Healthcare organizations today face mounting pressures as revenue management grows more complex each year. Staying financially healthy can be challenging, but this rev cycle pro guide is designed to help your practice gain control and achieve lasting success.
Inside, you will find step-by-step strategies, expert insights, and actionable solutions for optimizing every stage of the revenue cycle. Discover fundamentals, tackle common challenges, and learn how technology, compliance, and future trends can drive improvement.
Ready to boost your revenue performance? Explore proven techniques and empower your team to take action today.
Understanding the Revenue Cycle: Foundations for Financial Success
Mastering the healthcare revenue cycle is essential for organizations aiming for financial stability and growth. The path from patient registration to the final payment is complex, involving many moving parts and stakeholders. For any healthcare organization, adopting a rev cycle pro mindset is the key to navigating this landscape with confidence.
Defining the Revenue Cycle in Healthcare
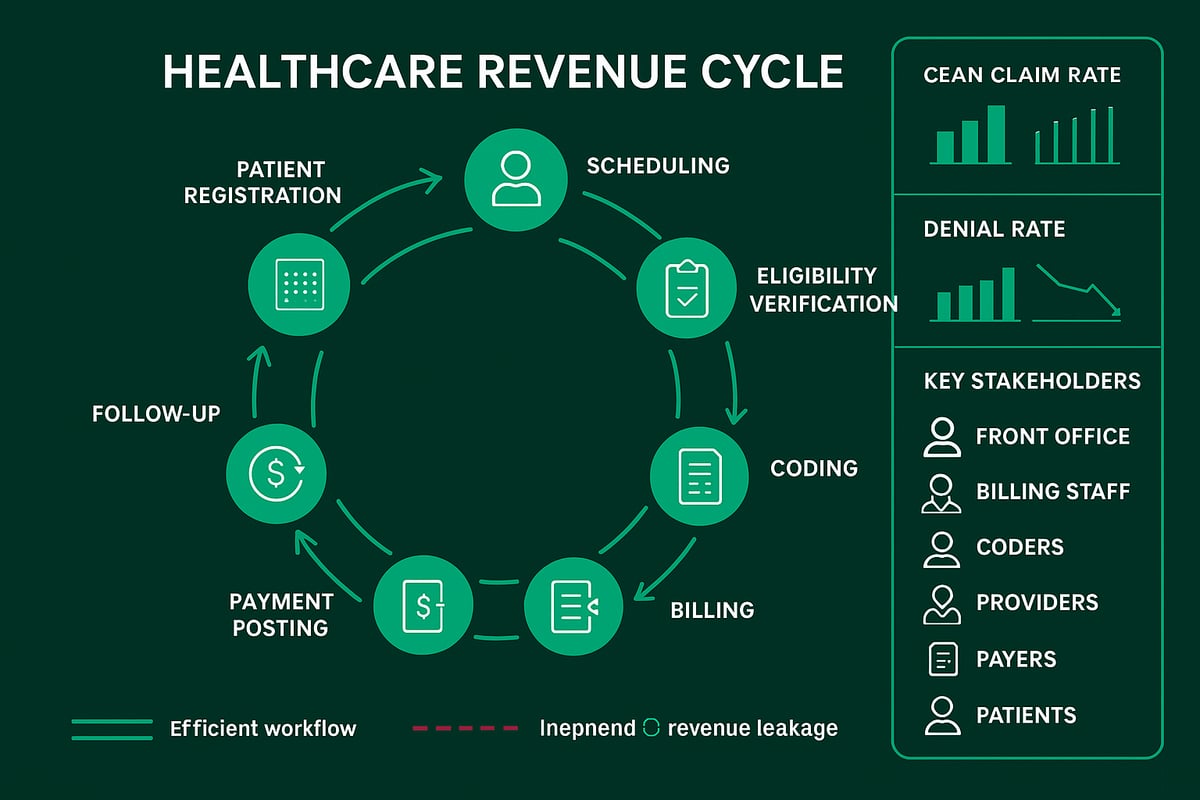
The healthcare revenue cycle is the end-to-end process that begins when a patient schedules an appointment and concludes once the provider receives complete payment for services rendered. Each phase, from initial scheduling and insurance verification to accurate coding, billing, and final follow-up, plays a critical part in sustaining your organization’s cash flow.
