Cardiology practices face a complex financial landscape, where even minor billing errors or regulatory shifts can lead to significant lost revenue. Denials, underpayments, and policy changes put millions of dollars at stake each year, making effective management critical for long-term stability.
This guide delivers a step-by-step approach to cardiology revenue cycle management, designed for healthcare professionals seeking to secure every dollar earned. You will discover the unique challenges in cardiology RCM, proven best practices, the impact of technology, compliance essentials, team-building strategies, and when to consider outsourcing.
Ready to transform your approach and protect your bottom line? Dive in to unlock actionable strategies for RCM success.
Understanding the Unique Challenges of Cardiology Revenue Cycle Management
Cardiology revenue cycle management presents distinct hurdles compared to other specialties. The sheer volume of procedures, coupled with frequent coding updates, creates an environment where small errors can have major financial consequences. Cardiology claims often require detailed documentation and precise coding, making the process highly susceptible to mistakes.
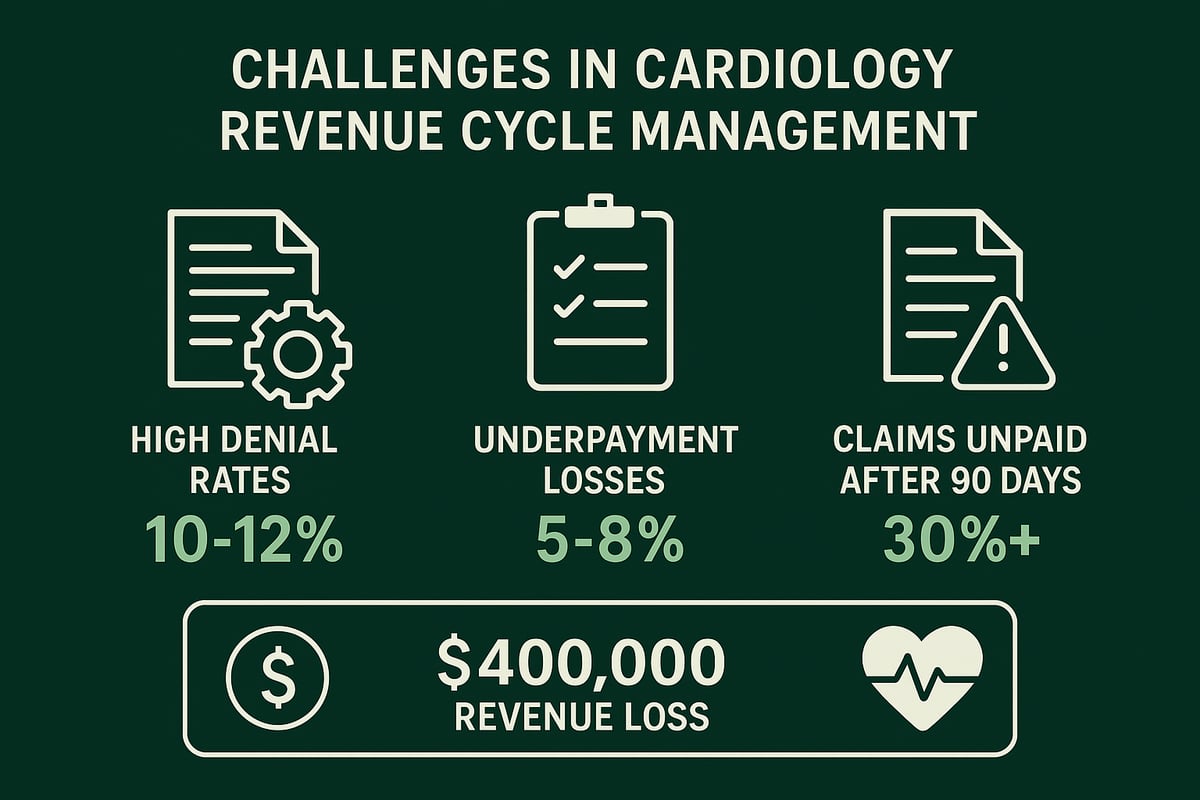
Common revenue leaks include claim denials, underpayments, and aging accounts receivable. On average, cardiology practices experience denial rates between 10% and 12%, with typical annual revenue loss from underpayments ranging from 5% to 8%. More than 30% of claims may remain unpaid after 90 days, severely impacting cash flow.
