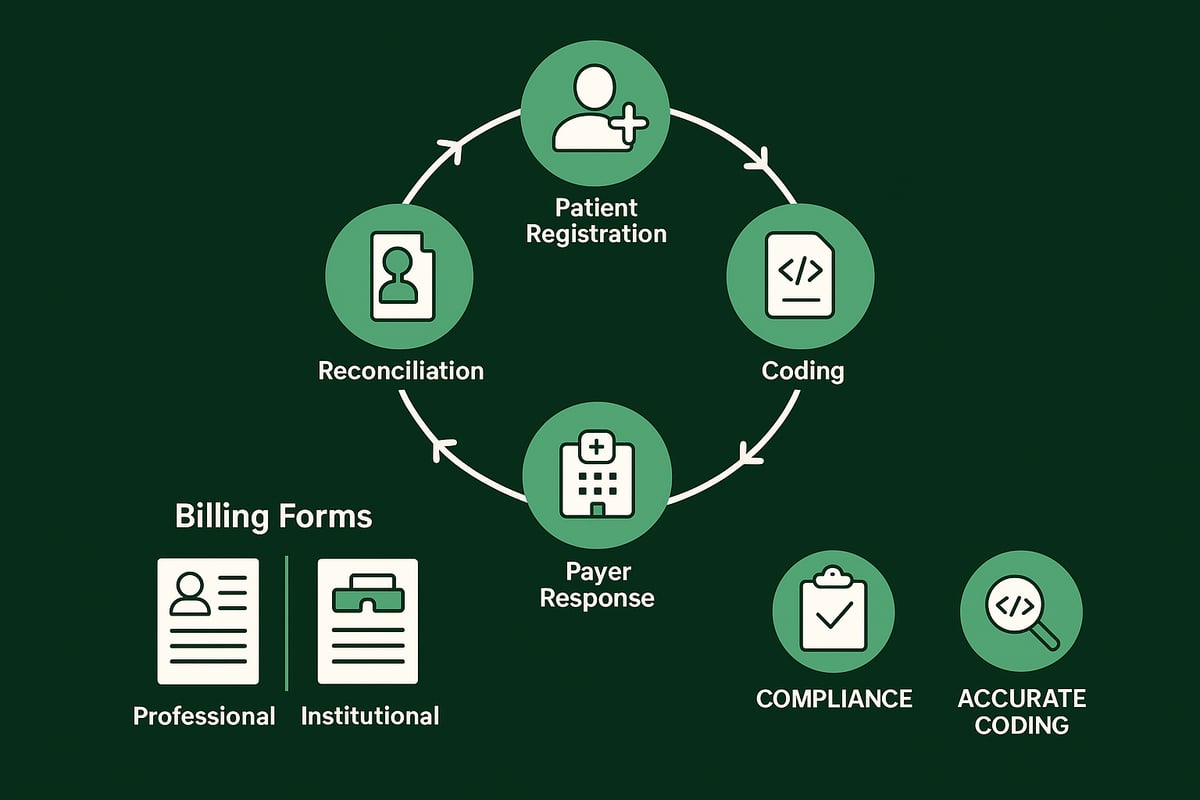
Key Components of the Billing Cycle
At the heart of billing health lies the revenue cycle, encompassing every step from patient registration through to final payment. Accurate collection of demographic and insurance data during registration forms the backbone of this process. Each detail, such as policy numbers and payer information, is critical to prevent downstream issues.
Once data is collected, charge entry and coding translate clinical care into billable services. Claims are then submitted, either electronically or on paper, before payment posting and careful account reconciliation. Even a single error, like a missing insurance digit, can trigger claim denial and slow down reimbursements. For a comprehensive overview, see The Revenue Cycle in Healthcare.
Types of Medical Billing: Professional vs. Institutional
Within billing health operations, understanding the distinction between professional and institutional billing is vital. Professional billing, often using the CMS 1500 form, is typically managed by individual providers or physician groups. Institutional billing, submitted on the UB 04 form, is used by hospitals and larger clinics.
This difference impacts coding, reimbursement processes, and regulatory compliance. For example, a multi-specialty group might need to generate both types of claims depending on the services rendered. Knowing which form to use for each encounter ensures correct payment and reduces compliance risk.
