Healthcare is rapidly evolving, demanding that organizations stay ahead with future-ready strategies. For healthcare professionals, mastering medical coding revenue cycle management is no longer optional—it is essential for financial stability and compliance.
This guide explores how to excel in medical coding revenue cycle management in 2026. You will discover the latest industry standards, groundbreaking technology, and up-to-date compliance requirements.
We will walk you through the entire RCM process, highlight innovations, and share best practices for maximizing financial outcomes. Stay informed about emerging trends and expert insights designed to help your practice thrive in the changing landscape.
Understanding the Medical Coding Revenue Cycle in 2026
The healthcare landscape in 2026 demands a deep understanding of medical coding revenue cycle management for sustained financial success. At its core, the revenue cycle encompasses every administrative and clinical function that contributes to capturing, managing, and collecting patient service revenue. For healthcare organizations, mastering this cycle is fundamental to maintaining financial stability and compliance.
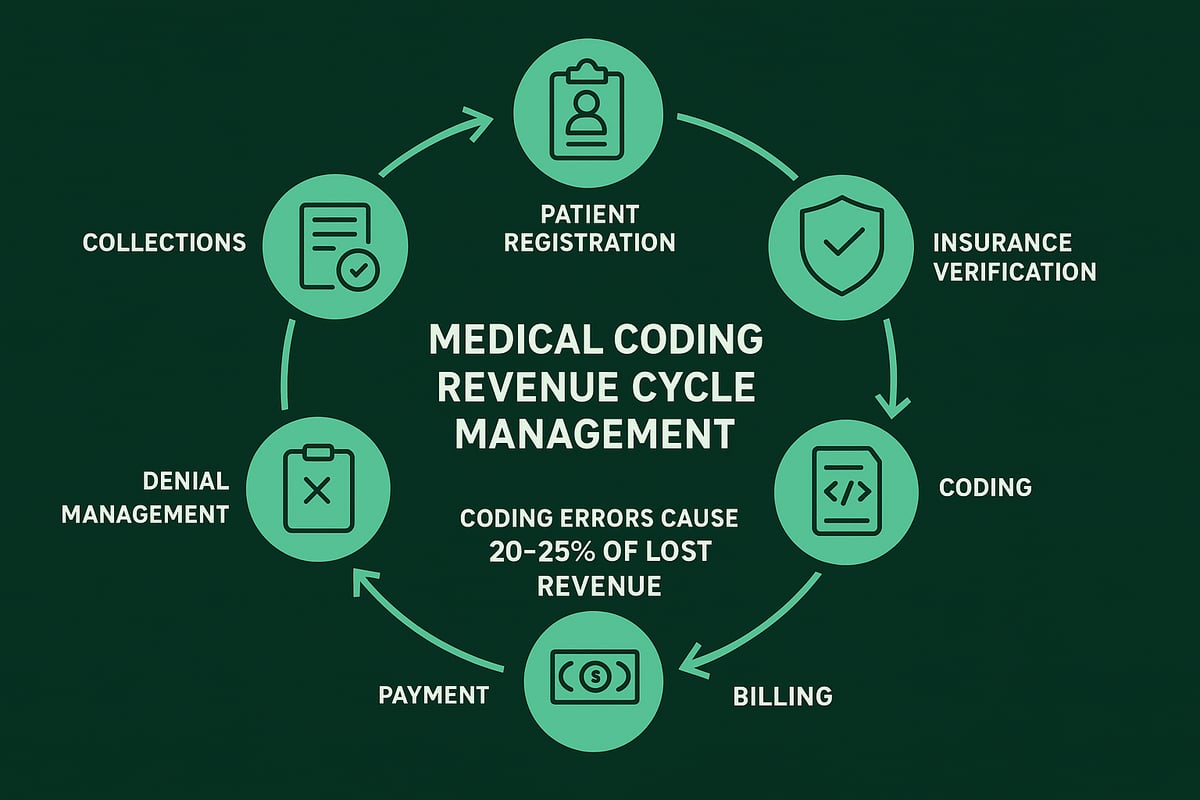
The medical coding revenue cycle management process begins with patient registration. Accurate entry of demographic and insurance details sets the stage for smooth downstream processes. Next is insurance verification, which confirms coverage and prevents eligibility-related denials. Pre-authorization and documentation collection ensure that all required information is gathered before care is delivered, minimizing the risk of delays.