The root causes are varied: coding errors, missing or incomplete documentation, delays in obtaining prior authorizations, and sudden payer policy changes. Regulatory shifts and increased payer scrutiny further complicate cardiology revenue cycle management, increasing the risk of audits or delayed payments. For example, a mid-sized practice can unknowingly lose $400,000 each year due to unnoticed underpayments.
To combat these challenges, specialty-specific expertise is essential. Engaging professionals who understand both clinical and billing nuances can help practices reduce denials, optimize collections, and maintain compliance. For more on strategies to address denials, see Denial management in medical billing.
Step-by-Step Best Practices for Cardiology RCM Optimization
A successful approach to cardiology revenue cycle management begins with structured, repeatable processes. These best practices help minimize revenue loss, improve compliance, and support sustainable growth for cardiology practices. Let us break down the steps your team should follow for optimal results.
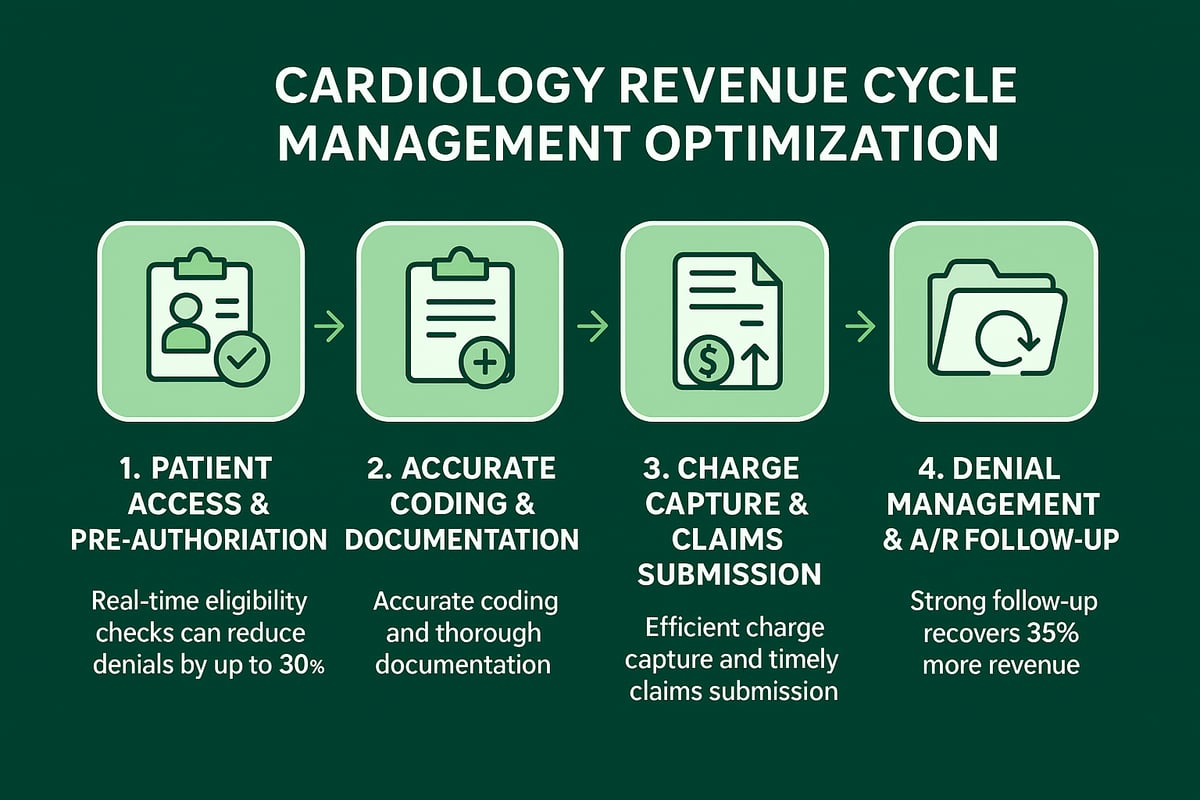
Step 1: Streamline Patient Access and Pre-Authorization
Start by automating eligibility verification and benefits checks before each appointment. This ensures patients are covered and reduces surprises at the front desk. Secure prior authorizations in advance to avoid delays in care and payment. Real-time eligibility checks can decrease claim denials by up to 30 percent, directly impacting cardiology revenue cycle management efficiency.