Common Billing Terminology and Codes
A solid grasp of billing health terminology and coding systems is fundamental. The main coding sets include ICD for diagnoses, CPT for procedures, and HCPCS for supplies and services. Key terms such as copay, deductible, coinsurance, EOB, and denial are used throughout the billing process.
| Term | Definition |
|---|---|
| Copay | Fixed fee paid by patient at visit |
| Deductible | Amount patient pays before insurance pays |
| EOB | Explanation of Benefits from payer |
Accuracy is non negotiable. An incorrect CPT code can result in rejected claims or even trigger audits, affecting both revenue and compliance.
The Role of Compliance in Billing Practices
Compliance is the cornerstone of billing health success. HIPAA regulations mandate strict patient data privacy and security throughout the billing process. Recent laws like the No Surprises Act require transparent billing and clear disclosures to patients.
Legal risks for non compliance include fines, audits, and reputational harm. For example, failure to provide mandated billing disclosures can result in penalties under federal law. Regular internal audits and staff training help safeguard against these risks, ensuring the practice remains both profitable and compliant.
Step-by-Step: The Modern Medical Billing Process
Navigating the modern billing health process requires a methodical approach, combining industry expertise with attention to detail. Each step—from patient intake to final collections—plays a critical role in the financial success of healthcare organizations. Let us break down the key components of a robust billing health workflow.
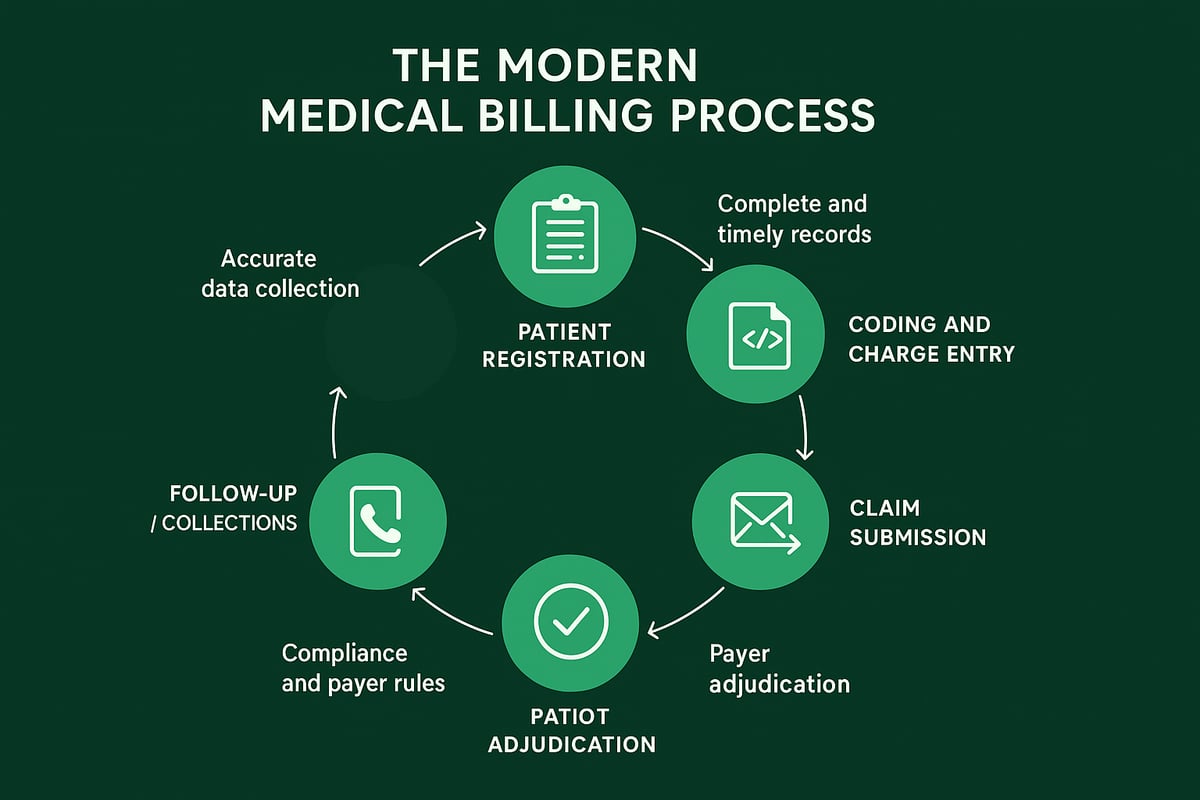
Step 1: Patient Registration and Insurance Verification
The first step in billing health is collecting accurate patient demographics and insurance details. Front-desk teams must verify eligibility and coverage before services are rendered. This includes confirming policy status, checking for outstanding balances, and identifying prior authorization requirements.