Accurate charge capture and documentation review are vital steps. Here, clinical data is translated into standardized codes using systems such as ICD-11, CPT, and HCPCS. These codes drive billing, reimbursement, and reporting. Coding accuracy is increasingly important in 2026 as payer requirements become more stringent and regulatory frameworks evolve. For organizations seeking to enhance precision, Medical Coding Services Overview outlines how professional services can support compliance and efficiency.
Once coding is complete, claims are submitted to payers using specific formats and guidelines. Payment posting and reconciliation follow, tracking received payments and identifying discrepancies. Denial management addresses rejected claims, allowing for corrections and appeals. Finally, patient billing and collections round out the cycle, ensuring that outstanding balances are resolved.
The integration of medical coding revenue cycle management with EHR and practice management systems is now standard. This seamless connection reduces manual entry and improves data accuracy. However, evolving payer rules and regulatory shifts—such as updates to ICD-11 and CPT—require continuous adaptation. Organizations must monitor changes and adjust workflows promptly to avoid disruptions.
Common bottlenecks can occur at any stage of the cycle. For example, errors during insurance verification or coding often lead to claim denials, delayed payments, or compliance risks. According to industry reports, inefficiencies in medical coding revenue cycle management may result in up to 30 percent revenue loss for healthcare providers. These financial consequences underscore the need for robust processes, regular audits, and ongoing staff training.
Ultimately, a streamlined, accurate medical coding revenue cycle management process is essential for profitability and regulatory compliance. By prioritizing precision, leveraging technology, and staying informed of industry developments, healthcare organizations can overcome challenges and optimize their financial outcomes.

Key Steps in the Medical Coding Revenue Cycle Management Process
A successful medical coding revenue cycle management process is the backbone of financial health for healthcare organizations. Each step, from initial patient contact to final collections, plays a pivotal role in ensuring accurate reimbursement and compliance.
To break down medical coding revenue cycle management, consider the following essential stages:
| Step | Description |
|---|---|
| 1 | Patient Registration & Insurance Verification |
| 2 | Pre-authorization & Documentation Collection |
| 3 | Charge Capture & Documentation Review |
| 4 | Medical Coding (ICD-11, CPT 2026) |
| 5 | Claims Submission & Payer Formatting |
| 6 | Payment Posting & Reconciliation |
| 7 | Denial Management & Appeals |
| 8 | Patient Billing & Collections |
Step 1: Patient Registration and Insurance Eligibility Verification
Accurate patient registration is the first defense against downstream errors in medical coding revenue cycle management. Missing or incorrect demographic and insurance details can lead to claim rejections, directly impacting cash flow.
Verifying insurance eligibility before appointments ensures that the provider is aware of coverage limitations, preventing delays and denials later.
Step 2: Pre-authorization and Documentation Collection
Many payers require pre-authorization for specific procedures. Failing to obtain it may result in denied claims, which disrupt the medical coding revenue cycle management process. Collecting complete clinical documentation at this stage is vital for accurate coding and compliance with payer requirements.
Step 3: Accurate Charge Capture and Documentation Review
All services provided must be captured and documented thoroughly. Incomplete or inconsistent documentation can cause undercoding or overcoding, both of which jeopardize compliance and revenue.
A real-world scenario: If a clinician forgets to document a procedure, it will not be coded or billed, leading to lost revenue. Regular internal audits are necessary to identify and correct such issues.