- Automate eligibility checks
- Obtain prior authorizations early
- Reduce scheduling bottlenecks
Step 2: Ensure Accurate Coding and Documentation
Certified coders with deep cardiology knowledge are essential. Regular coding audits help catch errors and prevent compliance issues. Invest in documentation improvement programs so clinical notes support accurate billing. For more on the critical role of coding, see Medical coding revenue cycle management.
- Employ certified cardiology coders
- Conduct frequent audits
- Enhance documentation quality
Accurate coding is the backbone of effective cardiology revenue cycle management.
Step 3: Optimize Charge Capture and Claims Submission
Establish clear processes to guarantee every service is billed. Submit claims within seven days of the encounter to speed up reimbursement. Use double-check systems to prevent missed or incorrect charges, which often lead to lost revenue.
- Track all services provided
- Submit claims quickly
- Implement charge reconciliation
Efficient charge capture keeps your revenue cycle on track.
Step 4: Strengthen Denial Management and A/R Follow-Up
Monitor denials closely, analyze root causes, and resubmit corrected claims without delay. Assign dedicated staff to follow up on aging accounts receivable. Practices with strong follow-up recover up to 35 percent more revenue, a significant boost for cardiology revenue cycle management.
- Review denials regularly
- Resubmit claims promptly
- Aggressively follow up on unpaid claims
Consistent follow-up ensures your practice captures all earned revenue.
Leveraging Technology and Automation in Cardiology RCM
The landscape of cardiology revenue cycle management is rapidly evolving as practices turn to advanced technology and automation for a competitive edge. Efficient workflows, powered by integrated RCM tools, are now essential for optimizing financial health and reducing revenue leakage.
Automation Benefits and Applications
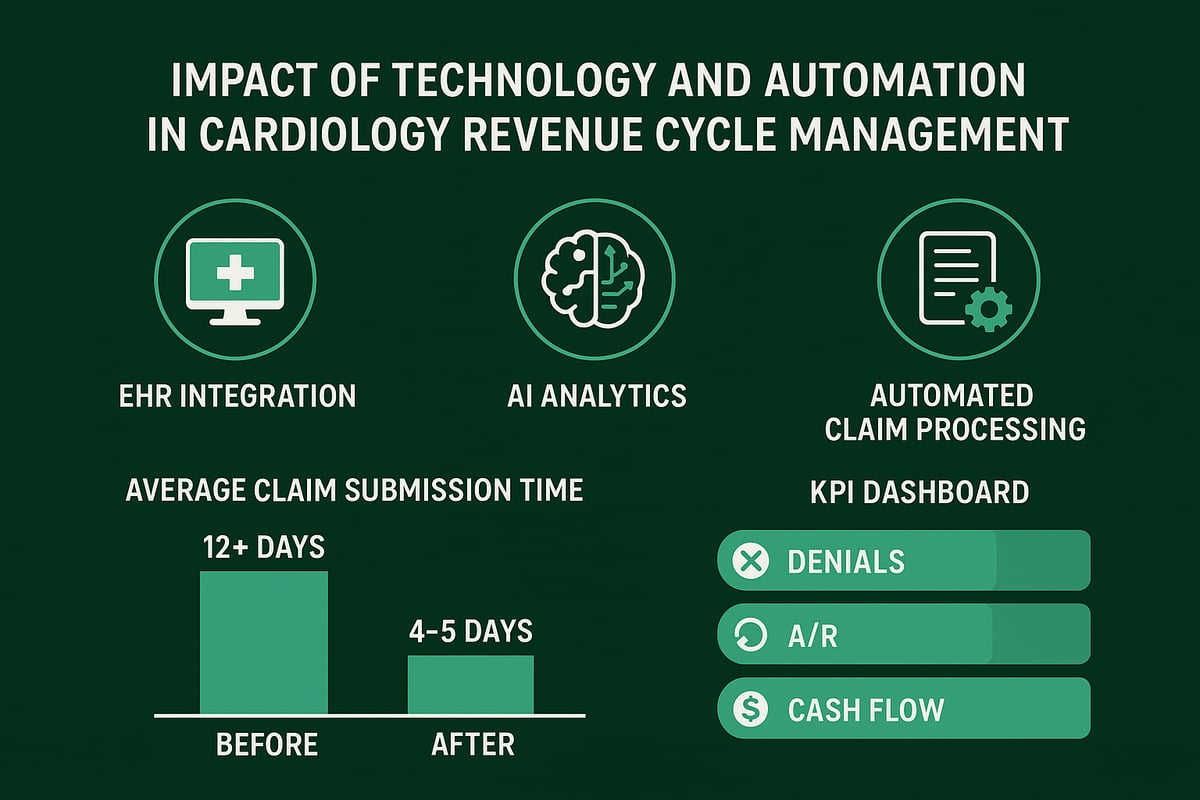
Modern RCM platforms seamlessly integrate with EHR and practice management systems, streamlining daily operations. Automated eligibility checks, real-time benefits verification, and digital payment posting minimize manual data entry and reduce the risk of errors. AI-driven denial management tools quickly flag and categorize rejected claims, allowing teams to prioritize high-value recoveries.