A streamlined workflow means information is captured accurately at every step, reducing errors and speeding up reimbursement. In contrast, an inefficient process can cause bottlenecks, claim denials, and delayed payments. For a deeper look at how these steps interconnect, the Revenue cycle medical billing overview offers valuable insights.
By prioritizing each stage, organizations position themselves as rev cycle pro leaders, able to identify risks and opportunities early.
Core Components and Stakeholders
A successful rev cycle pro approach depends on seamless coordination among the internal teams and external partners involved. Internally, the front office manages patient intake, billing staff handle claims, and certified coders ensure services are documented correctly. Providers play a crucial role by supplying accurate clinical information.
Externally, payers (insurance companies), clearinghouses, and patients all affect the pace and outcome of revenue collection. When these parties communicate effectively, revenue flows smoothly. However, any breakdown in collaboration can disrupt the entire process and impact financial performance.
Interdepartmental alignment and clear protocols are vital for minimizing delays and ensuring every claim is processed efficiently.
Metrics That Matter: KPIs for Revenue Cycle Health
To operate as a rev cycle pro, your organization must track the right key performance indicators (KPIs). The clean claim rate shows how often claims are submitted correctly the first time. Days in accounts receivable (A/R) measures how quickly payments are collected. The denial rate highlights the percentage of claims rejected by payers, while the net collection rate reveals how much of the total billed amount is actually collected.
Industry benchmarks, such as those from MGMA, report median A/R days for practices as a reference point. Regularly monitoring these KPIs helps organizations identify trends, set improvement goals, and maintain cash flow stability.
A proactive focus on these metrics empowers your team to spot issues before they escalate.
The Cost of Inefficiency: Revenue Leakage and Its Impact
Revenue leakage can quietly erode your bottom line. Common sources include claim denials, undercoding, and challenges in collecting patient payments. The average denial rate ranges from 6 to 13 percent, translating into significant lost revenue for many practices.
For example, a single practice might lose $50,000 annually due to preventable claim errors. Without a rev cycle pro strategy, these issues can accumulate and threaten long-term sustainability.
Addressing inefficiencies is not just about boosting revenue, but also about building a resilient and future-ready organization.
Common Revenue Cycle Challenges Facing Healthcare Providers
Healthcare organizations striving for rev cycle pro status face a landscape filled with obstacles. These challenges impact cash flow, compliance, and patient satisfaction. Addressing them effectively is crucial for sustainable revenue management.
![]()
Denials and Delays: Root Causes and Solutions
Claim denials are a top concern for any rev cycle pro. The main causes include eligibility issues, coding errors, and missing information. Over 65% of denied claims are never resubmitted, resulting in significant revenue leakage.
To reduce denials, it is essential to focus on accurate data entry, eligibility verification, and coding reviews. Implementing denial management strategies in billing ensures timely follow-up and appeals, turning lost claims into recovered revenue.
Patient Financial Responsibility and Collection Difficulties
With rising out-of-pocket costs, patient collections present a major hurdle for the rev cycle pro. Studies show that up to 30% of patient payments are never collected, especially in smaller practices.
Best practices include transparent financial communication, upfront estimates, and offering payment plans. Early engagement and digital payment options help practices collect more efficiently while maintaining positive patient relationships.
Compliance Risks and Regulatory Changes
Staying compliant is a core responsibility for every rev cycle pro. Constant updates to HIPAA, payer policies, and coding standards create risk for non-compliance and potential penalties.
Ongoing staff training, policy reviews, and robust documentation are vital. Practices that prioritize compliance avoid costly fines, adapt quickly to regulatory shifts, and maintain trust with payers and patients.
Staffing, Training, and Process Bottlenecks
Staff turnover, limited expertise, and manual processes can slow down the rev cycle pro. Billing delays and bottlenecks result in delayed payments and increased errors.
Investing in cross-training, workflow standardization, and process automation helps teams work efficiently. A well-trained, agile staff ensures that revenue cycle operations remain smooth, even as industry demands evolve.
Step-by-Step Guide to Revenue Cycle Optimization
Optimizing your revenue cycle is not a one-time project but a repeatable process. For healthcare organizations, mastering each stage is what separates a struggling operation from a high-performing rev cycle pro team. Below, we break down the most critical steps to help your organization streamline cash flow, reduce denials, and drive sustainable growth.