Digital forms and EHR integrations help reduce manual errors, ensuring clean data entry. Missing or incorrect information can lead to denials, impacting billing health and delaying revenue. A proactive approach at registration sets the stage for a smooth revenue cycle.
Consider using a checklist for staff to consistently capture all required information. This minimizes rework and supports downstream processes.
Step 2: Documentation of Patient Encounter
Accurate clinical documentation is foundational to billing health. Providers should thoroughly record symptoms, diagnoses, and all procedures performed during each encounter. These notes are not only vital for care continuity but also directly inform coding and billing.
Incomplete or vague documentation can cause delays or claim rejections. Establishing documentation standards for your team helps ensure every necessary detail is captured. Audit trails within EHR systems further support compliance and streamline the audit process.
Timely, clear documentation safeguards both revenue and compliance, reinforcing strong billing health for your practice.
Step 3: Medical Coding and Charge Entry
Translating clinical notes into standardized codes is a critical part of billing health. Coders assign ICD, CPT, and HCPCS codes based on documentation, ensuring every service and supply is accurately captured. Charge entry specialists then input these codes into the system, forming the basis for claims.
Coding accuracy is essential for compliance and optimal reimbursement. Both upcoding and downcoding can trigger payer scrutiny or audits. Regular coder training and double-check systems reduce risks.
A structured workflow for coding and charge entry supports consistent billing health, minimizing errors and maximizing revenue.
Step 4: Claim Creation and Submission
Once codes and charges are finalized, claims are prepared using standardized forms like CMS 1500 or UB 04. The use of electronic submission, rather than paper, speeds up processing and reduces common errors in billing health workflows.
Clearinghouses play a key role by scrubbing claims for completeness and accuracy before submission to payers. This extra validation step decreases the likelihood of denials.
Timely and accurate claim submission drives faster payment cycles. Leveraging electronic tools and experienced service providers ensures your billing health process remains efficient and reliable.
Step 5: Adjudication and Payer Response
After submission, insurers review claims for medical necessity and policy compliance. They issue an Explanation of Benefits (EOB) and remittance advice, detailing approved payments and any reductions.
Common denial reasons include missing preauthorizations or insufficient documentation. Understanding payer criteria is vital for maintaining healthy billing health outcomes.
Reviewing payer responses promptly allows staff to address issues before revenue is lost. A systematic approach to tracking remittances and denials keeps your organization financially agile.
Step 6: Patient Billing and Financial Communication
When balances remain after insurance payments, clear and timely patient billing is essential for effective billing health. Statements should outline charges, due dates, and available payment options.
Providing transparent communication reduces confusion and improves patient satisfaction. Offering online payment portals or flexible plans increases collection rates and supports financial engagement.
Staff should be trained to handle questions and set up payment arrangements as needed. Strong patient communication practices are a hallmark of successful billing health strategies.
Step 7: Follow-Up, Appeals, and Collections
The final step in the billing health process involves rigorous follow-up on unpaid or denied claims. Investigating denial reasons and submitting timely appeals are critical for revenue recovery. Automated reminders and tracking systems boost efficiency in collections.
For advanced tips on optimizing this stage, refer to Denial Management Strategies, which explores proven methods that strengthen cash flow and billing health.
Ethical collections practices and regular follow-up keep your revenue cycle healthy, ensuring sustainable financial performance for your organization.
Navigating New Regulations and Compliance Standards
Staying ahead of new regulations is essential for maintaining a healthy billing health strategy. Regulatory shifts impact every stage of the revenue cycle, from data security to patient communication. Let us explore the critical standards shaping compliance today.