Key benefits include:
- Faster claim cycles and reduced administrative workload
- Fewer manual errors and better compliance
- Enhanced visibility into key performance indicators (KPIs) through analytics dashboards
With these tools, practices can track trends in denials and identify revenue leaks instantly. This data-driven approach supports proactive decision-making and continuous process improvement.
Real-World Impact and Implementation
Cardiology revenue cycle management professionals see tangible results when automation is paired with skilled staff. Practices leveraging automation typically reduce claim submission times from over 12 days to just 4-5 days. Analytics dashboards also help managers monitor A/R aging and accelerate collections.
Adoption does come with challenges. Staff must be trained to use new platforms, and integrations with existing systems require careful planning. Ongoing support is critical to maximize technology’s value. According to Advanced RCM Strategies Help Streamline Operations, Improve Profits, the greatest financial improvements are achieved when technology is combined with expert oversight.
Ultimately, automation should enhance—not replace—specialized RCM expertise. The right balance delivers sustainable financial performance and operational efficiency.
Ensuring Compliance and Revenue Integrity in Cardiology Billing
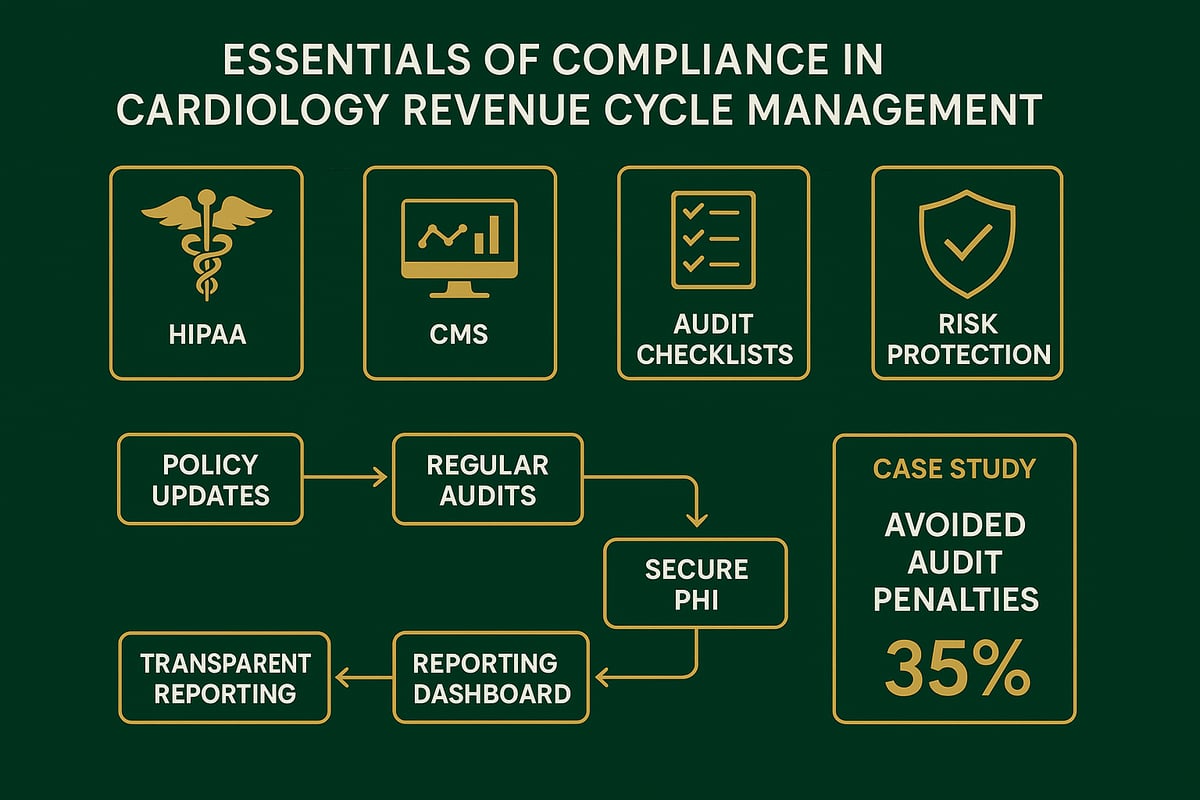
Staying compliant is non-negotiable for cardiology revenue cycle management. Regulatory requirements, such as HIPAA and CMS guidelines, are constantly evolving, and failing to keep up can jeopardize your practice’s revenue and reputation.