Step 1: Patient Scheduling and Pre-Registration
The journey to becoming a rev cycle pro starts with precise scheduling and pre-registration. This foundation ensures smooth billing down the line. Capturing accurate patient demographics and insurance information at the outset reduces errors that can lead to costly denials.
Best practices include verifying contact details, confirming insurance coverage, and collecting copay information upfront. Many organizations use checklists or digital forms to standardize this process.
Benefits of clean intake:
- Fewer claim rejections
- Faster patient throughput
- Improved patient satisfaction
A robust intake process sets the tone for the entire revenue cycle and positions your team for long-term success.
Step 2: Insurance Verification and Prior Authorization
Insurance verification is a key step for any rev cycle pro. Verifying patient eligibility in advance prevents delays and denials. Prior authorization, when required, must be obtained before services are rendered to avoid reimbursement issues.
Automated verification tools can check insurance status in real time, saving valuable staff hours. Practices that implement automated workflows often see a 20 percent reduction in denials linked to eligibility or authorization.
Checklist for effective verification:
- Confirm coverage and benefits
- Identify out-of-pocket costs
- Secure prior authorizations as needed
Investing time in this step reduces downstream workload and ensures claims are processed smoothly.
Step 3: Coding Accuracy and Documentation
Accurate coding is the engine behind a successful rev cycle pro operation. Certified medical coders ensure every service is documented and coded to the highest level of specificity, maximizing reimbursement and minimizing compliance risk.
Ongoing education is vital, as coding standards and payer requirements evolve. Specialty-specific codes can capture the full complexity of patient care.
Under-coding can lead to a 5 to 10 percent revenue loss for practices. For a deeper dive into the impact of coding, visit Medical coding’s role in RCM.
Strong documentation and coding not only drive revenue but also protect your organization during audits.
Step 4: Claims Submission and Tracking
A rev cycle pro ensures claims are submitted cleanly and efficiently. Using electronic claims scrubbing tools helps catch errors before submission, reducing rejections and shortening payment cycles.
Electronic submission offers faster turnaround and better tracking compared to manual processes. It is critical to monitor claim status, address rejections promptly, and resubmit corrected claims without delay.
Tips for effective claims management:
- Use claims scrubbing software
- Track claims daily
- Resolve errors within 48 hours
Proactive tracking can significantly improve cash flow and reduce days in A/R.
Step 5: Payment Posting and Reconciliation
Timely and accurate payment posting is a hallmark of a rev cycle pro. As payments are received from payers and patients, they must be posted in real time to avoid errors and misapplied funds.
Automated reconciliation tools help identify underpayments or short pays, allowing organizations to pursue outstanding balances efficiently.
Benefits of streamlined posting:
- Immediate visibility into collections
- Quick identification of payment gaps
- Accurate financial reporting
Effective reconciliation ensures your revenue data is reliable and actionable.
Step 6: Denial Management and Appeals
Handling denials is a critical competency for any rev cycle pro. Denials should be tracked, categorized, and analyzed to uncover root causes and trends.
A structured appeals process allows your team to recover lost revenue quickly. Practices that proactively manage denials and submit timely appeals can recover up to $100,000 or more annually.
Key steps in denial management:
- Log each denial with reason codes
- Conduct root cause analysis monthly
- Standardize appeals documentation
Resolving denials efficiently keeps your revenue cycle healthy and predictable.
Step 7: Patient Billing and Collections
The final step for a rev cycle pro is transparent, patient-friendly billing and diligent collections. Clear statements, multiple payment options, and digital reminders improve the likelihood of collecting balances.
Early intervention is essential. Practices that communicate proactively with patients and offer payment plans see a reduction in bad debt and higher patient satisfaction.
Best practices for collections:
- Send statements promptly
- Offer online payment portals
- Follow up with personalized reminders
A strong patient collections process closes the revenue loop and boosts overall financial performance.
Leveraging Technology and Outsourcing for Revenue Cycle Excellence
Modern healthcare organizations face mounting financial and operational complexity. To stay ahead, a rev cycle pro approach leverages both advanced technology and specialized outsourcing partners. This combination streamlines revenue processes, boosts collections, and ensures compliance, empowering providers to focus on patient care.
