The future of healthcare belongs to organizations that master health management solutions. As demands rise and regulations shift, the need for effective strategies becomes urgent for every healthcare leader aiming to stay competitive.
This guide is designed for healthcare professionals, clinics, and organizations seeking to optimize care delivery and streamline operations. You’ll discover actionable insights to reduce costs, improve patient outcomes, and achieve lasting operational excellence.
We’ll explore the latest trends, core solution categories, step-by-step implementation, compliance essentials, and emerging innovations. Ready to lead your organization with confidence? Let’s unlock the next level of performance together.
Understanding Health Management Solutions: Key Concepts and Benefits
Health management solutions are comprehensive strategies and services designed to optimize healthcare delivery, cost control, and compliance for organizations. In a B2B context, these solutions support clinics, hospitals, and practitioners by streamlining processes and improving outcomes.
What Are Health Management Solutions?
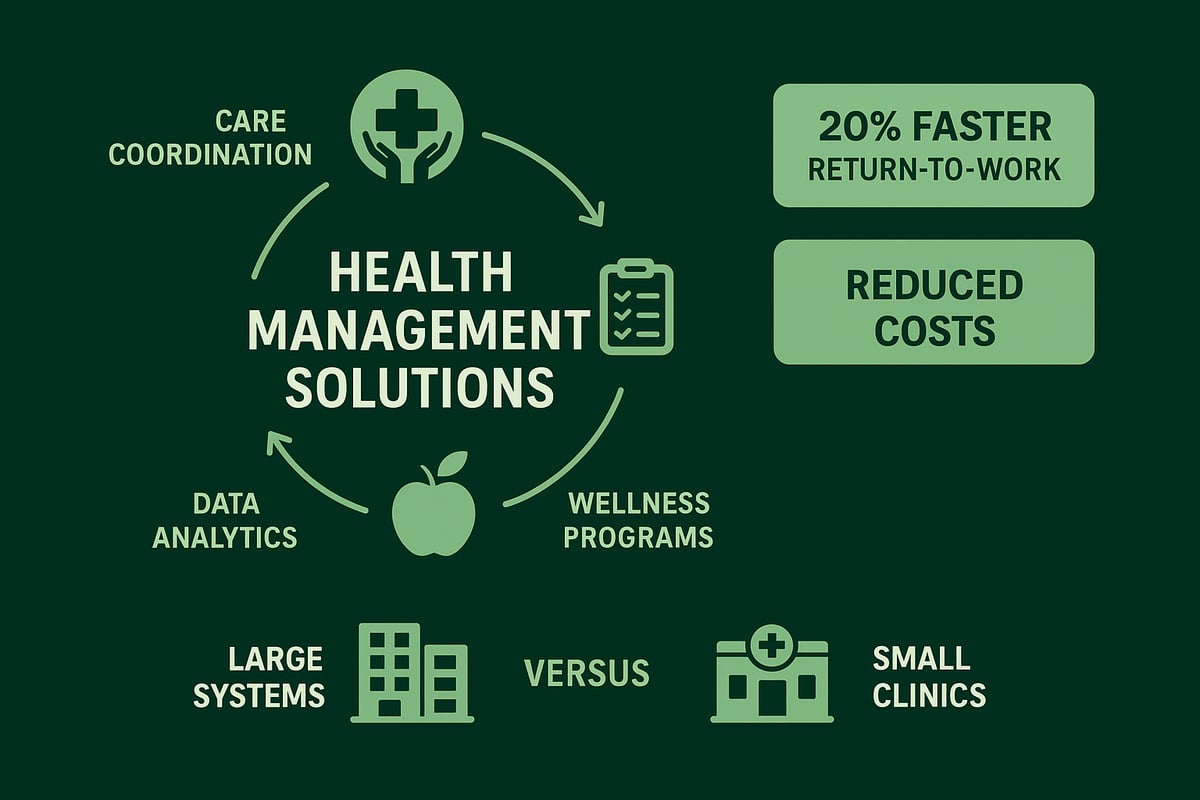
At their core, health management solutions include care coordination, claims management, wellness programs, and data analytics. These elements work together to create a seamless experience for both providers and patients. For example, managed care organizations help employers and clinics navigate claims while supporting better patient care.
Key Components in Practice
Typical components include:
- Care coordination to connect providers and patients
- Claims management for efficient billing and reimbursement
- Wellness programs that promote preventive care
- Analytics platforms for measuring outcomes and ROI
To learn more about claims and revenue optimization, explore revenue management solutions in healthcare.
