Revenue cycle management is becoming more complex every year for healthcare organizations. With rising regulatory demands and payer requirements, the need to improve revenue cycle management has never been greater.
Revenue leakage, claim denials, and frequent rule changes can all have a substantial impact on your financial performance. Fortunately, proven strategies exist to streamline processes, increase collections, and enhance overall profitability.
In this article, we outline seven actionable, evidence-based ways to improve revenue cycle management. You will find practical examples and recent data for each approach, including:
- Optimizing patient access and eligibility verification
- Standardizing and streamlining claims submission
- Enhancing denial management and appeals
- Improving patient payment collections and communication
- Leveraging data analytics and reporting
- Investing in staff training and collaboration
- Embracing automation and technology integration
Understanding the Revenue Cycle Management Landscape
Revenue cycle management is the backbone of financial health for healthcare organizations. As the industry evolves, the pressure to improve revenue cycle management grows, impacting everything from operational efficiency to profitability.
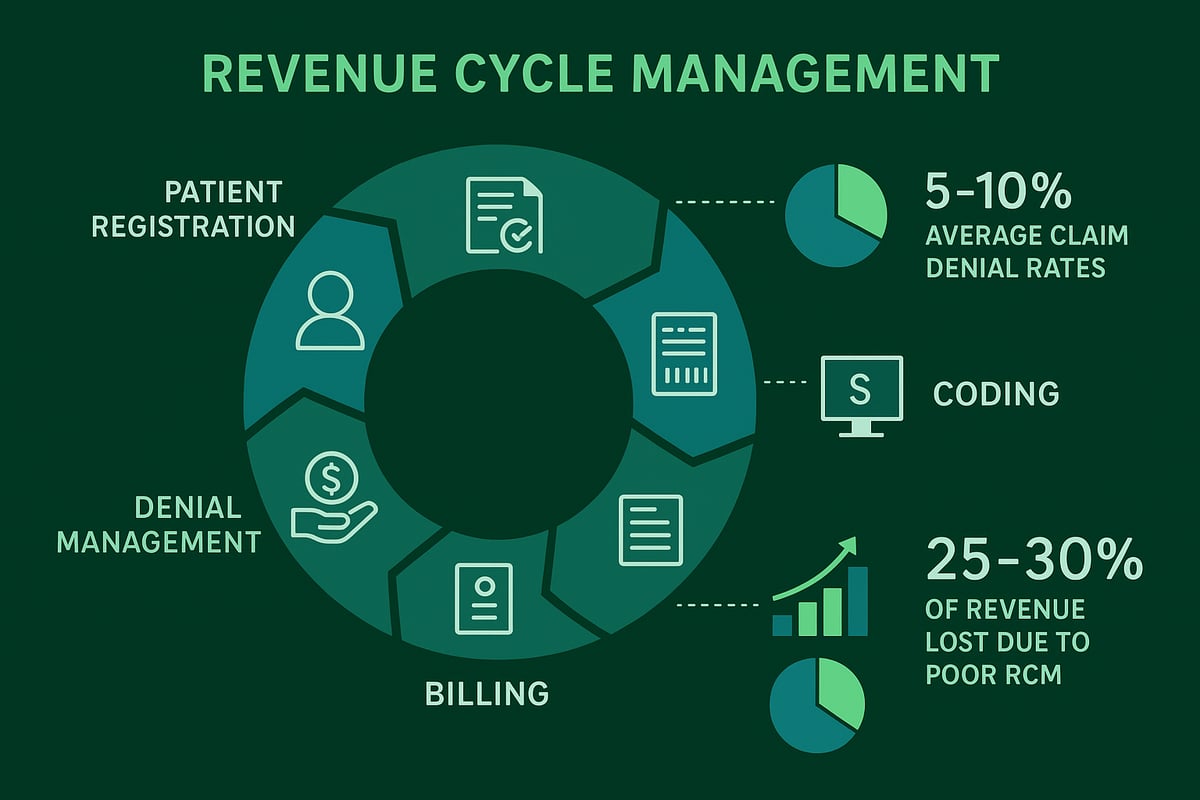
The revenue cycle begins with patient registration and continues through eligibility verification, coding, billing, collections, and denial management. Each step must be executed with precision to optimize cash flow and reduce financial risk. For a more detailed breakdown of these processes, see this Revenue cycle medical billing overview.
When organizations fail to improve revenue cycle management, the financial consequences are immediate. Industry data shows average claim denial rates between 5% and 10%. Each denial costs time and money to rework, with the average claim resubmission costing up to $25 per claim. Studies reveal that poor RCM processes can cause healthcare providers to lose up to 3% of net revenue annually. These losses compound quickly, affecting investments in patient care, staffing, and technology upgrades.