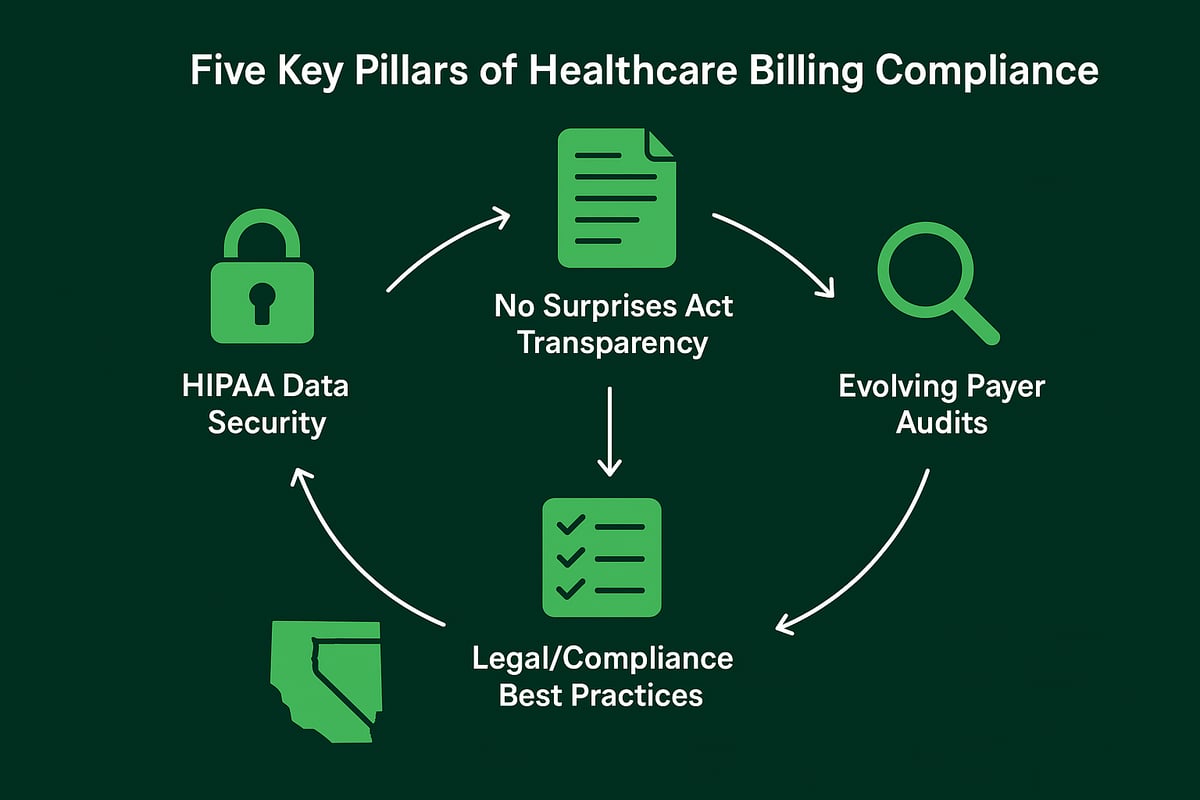
HIPAA and Patient Data Security
Protecting patient information is foundational for billing health. HIPAA regulations require secure handling of all patient data, including billing records. Practices must ensure encryption, access controls, and secure data transmission.
A breach can result in severe penalties and loss of trust. Common safeguards include multi-factor authentication, role-based access, and regular staff training. Service providers should always verify that client-owned software meets HIPAA standards.
For example, encrypted billing systems and restricted system access help prevent unauthorized data exposure.
The No Surprises Act and Price Transparency
Billing health now depends on transparent patient communications. The No Surprises Act protects patients from unexpected out-of-network charges. Providers must deliver clear cost estimates and Good Faith Estimates before non-emergency services.
Key requirements:
- Inform patients of network status and potential costs
- Provide written estimates for scheduled procedures
- Update workflows to document disclosures
Practices that communicate openly about costs and coverage reduce patient confusion and foster trust. For instance, offering cost estimates before elective procedures aligns with both compliance and patient satisfaction.
Evolving Payer Policies and Audit Trends
As payer requirements evolve, so must your billing health protocols. Payers increasingly demand thorough documentation and precise coding. Pre-payment reviews and audits are more common, with denials issued for insufficient medical necessity documentation.