Step 4: Medical Coding Using Updated 2026 Standards
Medical coding revenue cycle management in 2026 revolves around using the latest ICD-11, CPT, and HCPCS standards. Coders must translate clinical documentation into precise codes, reflecting the care delivered.
The adoption of updated coding systems demands ongoing education for staff and rigorous quality checks. Coding errors here remain a leading cause of claim denials, with industry reports showing they account for 20-25% of lost revenue.
Step 5: Claims Submission and Payer-Specific Formatting
Submitting claims in the correct format and within payer-specific timelines is essential. Errors in claim forms or missed deadlines can delay payments or lead to outright denials.
Automation tools can help flag incomplete or incorrect claims before submission, reducing manual work and improving the speed and accuracy of medical coding revenue cycle management.
Step 6: Payment Posting and Reconciliation
Once payments are received from payers, they must be posted accurately in the system. Discrepancies between expected and actual payments should be identified quickly.
Timely reconciliation allows organizations to spot underpayments and initiate follow-ups, ensuring optimal reimbursement for services rendered.
Step 7: Denial Management and Appeals
Denial management is a critical component of medical coding revenue cycle management. Proactive tracking, analysis, and resolution of denials prevent recurring issues and recover lost revenue.
For practical strategies to enhance denial management, explore Denial Management in Medical Billing.
Step 8: Patient Billing and Collections
Clear patient statements and proactive communication are crucial for successful collections. Patients are increasingly responsible for a larger share of healthcare costs, making transparency and empathy key.
Automated reminders and multiple payment options can improve collection rates and reduce accounts receivable days.
The Value of Workflow Automation and Regular Audits
Integrating automation into the medical coding revenue cycle management process streamlines repetitive tasks, minimizes human error, and accelerates the revenue cycle. Regular audits help identify bottlenecks and areas for improvement, supporting overall financial performance.
In summary, mastering each step of medical coding revenue cycle management is essential for reducing lost revenue, maintaining compliance, and achieving sustainable growth for healthcare organizations.
Technology & Automation: Transforming RCM in 2026
The digital revolution is reshaping how healthcare organizations approach medical coding revenue cycle management. In 2026, technology adoption is no longer optional. It is essential for maximizing reimbursements, reducing errors, and maintaining compliance in a rapidly evolving regulatory environment.