Providers face a range of challenges in their efforts to improve revenue cycle management. Constant changes in payer rules and reimbursement policies demand ongoing vigilance. Staffing shortages, especially in billing and coding departments, can lead to backlogs and errors. Integrating new technology with existing systems is another hurdle, as organizations strive for seamless data exchange and process automation. Compliance with evolving payer requirements is non-negotiable, with regulatory penalties posing significant risks.
Consider a breakdown in eligibility verification. If staff miss an insurance coverage issue at registration, the error ripples through the entire revenue cycle. The result is a denied claim, delayed payment, and increased workload for staff tasked with appeals. This single misstep can undermine even the best efforts to improve revenue cycle management.
Continuous process improvement and regular staff training are essential. Investing in education and feedback loops ensures teams stay current with payer policies, coding updates, and compliance standards. In today's complex healthcare environment, a proactive approach is the only way to sustainably improve revenue cycle management.
7 Proven Ways To Improve Revenue Cycle Management
Healthcare organizations aiming to improve revenue cycle management must address every stage, from patient access to collections and data analytics. The following strategies provide actionable steps to streamline operations, reduce denials, and maximize collections. Each method is supported by real-world examples, industry data, and proven best practices.
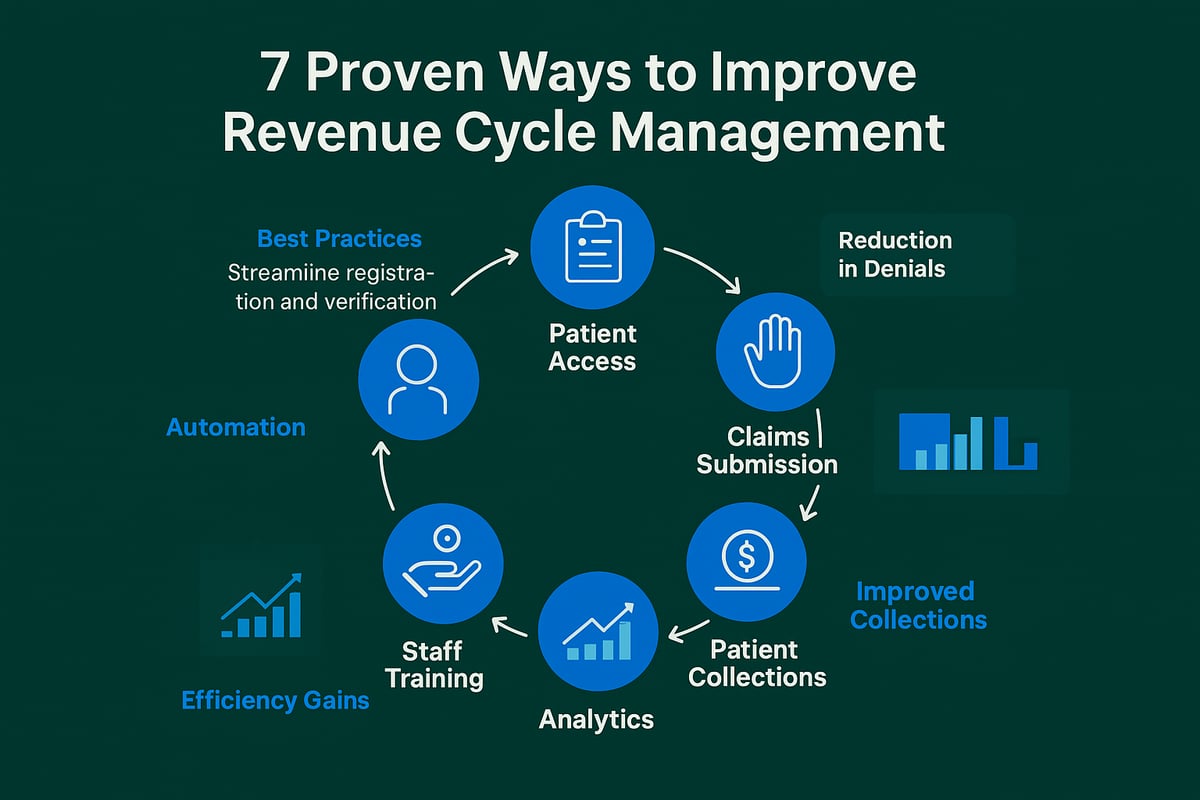
1. Optimize Patient Access and Eligibility Verification
Accurate patient access is the foundation to improve revenue cycle management. Collecting correct demographic and insurance data upfront prevents downstream errors and delays.
Best practices include verifying insurance eligibility before each service. Automated tools can confirm coverage in real time, reducing manual errors. Staff should be trained to spot common data entry mistakes.
Missed or incorrect eligibility checks often lead to increased denials and payment delays. For example, a clinic that adopted real-time eligibility verification saw denials drop by 25 percent within three months. Ongoing audits and process improvement ensure sustained accuracy.