Major Benefits for Healthcare Organizations
Organizations using health management solutions often see improved patient outcomes, reduced costs, and greater operational efficiency. Studies show that managed care can lead to a 20 percent faster return-to-work rate for employees. Regulatory compliance is also streamlined, supporting safer, more reliable care.
Adaptability Across Organizations
These solutions are scalable, serving both large health systems and specialized clinics. For instance, Ohio employers have successfully used managed care to lower workplace injury costs, proving the value of tailored health management solutions for diverse settings.
Core Types of Health Management Solutions for Healthcare Organizations
Healthcare organizations can choose from several core types of health management solutions, each targeting specific aspects of care delivery, cost control, and operational efficiency. Understanding these solution types allows leaders to select the best fit for their unique needs and workforce profiles.
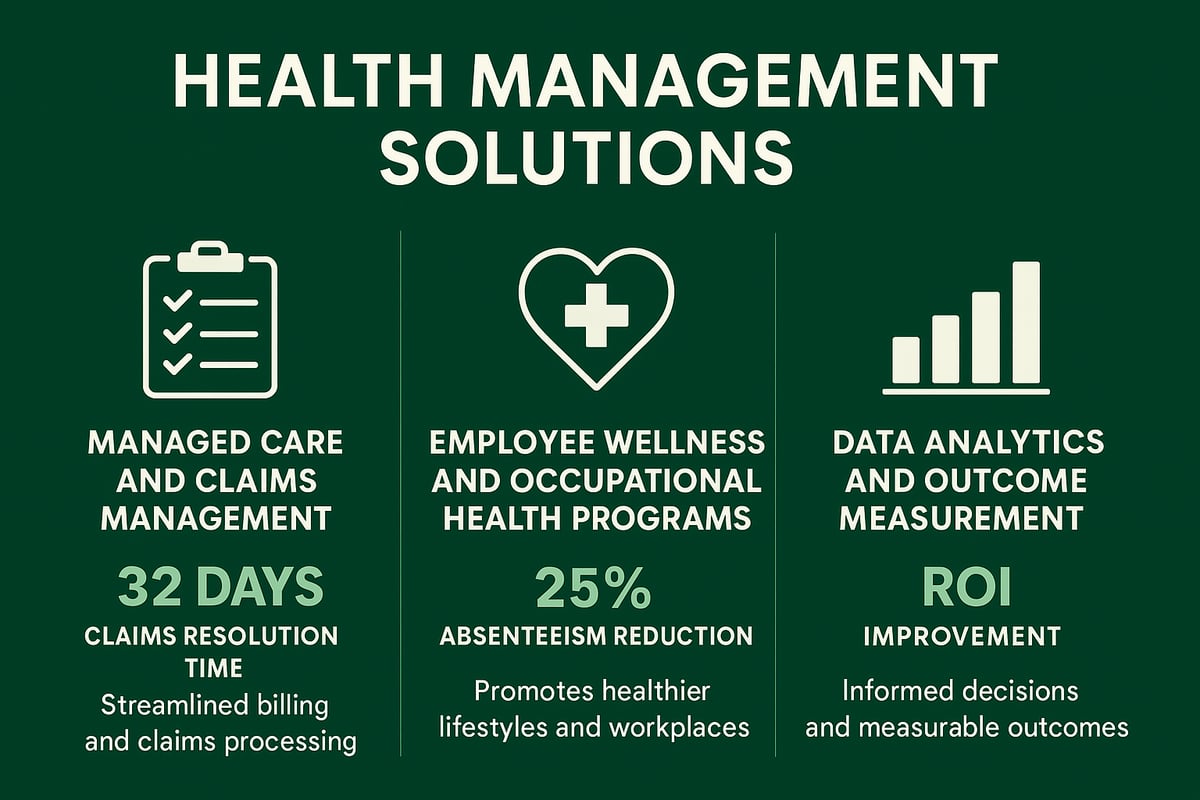
Managed Care and Claims Management
Managed care organizations play a pivotal role in streamlining workers’ compensation and reducing employer risk. Effective claims management processes minimize administrative load and speed up claim resolution, vital for both patient outcomes and cost containment.
For instance, Ohio mandates employer enrollment with MCOs, ensuring a standardized approach to claims. Integration with broader healthcare systems allows for seamless data sharing and improved coordination. Discover how denial management in medical billing further optimizes claims processes by reducing payment delays and errors.
Employee Wellness and Occupational Health Programs
Employee wellness programs focus on preventive care, chronic disease support, and mental health resources. Occupational health services address workplace injuries and facilitate safe, timely returns to work.
Organizations investing in robust wellness initiatives often see absenteeism drop by as much as 25 percent. These health management solutions not only boost productivity but also foster a healthier, more engaged workforce.