![]()
Role of RCM Technology: EHRs, Clearinghouses, and Automation
A rev cycle pro strategy harnesses the power of integrated EHR and billing platforms to eliminate manual errors and accelerate workflows. Automation tools verify insurance eligibility, streamline coding, and enable real-time payment posting. Practices integrating EHRs with clearinghouses report a 15% improvement in A R days, underscoring the impact of seamless data flow.
Automation also supports claim scrubbing, flagging issues before submission. This reduces denials and shortens reimbursement cycles. By embedding analytics into daily operations, organizations gain visibility into bottlenecks and performance metrics. For a deeper dive into analytics and KPIs, Healthcare revenue cycle analytics offers valuable insights.
Benefits of Outsourcing Revenue Cycle Management
Partnering with a rev cycle pro outsourcing firm delivers access to industry expertise and scalable resources. Outsourcing reduces the burden of hiring, training, and retaining in-house billing staff. It also provides continuity during staff turnover or surges in claim volume.
Outsourced teams specialize in denial management, coding updates, and payer policy changes. This focus ensures compliance and maximizes collections. Many practices find that outsourcing yields significant cost savings compared to maintaining a full internal department.
| Feature | In-House Billing | Outsourced RCM |
|---|---|---|
| Staffing Burden | High | Low |
| Expertise Access | Limited | Extensive |
| Scalability | Challenging | Flexible |
| Cost Efficiency | Variable | Predictable |
Greenhive Billing Solutions: Partnering for Revenue Cycle Success
Greenhive brings a rev cycle pro mindset to every client engagement. Our team of certified professionals delivers comprehensive RCM services, adapting to client-owned software and systems. We ensure HIPAA compliance, transparent reporting, and ongoing communication.
Clients working with Greenhive experience higher clean claim rates and faster collections. Our proactive denial management and analytics-driven approach position organizations for sustainable growth. We act as an extension of your team, focused on your revenue health and operational excellence.
Data Security and Compliance Considerations
A true rev cycle pro partnership prioritizes data security at every stage. Healthcare providers must ensure their RCM partners adhere to HIPAA regulations, secure data transfers, and robust storage protocols. Breach response plans and regular audits are essential to maintain trust and avoid costly penalties.
When evaluating technology solutions, confirm that vendors offer end-to-end encryption, role-based access, and audit trails. Ongoing staff training on compliance requirements further reduces risk and supports a culture of accountability.
Choosing the Right RCM Partner or Platform
Selecting a rev cycle pro partner is a strategic decision. Key criteria include experience with your specialty, transparent fee structures, responsive support, and proven results. Request references and case studies to validate performance claims.
Use this checklist when evaluating RCM vendors:
- Does the provider have deep industry expertise?
- Can they work seamlessly with your existing software?
- Are reporting and analytics accessible and actionable?
- Is their compliance record strong and up to date?
Many organizations see a 20% reduction in A R days after switching to the right partner. Taking the time to vet your options ensures a successful, long-term revenue cycle strategy.
Compliance, Regulatory Trends, and Risk Mitigation
Staying ahead of compliance requirements is essential for every rev cycle pro. Regulations continue to evolve, challenging healthcare organizations to adapt quickly. Payment models, coding standards, and privacy laws are updated frequently. For example, the transition to ICD-11 brings new documentation rules and payer expectations. Remaining current with CMS and commercial payer updates is crucial. The shift toward value-based care is a significant driver for regulatory change, as explored in Value-Based Care’s Impact on RCM. Proactive monitoring ensures your revenue cycle stays compliant and efficient.
Building a Culture of Compliance
A strong compliance culture sets the foundation for a successful rev cycle pro approach. Regular staff training, frequent policy updates, and internal audits are vital. Encourage open communication, where team members report issues without fear. This proactive stance helps prevent costly errors and penalties. Practices that implement internal compliance programs consistently avoid regulatory fines. Make compliance a shared responsibility, with leadership setting the tone and providing resources. Establish clear procedures and reinforce them through ongoing education. This culture not only safeguards your organization but also improves overall revenue integrity.