To stay current:
- Monitor payer bulletins and updates
- Review claim requirements regularly
- Train staff on new coding and reporting standards
For more on coding essentials, see Understanding Medical Coding Types. Proactive management of payer expectations helps prevent denials and optimize revenue.
Legal Risks and Best Practices for Compliance
Legal risks can undermine billing health if not addressed proactively. Fraudulent or inaccurate billing can trigger audits, fines, and reputational harm. Establishing internal audits and compliance checklists is vital.
Best practices include:
- Ongoing staff education on legal requirements
- Routine internal reviews of billing processes
- Clear documentation of all billing actions
For example, regular compliance training sessions reduce the likelihood of costly violations and keep staff up to date on changing regulations.
The Impact of State-Specific Laws and Regional Variations
State regulations add another layer to billing health management. Medicaid rules, allowable charges, and transparency mandates often differ by region. Staying informed about both federal and state updates is critical.
Comparing State vs Federal Billing Requirements:
| Requirement | Federal Standard | State Variations |
|---|---|---|
| Price Transparency | Required by No Surprises | Additional disclosures |
| Facility Fees | Regulated for Medicare | Varies by state |
| Balance Billing | Restricted in many cases | Some allow/limit |
For instance, certain states mandate specific billing disclosures or limit facility fees. Regularly reviewing regional updates ensures compliance and protects revenue.
Technology and Innovation in Healthcare Billing
Modern billing health strategies depend on technology innovation to drive efficiency, compliance, and patient satisfaction. As practices face new challenges, leveraging digital tools is essential for optimizing workflows and staying ahead in a competitive landscape.
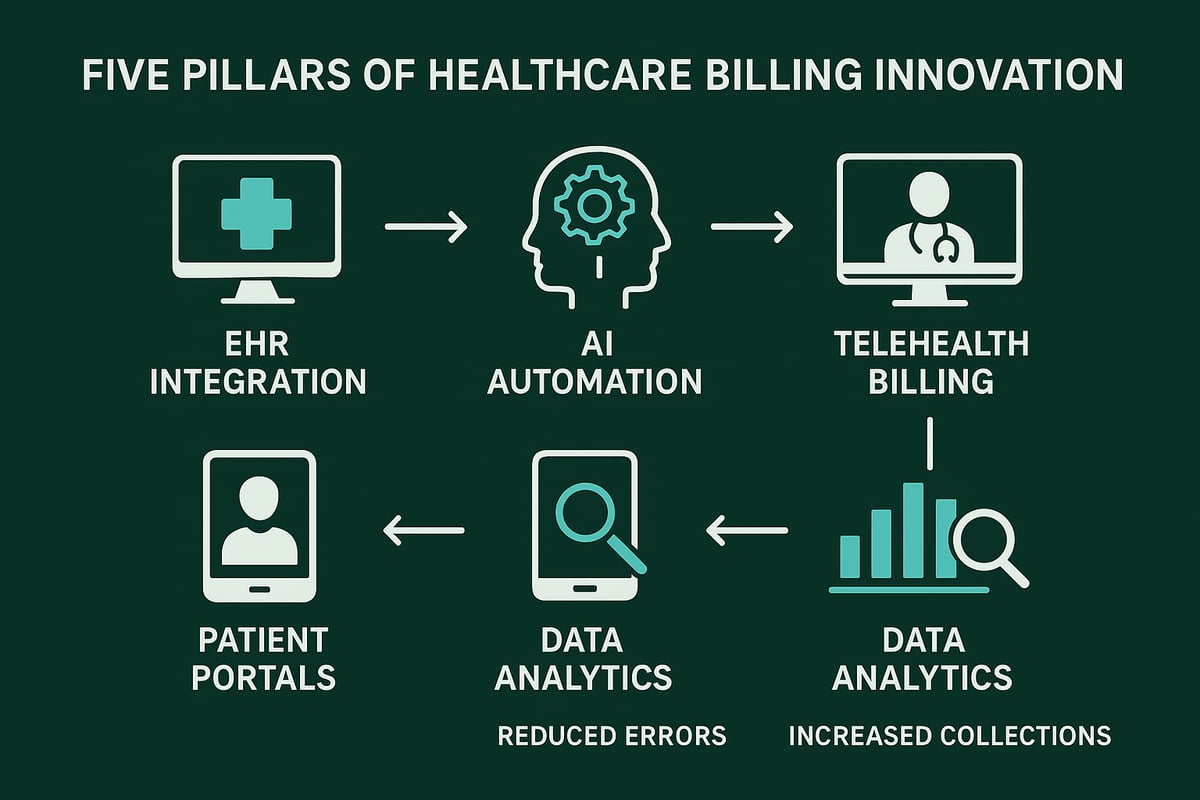
The Shift to Electronic Health Records (EHR) and Digital Billing
Integrating EHR platforms with billing health processes has revolutionized the revenue cycle for healthcare organizations. Seamless data flow between clinical and financial systems reduces manual entry errors and accelerates claim submission.