Data Analytics and Outcome Measurement
The adoption of analytics platforms is transforming health management solutions. Employers leverage data to identify high-risk populations, track program ROI, and measure outcomes like return-to-work rates and cost savings.
With real-time dashboards, organizations make informed decisions and tailor interventions for maximum impact. This data-driven approach ensures continuous improvement and demonstrates measurable value to stakeholders.
Steps to Implementing Effective Health Management Solutions
Implementing health management solutions begins with a clear understanding of your organization's unique needs. A strategic approach ensures measurable results, cost savings, and improved patient outcomes.
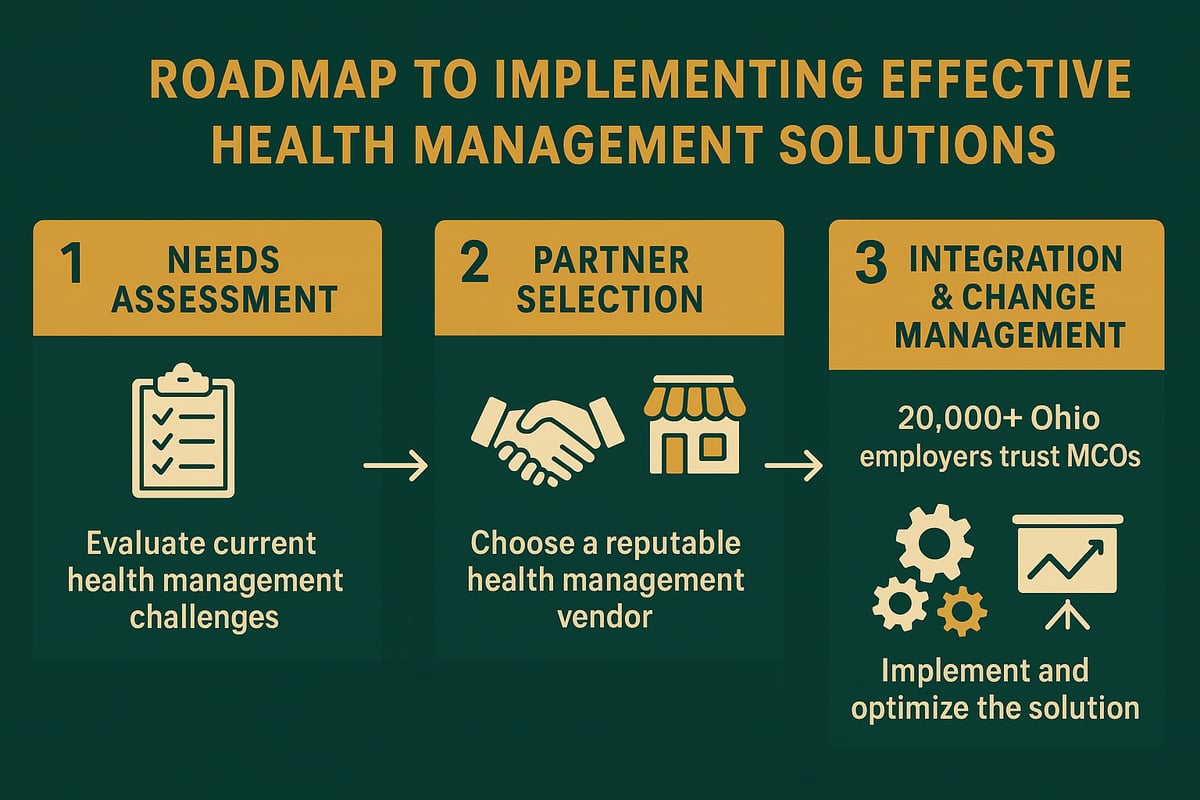
Assessing Organizational Needs and Setting Goals
Start by conducting a comprehensive assessment of your organization’s health risks, claims history, and regulatory requirements. Analyze employee demographics, common workplace injuries, and current gaps in care.
Set specific, measurable goals for your health management solutions initiative. These might include reducing claims processing time, improving employee engagement, or enhancing compliance rates. Clear objectives will guide your decisions and benchmark progress.
Selecting the Right Partners and Vendors
Choosing the right partners is essential for success. Evaluate vendors based on their expertise, scalability, and ability to integrate with your existing systems. Consider working with managed care organizations, wellness consultants, and analytics specialists.
Look for a track record of reliability and adaptability. For example, more than 20,000 Ohio employers rely on specialized MCOs for expert claims management. The right partnership will support ongoing improvement and operational efficiency.
Integration and Change Management
Develop a step-by-step implementation plan tailored to your organization. Train staff on new processes and communicate changes across all departments to ensure buy-in.