Audit Readiness and Documentation Best Practices
Audit readiness is a hallmark of any effective rev cycle pro. Thorough, accurate documentation is your best defense during payer or government reviews. Prepare by maintaining organized records and following a standardized audit checklist:
- Verify coding accuracy
- Maintain up-to-date patient files
- Document all communications and billing actions
Regular mock audits identify gaps before an external review. Comprehensive documentation protects against denials and supports compliance. When your records are audit-ready at all times, you minimize disruptions and build payer trust. This level of preparation ensures your organization remains resilient and financially secure.
Mitigating Revenue Cycle Risks
Risk mitigation is a top priority for every rev cycle pro. Common threats include fraud, abuse, and billing errors. Leverage analytics and monitoring tools to detect anomalies early. Using predictive analytics, as highlighted in Predictive Analytics in Healthcare RCM, enables proactive identification of potential problems before they escalate. Address risks by setting up alerts, reviewing trends, and conducting regular audits. Early intervention protects revenue and reputation. A systematic risk management strategy helps you adapt quickly and prevents revenue leakage, supporting long-term financial health.
Future-Proofing Your Revenue Cycle: Trends and Strategies for Sustainable Growth
Healthcare organizations aiming to operate as a rev cycle pro must anticipate industry shifts and adopt strategies that guarantee long-term financial health. Future-proofing the revenue cycle means embracing data-driven decision-making, improving patient engagement, adapting to new payment models, investing in staff development, and setting clear goals.
Data Analytics and Predictive Insights
To remain a rev cycle pro, harnessing data analytics is essential. Real-time dashboards and KPIs empower revenue cycle leaders to spot trends, identify bottlenecks, and forecast cash flow issues before they escalate. Predictive analytics can help practices reduce denials by up to 25%, as they proactively adjust workflows in response to data.
The demand for advanced analytics is projected to surge, reflecting broader Healthcare Revenue Cycle Management Market Growth Projections. Organizations that adopt these tools gain a significant edge in efficiency and revenue integrity.
Patient Experience and Engagement in the Revenue Cycle
Modern rev cycle pro organizations recognize that patient satisfaction directly impacts collections. Offering digital payment options, transparent billing, and easy-to-use patient portals not only streamlines payment but also strengthens trust.
For instance, practices implementing patient-friendly billing have reported improved collection rates and higher patient retention. Key strategies include:
- Sending clear, itemized statements
- Providing multiple payment channels
- Automating payment reminders
These steps position your organization as both patient-centric and financially resilient.
Adapting to Value-Based Care and Alternative Payment Models
Transitioning from fee-for-service to value-based reimbursement challenges every rev cycle pro to rethink core processes. Aligning revenue cycle management with quality metrics, outcomes tracking, and risk adjustment is essential for success.
Integrating AI, as detailed in AI Integration in Revenue Cycle Management, supports automation of repetitive tasks and improves accuracy. Practices leveraging these tools have seen increased revenue through quality-driven incentives and fewer payment delays.
Talent, Training, and Organizational Agility
A rev cycle pro knows that technology alone does not drive results. Ongoing staff education, upskilling, and cross-training are critical to adapt to regulatory changes and payer requirements.
Agile teams equipped with current knowledge can quickly adjust to new coding standards or payer policies, reducing claim errors and denials. Regular workshops, e-learning modules, and peer collaboration keep teams sharp and responsive.
Strategic Planning for Long-Term Revenue Success
Long-term revenue cycle sustainability requires a rev cycle pro approach to planning. Set measurable goals, track KPIs, and benchmark against industry standards. Embrace continuous process improvement by regularly reviewing workflows, updating policies, and investing in innovation.
A strategic mindset, combined with the right tools and talent, ensures your organization stays ahead of industry trends and secures ongoing financial success.
As you reflect on the strategies we’ve covered to help you optimize every stage of your revenue cycle, it’s clear that even small improvements can drive measurable results in 2026 and beyond. If you’re ready to take the next step toward mastering your revenue processes, why not let an expert set of eyes assess your current workflow? You’ll discover actionable insights and opportunities for growth—no guesswork, just clear direction tailored to your practice’s unique needs. Start your journey to higher efficiency and stronger financial outcomes by taking advantage of our Get Your Free Audit today.