AI, Automation, and RPA in RCM
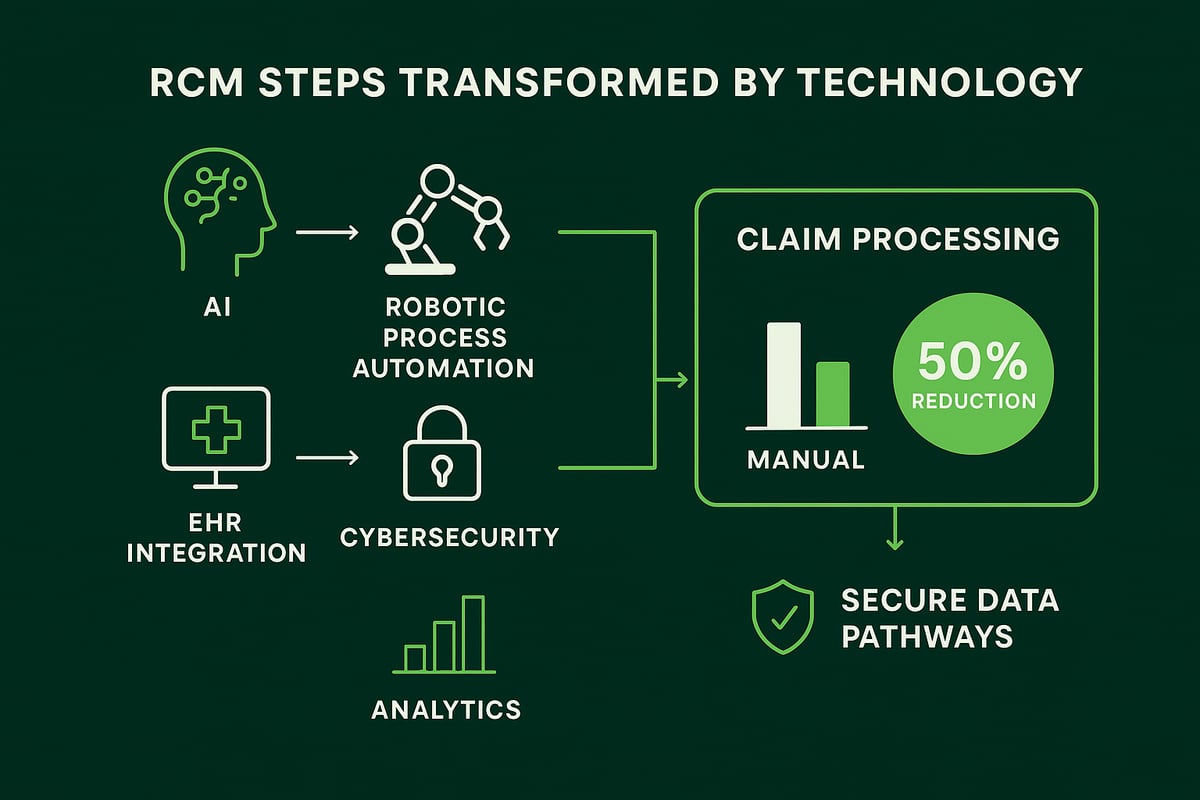
Artificial intelligence and automation are at the core of modern medical coding revenue cycle management. AI-driven coding assistance analyzes clinical documentation, suggests accurate codes, and flags inconsistencies before claims are submitted. Automated claim scrubbing tools catch common errors, helping prevent denials and delays. Predictive analytics identify high-risk claims, enabling proactive intervention.
Robotic process automation (RPA) is also playing a major role. RPA bots handle repetitive tasks, such as data entry and eligibility checks, with minimal human oversight. This results in fewer mistakes, faster throughput, and more time for staff to focus on complex cases. According to recent industry reports, automation can cut claim processing times by up to 50%.
To explore the latest innovations and trends, see this detailed overview of AI and automation in RCM.
| Automation Benefit | Impact on RCM |
|---|---|
| AI Coding Assistance | Reduces coding errors |
| Claim Scrubbing | Lowers denial rates |
| Predictive Analytics | Prevents lost revenue |
| RPA Bots | Speeds up workflows |
EHR Integration and Interoperability
Seamless integration between RCM platforms and electronic health records (EHRs) is now standard in medical coding revenue cycle management. Interoperability ensures that demographic, clinical, and billing data flow securely between systems, reducing duplicate entry and manual handoffs. This not only improves coding accuracy but also accelerates the entire revenue cycle, from patient registration to final collections.
Healthcare organizations that leverage these integrations experience fewer bottlenecks and can adapt more quickly to payer rule changes or regulatory updates.
Cybersecurity and HIPAA Compliance
As medical coding revenue cycle management becomes more digital, data security and patient privacy are top priorities. Cyber threats are increasing, and HIPAA compliance is non-negotiable. Organizations must invest in encrypted communications, multi-factor authentication, and regular security audits to safeguard sensitive health information.
A single breach can result in significant financial penalties and reputational harm. Proactive risk management is critical for protecting both patient data and organizational integrity.
Human Oversight and the Future
Despite the surge in automation, expert human oversight remains indispensable in medical coding revenue cycle management. Technology accelerates routine processes and reduces errors, but experienced professionals ensure compliance, handle exceptions, and interpret complex regulations.
The most successful healthcare organizations in 2026 will combine advanced technology with specialized RCM expertise, adapting quickly to new challenges and optimizing every stage of the revenue cycle.