Automated eligibility checks verify insurance in real time, while digital charge capture ensures every billable service is documented. Practices using EHR-linked billing health solutions see fewer denials and faster payments.
For a closer look at how EHR integration and automation are shaping the future, see EHR and Medical Billing Trends 2026.
Artificial Intelligence and Automation in Billing
Artificial intelligence is transforming billing health management by automating repetitive tasks and enhancing accuracy. AI-powered claim scrubbing tools flag inconsistencies and missing data before submission, reducing the risk of denials.
Machine learning algorithms can predict which claims are likely to be denied, allowing proactive corrections. Automation streamlines workflows, from eligibility verification to payment posting, freeing staff to focus on complex cases.
Key benefits of AI in billing health include:
- Faster claim processing
- Lower administrative costs
- Improved compliance and audit readiness
Telehealth Billing: Opportunities and Challenges
The rise of telehealth has introduced new dimensions to billing health operations. Virtual visits require precise coding and careful attention to payer policies, as some insurers do not reimburse facility fees for remote consults.
Billing health professionals must stay updated on evolving telehealth regulations, including documentation standards and allowable charges. Adapting billing workflows to accommodate telehealth ensures providers capture every eligible dollar.
A best practice is to create clear guidelines for telehealth billing health processes, ensuring compliance and maximizing reimbursement.
Enhancing Patient Financial Experience with Technology
Technology-driven billing health strategies improve patient satisfaction and collections. Online patient portals allow patients to review statements, pay bills, and access cost estimates anytime.
Transparent, easy-to-understand statements build trust and reduce confusion. Digital payment options, including payment plans, address financial barriers and encourage timely payments.
Practices that prioritize the digital patient experience in billing health often see higher satisfaction scores and lower rates of unpaid balances.
Data Analytics for Revenue Cycle Optimization
Data analytics is now a cornerstone of billing health optimization. Advanced dashboards track key performance indicators such as days in accounts receivable, denial rates, and collection efficiency.
By analyzing trends and identifying bottlenecks, practices can implement targeted improvements. For example, a spike in denials for a specific code can trigger training or process changes.
Effective use of analytics in billing health empowers organizations to make data-driven decisions, strengthening financial outcomes and supporting long-term growth.
Key Challenges and Solutions in Healthcare Billing
Healthcare organizations face a dynamic landscape where billing health processes are continually tested by evolving regulations, payer demands, and rising patient expectations. Addressing these challenges head-on is essential to protect revenue and maintain compliance. Below, we break down common obstacles and proven strategies to help streamline your billing health operations.
Common Billing Errors and How to Prevent Them
Billing health can be undermined by frequent mistakes such as incorrect patient data, errors in coding, or missing authorizations. These errors not only delay payments but can also trigger audits and create compliance risks.
To combat these issues, implement robust staff training, double-check systems, and leverage technology to automate error-prone steps. Real-time eligibility verification and coding validation tools are crucial for reducing denials. For a deeper dive into typical mistakes and their remedies, see Common Medical Billing Errors.
Accurate processes in billing health will keep your revenue cycle on track and minimize costly disruptions.
Managing Denials and Appeals Effectively
Denials are inevitable in billing health, but they don't have to be a permanent loss. Understanding denial reasons and analyzing patterns is the first step toward improvement.
Develop standardized appeal processes and track success rates to measure performance. Timely follow-up on denied claims can recover significant revenue. Use dashboards to monitor appeal turnaround times and identify recurring payer issues.
By prioritizing denial management, your practice can turn setbacks into learning opportunities and safeguard billing health.