Eligibility verification is widely recognized as a core RCM step. Leveraging insurance verification best practices helps prevent missed authorizations and coverage lapses, strengthening financial outcomes.
Regularly reviewing and refining patient access workflows is essential for organizations that want to improve revenue cycle management.
2. Standardize and Streamline Claims Submission Processes
Submitting clean claims on the first attempt is critical to improve revenue cycle management. Standardized workflows for charge capture and claim creation help minimize errors and rework.
Proper coding and comprehensive documentation prevent mistakes that can trigger denials. Technology solutions reduce manual data entry, which is a common source of billing errors. On average, coding errors account for a significant portion of denied claims, often due to inconsistent processes.
Routine audits and feedback loops help teams identify and correct recurring issues. A group practice that standardized its charge capture process reported a 15 percent increase in first-pass resolution rates, leading to faster payments.
Establishing clear protocols for claims submission, supported by regular training and performance reviews, creates a culture of accountability. With these measures, organizations are positioned to improve revenue cycle management and achieve more predictable cash flow.
3. Enhance Denial Management and Appeals
Denial management is a pivotal area to improve revenue cycle management. Common denial reasons include coding errors, missing documentation, or eligibility issues. Unresolved denials represent lost revenue and unnecessary administrative work.
Implementing a dedicated denial management workflow allows for efficient root cause analysis and trend tracking. Timely follow-up and appeals are essential, as industry data shows that up to 60 percent of denied claims are recoverable with proper action.
A structured approach—documenting denial reasons, tracking appeal outcomes, and refining processes—can significantly improve revenue recovery. For example, one clinic increased collections by 18 percent after implementing a formal denial management protocol.
For detailed strategies, see denial management in medical billing. Proactive denial management empowers organizations to improve revenue cycle management and protect their bottom line.
4. Improve Patient Payment Collections and Financial Communication
Patient responsibility now accounts for a larger share of healthcare revenue, making clear communication and flexible payment options essential to improve revenue cycle management.
Clear, upfront discussions about costs, insurance coverage, and payment options reduce confusion and increase collections. Offering multiple payment channels—such as online portals, mobile apps, and in-person payments—caters to patient preferences.
Implementing payment plans and collecting copays or deductibles before service can boost cash flow. Data shows that patient-friendly billing increases collection rates by 15–20 percent. For example, practices introducing digital payment reminders have reported a significant uptick in timely payments.
Staff should be trained in financial conversations to ensure a positive patient experience. By focusing on communication and convenience, healthcare organizations can improve revenue cycle management and reduce bad debt.
5. Leverage Data Analytics and Performance Reporting
Data-driven decision-making is essential to improve revenue cycle management. Tracking key RCM metrics—such as days in A R, denial rates, and collection rates—provides insight into process bottlenecks and areas for improvement.
Dashboards and regular reporting offer transparency and enable teams to monitor progress. Industry leaders use real-time analytics to identify trends and intervene early, preventing revenue loss. Benchmarking against industry standards helps set realistic targets.
For a deeper dive, explore healthcare revenue cycle analytics to see how analytics transform collections and efficiency. For example, one group used analytics to reduce their average days in A R by 10 days within six months.
Encouraging a data-driven culture allows organizations to continually improve revenue cycle management and achieve measurable financial gains.
6. Invest in Staff Training and Cross-Department Collaboration
Skilled staff are vital to improve revenue cycle management. Regular training on coding updates, payer rules, and compliance reduces errors and keeps teams current with industry changes.
Cross-department collaboration between front desk, billing, and clinical teams ensures information flows smoothly. Data indicates that high staff engagement lowers billing errors and reduces turnover, supporting long-term organizational health.
Standardized training modules and frequent workshops help maintain consistency. For instance, a practice that launched quarterly RCM training saw a 12 percent drop in claim rejections.
Encouraging feedback and continuous learning empowers staff to adapt and excel. By investing in people and collaboration, organizations can improve revenue cycle management and drive sustained success.
7. Embrace Automation and Technology Integration
Automation is a strategic lever to improve revenue cycle management. Automated workflows reduce manual errors and free staff to focus on higher-value tasks.
Integrating EHR, billing, and clearinghouse platforms ensures seamless data flow and eliminates duplicate entry. Automated tools can handle eligibility checks, claim scrubbing, and payment posting, increasing speed and accuracy.
Industry studies show that automation can reduce claim denials by up to 30 percent and cut processing time by half. A multi-specialty group practice achieved a 20 percent ROI in the first year after automating core RCM functions.
Organizations should evaluate technology regularly and plan for change management to support staff adoption. By embracing automation, healthcare providers position themselves to improve revenue cycle management and remain competitive in a dynamic market.