Address early adoption challenges by gathering feedback and adjusting strategies as needed. Integrating analytics tools, such as those described in Healthcare revenue cycle analytics, can help monitor key performance indicators and provide actionable insights throughout the transition.
A successful rollout of health management solutions depends on continuous evaluation and a willingness to adapt. By following these steps, your organization can achieve sustainable improvements in care delivery and cost management.
Compliance, Security, and Regulatory Considerations
Navigating compliance and security is critical for organizations using health management solutions. Regulatory requirements are constantly evolving, making it essential to stay informed and proactive.
Healthcare providers must adhere to core regulations such as HIPAA for patient privacy and OSHA for workplace safety. Industry-specific rules also shape how data is managed and protected. Failure to comply can result in significant financial penalties and reputational harm.
Secure data handling should be a top priority. Health management solutions must ensure encryption, access controls, and regular audits. Integrating compliance into daily workflows helps maintain standards without disrupting operations.
Managed care organizations often support employers by providing compliance expertise and guidance. Ongoing training and monitoring are essential. According to industry reports, 70% of healthcare organizations identify compliance as a top challenge when implementing new solutions.
To strengthen your compliance strategy, consider these best practices:
- Conduct regular risk assessments and audits
- Update policies to reflect regulatory changes
- Train staff on data security protocols
- Use dashboards to track compliance metrics
- Engage with partners who have proven compliance support
With the rise of cybersecurity threats and stricter regulations, staying ahead is vital. For more on the latest regulatory and security trends, see Eight Health Trends for 2026. By embedding compliance into your health management solutions, you can protect your organization while achieving operational excellence.
![]()
Measuring Success: KPIs and Continuous Improvement
Evaluating the impact of health management solutions is essential for healthcare organizations seeking measurable results. The right key performance indicators (KPIs) allow leaders to track progress, demonstrate value, and drive continuous improvement in care delivery and operational efficiency.
| KPI | Description | Benchmark |
|---|---|---|
| Return-to-Work Rate | Measures speed of employee recovery and reintegration | 20% faster with managed care |
| Claims Resolution Time | Tracks average days to close claims | Industry average: 30-45 days |
| Employee Satisfaction | Assesses engagement and wellness program participation | 60%+ satisfaction |
| Cost Savings | Calculates reduction in healthcare and admin expenses | Up to 25% decrease |
Modern analytics platforms and dashboards enable real-time monitoring of these KPIs. By leveraging data, organizations can identify trends, address challenges promptly, and tailor interventions for high-risk groups. Regular program reviews and stakeholder feedback sessions are vital for refining health management solutions and ensuring alignment with business goals.
For example, many employers use claims data to spot bottlenecks and deploy targeted wellness initiatives, resulting in higher return-to-work rates and lower absenteeism. Comparing performance against industry benchmarks, as outlined in the 2026 Global Health Care Outlook, helps organizations stay competitive and compliant.
Continuous improvement relies on adapting programs based on performance data. Investing in robust health management solutions delivers strong ROI, improved patient outcomes, and sustained operational excellence.
Innovations and Future Trends in Health Management Solutions
Healthcare organizations are embracing a new wave of innovation to stay ahead in a competitive industry. From AI-powered analytics to digital wellness platforms, technology is transforming how health management solutions deliver results for employers and care teams.
AI-driven tools are enabling real-time monitoring, risk prediction, and personalized interventions. For example, AI-driven ecosystems for chronic disease management are helping providers and employers manage populations more proactively, leading to better outcomes and improved operational efficiency.
Telehealth and remote care are now essential, especially as hybrid and remote work models become standard. These advances allow organizations to extend care access, offer virtual wellness programs, and support employees wherever they are. The focus on mental health and holistic well-being continues to grow, with tailored solutions addressing stress, burnout, and preventive care.
Regulatory frameworks are also evolving, requiring ongoing attention to compliance and data security. Organizations must stay alert to changing requirements and adapt their health management solutions to ensure both effectiveness and legal alignment.
Looking ahead, market analysts project significant growth for the sector, driven by demand for integrated care models and value-based reimbursement. To remain competitive, organizations should invest in continuous learning, strategic partnerships, and advanced technologies that align with their operational goals.
As you look ahead to 2026, it is clear that staying ahead in healthcare demands more than just adapting to new trends—it requires a proactive approach to optimizing your revenue cycle, streamlining operations, and ensuring compliance every step of the way. Greenhive Billing Solutions understands the unique challenges you face, from claims processing to keeping up with evolving regulations. If you are ready to identify opportunities for operational improvement and maximize your reimbursements, I invite you to Book Your Free Consultation. Let us help you build a strategy for lasting success—your future starts now.