Regulatory Compliance and Risk Management in 2026
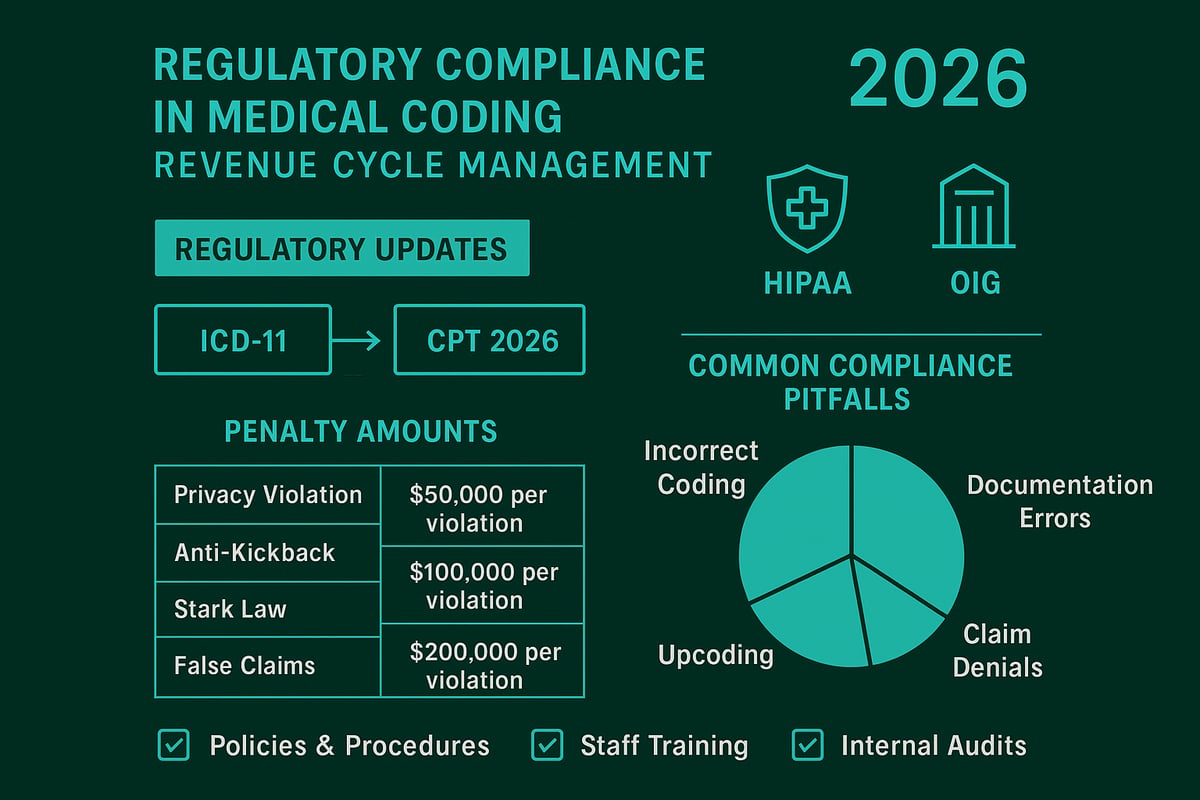
Navigating regulatory compliance in medical coding revenue cycle management is more complex than ever in 2026. Healthcare organizations must keep pace with evolving standards like ICD-11, CPT 2026, and shifting payer rules. Failing to comply can have severe financial consequences, with regulatory penalties often exceeding $1.5 million per violation.
Staying ahead requires a proactive approach. Leaders must ensure that every aspect of their medical coding revenue cycle management process aligns with the latest requirements. This includes accurate coding, timely billing, and robust documentation practices.
Key Regulatory Changes and Industry Standards
The adoption of ICD-11 is a major development for medical coding revenue cycle management this year. The World Health Organization’s 2025 update to ICD-11 introduces new codes and classifications, demanding that coders and billing teams stay current.