The Role of Professional RCM Service Providers
Outsourcing to professional RCM service providers has become a strategic move for many healthcare organizations seeking to improve revenue cycle management. With the increasing complexity of billing, coding, and payer requirements, leveraging external expertise can help organizations stay competitive and maintain financial health.
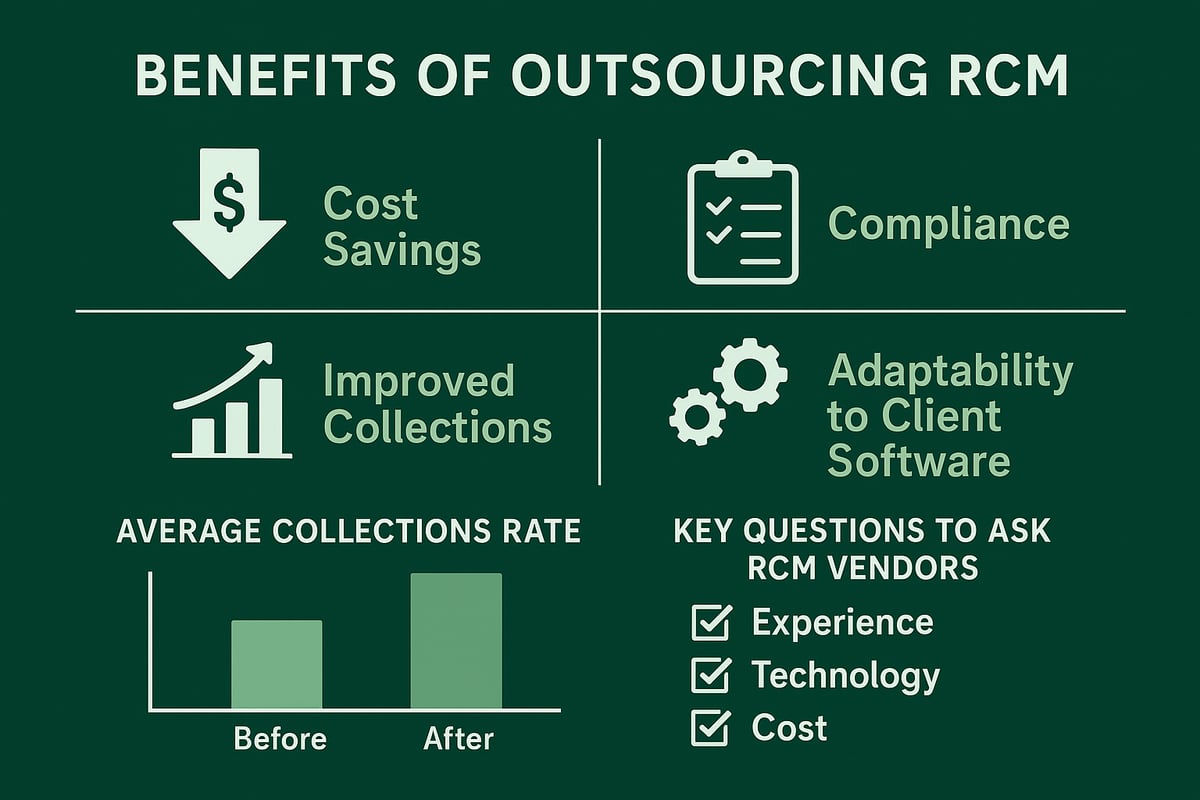
Partnering with a specialized provider brings measurable advantages. Expert RCM teams manage complex billing, coding, and denial processes efficiently, reducing administrative burdens on your staff. According to the U.S. Revenue Cycle Management Market Report 2025, organizations that outsource can achieve significant cost savings while also increasing collections and ensuring ongoing compliance. These improvements directly contribute to efforts to improve revenue cycle management and operational efficiency.
Service providers adapt to client-owned software and established workflows, ensuring a seamless transition and minimal disruption. For example, a midsize clinic saw a 20% boost in collections and faster cash flow after collaborating with an experienced RCM team, demonstrating how outsourcing can improve revenue cycle management in practice.
When evaluating RCM vendors, prioritize transparency, compliance expertise, and relevant specialty experience. Ask critical questions about data security, reporting practices, and adaptability to your organization’s needs. The right partner will support your goals and help drive long-term financial performance.
As you’ve seen, improving your revenue cycle management isn’t just about fixing one step—it’s about building a seamless, efficient system that truly supports your practice’s financial health. Whether you’re looking to reduce claim denials, streamline your billing processes, or leverage the latest technology, every improvement brings you closer to maximizing your reimbursements. If you’re ready to take a closer look at where your RCM stands today and find actionable ways to boost your results, let’s connect. You can Get Your Free Audit and discover how Greenhive Billing Solutions can help you thrive in 2026 and beyond.