Regulatory Compliance and Payer Policies
Cardiology practices must monitor frequent changes in payer requirements and coding standards. Staying current reduces the risk of claim denials, penalties, and unexpected audits. Understanding the revenue cycle process in healthcare is foundational for ensuring compliance at every stage.
Audit Strategies and Documentation Reviews
Regular compliance audits are essential. Conduct periodic documentation reviews to catch errors before they trigger payer scrutiny. Internal controls, such as audit trails and transparent reporting, help maintain accountability and revenue integrity across teams.
PHI Security and Maintaining Transparency
Protecting patient health information is a legal and ethical mandate. Implement HIPAA-compliant processes, secure data storage, and strict access controls. Clear protocols for handling sensitive information reduce the risk of breaches and support regulatory compliance.
Case Example: Proactive Compliance in Action
A cardiology practice avoided a costly audit by performing routine compliance checks and updating its documentation protocols. Partnering with RCM experts ensures ongoing adherence to changing standards and preserves revenue integrity for the long term.
Building and Training a High-Performance RCM Team
A high-performing team is essential for mastering cardiology revenue cycle management. The right mix of expertise, training, and collaboration builds a strong foundation for revenue success.
Key roles in a successful RCM team include:
- Certified coders with cardiology expertise
- Billing specialists who understand payer requirements
- Denial management experts focused on appeals
- Compliance officers ensuring regulatory adherence
Ongoing training keeps your team current with the latest codes, payer policies, and system updates. Cross-functional collaboration between clinical and billing staff helps bridge communication gaps and ensures accurate claims.
Setting clear performance metrics and regular feedback loops drives accountability. Track error rates, denial trends, and collection ratios to measure progress.
Practices with dedicated RCM teams often see collection rates improve by 12-18%. This improvement is a direct result of specialized focus and continuous education, as highlighted in Optimizing Cardiology Revenue: Proven Strategies for 2025 and Beyond.
Investing in ongoing certification and education ensures your cardiology revenue cycle management team stays ahead of industry changes and delivers measurable results.
Outsourcing Cardiology Revenue Cycle Management: When and Why to Consider It
Outsourcing cardiology revenue cycle management can be a strategic solution when your practice faces persistent claim denials, slow reimbursements, high administrative costs, or staff burnout. These pain points often signal that internal resources are stretched thin, making it difficult to keep up with the evolving demands of payers and regulatory changes.
When weighing in-house versus outsourced RCM, practices must consider cost efficiency, results, and scalability. In-house teams may struggle with rising overhead and limited expertise, while outsourcing can provide access to specialized professionals and proven workflows. According to industry data, more than 58% of specialty practices have turned to outsourcing for improved outcomes, including higher collection rates and faster claims processing.
The financial impact is significant. Outsourcing can reduce operational costs by an average of $90,000 per year, while helping practices capture more revenue through dedicated denial management and timely submissions. To learn more about the key benefits and considerations, visit Revenue cycle management outsourcing for a comprehensive overview.
Common concerns about data security and control are valid, but reputable RCM partners offer HIPAA-compliant processes, transparent reporting, and certified staff. When selecting a partner, look for cardiology expertise, clear communication, and a track record of measurable results.
A recent example involved a cardiology group that reversed declining revenue by outsourcing their RCM. With fewer denials, improved cash flow, and reduced administrative burden, their practice achieved sustainable financial growth and peace of mind.
As you’ve seen throughout this guide, mastering cardiology revenue cycle management requires a careful blend of expertise, technology, and ongoing compliance. If you’re ready to uncover hidden opportunities in your reimbursement process, a tailored audit could be the first step toward better financial health for your practice. With Greenhive Billing Solutions, you gain a partner who understands the unique challenges of cardiology billing and offers transparent, HIPAA compliant support every step of the way.
Take the next step and Get Your Free Audit—let’s work together to maximize your collections, reduce denials, and set your practice up for success in 2026.