CPT 2026 brings additional revisions, while private and government payers frequently update their requirements. These changes affect claim submission formats, pre-authorization protocols, and documentation standards.
Healthcare organizations that do not update their processes risk increased denials, delayed payments, and audit exposure. Integrating these updates into medical coding revenue cycle management workflows is essential for maintaining compliance and profitability.
HIPAA, OIG, and State Regulations
Compliance goes beyond coding updates. HIPAA safeguards patient data privacy, while the Office of Inspector General (OIG) issues guidelines to prevent fraud, waste, and abuse. State-specific regulations can add another layer of complexity to medical coding revenue cycle management.
Consider the following summary of key regulations and potential penalties:
| Regulation | Focus Area | Potential Penalty per Violation |
|---|---|---|
| HIPAA | Data privacy | Up to $1.5 million |
| OIG Guidelines | Fraud prevention | Civil/Criminal penalties |
| State Laws | Billing practices | Varies by state |
Ensuring that all staff understand these requirements is critical for effective medical coding revenue cycle management.
Value-Based Care and Quality Reporting
The shift to value-based care continues to impact medical coding revenue cycle management. Providers must now report quality measures and outcomes, not just services rendered. Accurate coding supports this transition by capturing clinical complexity and risk adjustment factors.
Quality reporting requires a collaborative approach between clinical, coding, and billing teams. Clear communication and well-defined processes help prevent errors and support compliance.
Audit Readiness and Minimizing Risks
Regulatory audits are on the rise. A robust audit readiness strategy is vital for medical coding revenue cycle management. This includes:
- Conducting regular internal audits
- Maintaining detailed documentation
- Using standardized coding protocols
- Training staff on the latest compliance updates
Common pitfalls include incomplete documentation, incorrect code selection, and missed payer updates. Proactive reviews and ongoing training reduce the risk of penalties and lost revenue.
Continuous education and strong internal controls are non-negotiable for B2B healthcare organizations. Investing in compliance not only safeguards finances but also builds trust with partners and payers.
Measuring and Optimizing RCM Performance
A robust approach to measuring and optimizing medical coding revenue cycle management is essential for healthcare providers aiming to thrive in 2026. With industry standards evolving, understanding what to measure and how to improve ensures sustained financial health and compliance.
Identifying and Tracking RCM KPIs
The foundation of effective medical coding revenue cycle management is a clear understanding of key performance indicators. The most critical KPIs for 2026 include clean claim rate, days in accounts receivable (A/R), denial rate, and net collection rate.
Here is a quick summary of each KPI:
| KPI | Definition | Industry Benchmark (2026) |
|---|---|---|
| Clean Claim Rate | % of claims paid on first submission | 95-98% |
| Days in A/R | Avg. time to collect payments | < 30 days |
| Denial Rate | % of claims denied by payers | < 5% |
| Net Collection Rate | % of collectible payments received | 96-99% |
Consistently monitoring these metrics helps organizations set realistic benchmarks, identify bottlenecks, and maintain a competitive edge in medical coding revenue cycle management.
Leveraging Analytics for Performance Optimization
Advanced analytics are transforming how organizations approach medical coding revenue cycle management. Real-time dashboards, predictive analytics, and custom reporting make it possible to detect trends and intervene before issues escalate.
Utilizing Healthcare Revenue Cycle Analytics enables teams to drill down into claim-level data, analyze denial patterns, and forecast cash flow. Automated alerts can flag anomalies, such as spikes in denial rates or delays in payment posting, allowing for rapid corrective action.
By leveraging these tools, providers can pinpoint root causes of revenue leakage and implement targeted solutions. This data-driven approach ensures medical coding revenue cycle management remains agile and responsive to industry changes.
Continuous Improvement and Reporting
Sustained success in medical coding revenue cycle management depends on a culture of continuous improvement. Regular audits, workflow reviews, and staff training are essential for keeping processes efficient and compliant.