Coping with Changing Payer Requirements
Payer requirements are constantly changing, impacting billing health every step of the way. Adapting to new documentation standards and reimbursement policies is a continuous challenge.
Maintain updated payer contact information and subscribe to regular policy bulletins. Schedule team meetings to review recent changes and share insights. Proactive adaptation prevents unexpected denials and keeps your billing health resilient.
Regular communication with payers and staying informed are the best lines of defense against shifting requirements.
Balancing Patient Satisfaction and Revenue Goals
Balancing financial objectives with patient satisfaction is a key element of billing health. Patients expect clear communication regarding their financial responsibility and flexible payment options.
Offer simplified statements and financial counseling to help patients understand charges and payment plans. Practices that prioritize patient-centric billing health strategies see improved collection rates and fewer unpaid balances.
Transparent and supportive communication not only boosts revenue but also strengthens patient trust.
Staffing, Training, and Outsourcing Considerations
A skilled team is the backbone of effective billing health. Regular training ensures staff stay updated on regulations and payer guidelines. However, high claim volumes or limited resources may prompt practices to consider outsourcing.
Outsourcing can offer cost savings and improved collections, especially when partnering with experienced RCM service providers. The Medical Billing Outsourcing Market Growth highlights this trend, showing how organizations leverage external expertise to optimize billing health.
Ultimately, the right combination of internal skill development and strategic outsourcing will support financial performance and compliance.
Healthcare Billing Best Practices for Financial Health
Optimizing billing health is crucial for every healthcare organization aiming to maintain financial stability and compliance. By focusing on strategic best practices, practices can enhance revenue cycle performance, minimize risk, and deliver a better experience for both patients and staff.
Proactive Revenue Cycle Management
Effective billing health starts with proactive revenue cycle management. Monitoring every step, from patient intake to final payment, helps identify bottlenecks before they impact cash flow.
Teams should review KPIs such as days in accounts receivable, denial rates, and collection percentages monthly. Early detection of trends allows for timely adjustments and prevents revenue leakage.
For example, a practice that regularly reviews its metrics can spot a rise in claim denials quickly and implement corrective action. This approach ensures that billing health remains robust and responsive to changing payer requirements.
Patient-Centric Billing Strategies
Placing patients at the center of billing health initiatives leads to improved satisfaction and payment rates. Clear, concise billing statements and transparent pricing reduce confusion and build trust.
Leveraging technology, such as digital portals, enables patients to view balances, set up payment plans, and access cost estimates with ease. This transparency empowers patients and streamlines collections.
For instance, practices that offer online payment options report fewer unpaid balances and higher overall engagement. A patient-centric approach directly contributes to stronger billing health by making payment processes more accessible.
Regular Compliance Audits and Staff Training
Sustaining billing health depends on consistent compliance audits and ongoing staff education. Internal audits catch errors before claims are submitted, reducing the risk of denials and regulatory penalties.
Staff should receive quarterly training on evolving payer guidelines and new regulations. This proactive investment keeps teams informed and prepared to handle complex billing scenarios.
A practice that prioritizes staff development and routine audits demonstrates a commitment to both compliance and billing health, lowering the likelihood of costly mistakes and improving long-term outcomes.
Leveraging Industry Partnerships and Expert Support
Partnering with experienced revenue cycle management providers brings specialized expertise to your billing health strategy. These partnerships enable access to advanced analytics, best practices, and up-to-date regulatory knowledge.
Collaborating with industry experts can lead to improved collections, better compliance, and measurable cost savings. According to the Healthcare Sector Outlook 2026, organizations that focus on benefit cost containment and strategic alliances are better positioned for financial resilience.
Practices that integrate external RCM support into their billing health initiatives often achieve more efficient workflows and a stronger bottom line.
As you navigate the growing complexities of healthcare billing, staying informed and proactive is the key to financial health. With evolving regulations, technology shifts, and increasing payer demands, even the most diligent practices can miss hidden inefficiencies or compliance risks. That is where a second set of expert eyes makes all the difference. If you are curious about how your billing processes measure up or want to ensure you are positioned for success in 2026, let us help. Take the next step and Get Your Free Audit—you deserve clarity, confidence, and peace of mind for your practice’s future.