Effective strategies include:
- Conducting monthly claim denial analyses
- Holding cross-functional meetings to resolve recurring issues
- Updating documentation practices in response to payer feedback
Transparent reporting provides stakeholders with actionable insights, supporting informed financial decision-making. Industry data shows that practices reducing denials by 40% through targeted interventions outperform competitors and maintain stronger cash flow.
Benchmarking against national standards, as highlighted in U.S. RCM market projections, helps organizations measure progress and set realistic goals.
Conclusion
Staying ahead in medical coding revenue cycle management requires a proactive approach to measurement, optimization, and reporting. By focusing on the right KPIs, leveraging analytics, and committing to continuous improvement, healthcare practices can drive financial performance and ensure compliance in 2026.
Emerging Trends and the Future of Medical Coding RCM
Staying ahead in the world of medical coding revenue cycle management requires keen attention to emerging trends and future developments. As the healthcare landscape evolves, providers must adapt strategies to secure financial performance and compliance in 2026 and beyond.
Artificial Intelligence and Automation Shape RCM
Artificial intelligence and machine learning are transforming medical coding revenue cycle management by enhancing coding accuracy, claim scrubbing, and denial prediction. Advanced algorithms process large volumes of clinical data, identify coding patterns, and flag potential errors before claims submission.
Automated tools also streamline repetitive tasks, allowing RCM professionals to focus on complex cases and exception management. According to industry reports, automation can reduce claim processing times by up to 50 percent, boosting the efficiency of medical coding revenue cycle management for B2B healthcare organizations.
Value-Based Care Reshapes Financial Models
The shift toward value-based reimbursement is fundamentally changing medical coding revenue cycle management. Payers now reward quality outcomes and patient satisfaction rather than just service volume. This requires RCM teams to accurately code for risk adjustment, chronic care, and quality measures.
Staying current with coding standards, such as ICD-11 and CPT updates, is essential for capturing the full value of care delivered. For a deeper understanding of coding types that impact RCM, see Different Types of Medical Coding.
Patient Engagement and Transparency Take Center Stage
Patient financial engagement is increasingly important in medical coding revenue cycle management. As patients take on higher deductibles and out-of-pocket expenses, transparent billing and real-time communication are vital.
Providers are adopting digital payment tools and clear financial policies to improve patient satisfaction and collection rates. A focus on education and proactive outreach can reduce confusion, speed up payments, and support long-term relationships between providers and patients.
Telehealth and Evolving Regulations
The expansion of telehealth services brings new challenges to medical coding revenue cycle management. Virtual visits require precise coding and documentation to meet payer requirements and ensure proper reimbursement.
Regulatory trends, including the adoption of ICD-11, will further impact coding practices and compliance. The AHA’s response on ICD-11 adoption highlights key considerations for U.S. providers preparing for these changes. Adapting to new payer expectations and maintaining audit readiness will be critical in 2026.
Staying Future-Ready: Recommendations
To excel in medical coding revenue cycle management, healthcare organizations should invest in ongoing staff training, leverage automation, and monitor regulatory updates. Strategic partnerships with experienced RCM service providers can provide the expertise needed to navigate emerging trends.
Industry forecasts predict the global RCM market will reach $160 billion by 2026, reflecting the growing importance of future-ready solutions. By embracing innovation, fostering adaptability, and prioritizing compliance, providers can secure financial health in a rapidly changing environment.
As we look ahead to 2026, staying ahead of new coding standards, evolving regulations, and the latest RCM technologies is essential for your practice’s financial success. Navigating these changes can feel overwhelming, but you don’t have to do it alone. Greenhive Billing Solutions combines proven expertise, transparent communication, and a commitment to HIPAA compliance to help practices like yours boost reimbursements and streamline operations. If you’re ready to take the next step toward optimizing your revenue cycle and ensuring lasting financial health, let’s connect—Book Your Free Consultation today.