Accurate use of the cpt code for suture removal is critical for healthcare organizations seeking proper reimbursement and regulatory compliance. Coding errors can result in costly denials or lost revenue, putting financial stability at risk.
This guide delivers a clear, updated perspective on suture removal billing, with a focus on 2026 changes, CPT basics, E/M coding, real-world billing scenarios, and documentation strategies. Discover how to streamline your billing process, minimize errors, and protect your revenue with expert insights tailored for medical professionals.
Understanding CPT Codes and Their Role in Medical Billing
CPT codes are the backbone of medical billing, ensuring that every service provided by a healthcare professional is translated into a standardized language for payers. These numeric codes allow clinics and organizations to communicate clearly with insurers, streamlining claims and supporting timely reimbursement. Without the accuracy provided by CPT codes, even a simple service like the cpt code for suture removal could result in confusion and delayed payments.
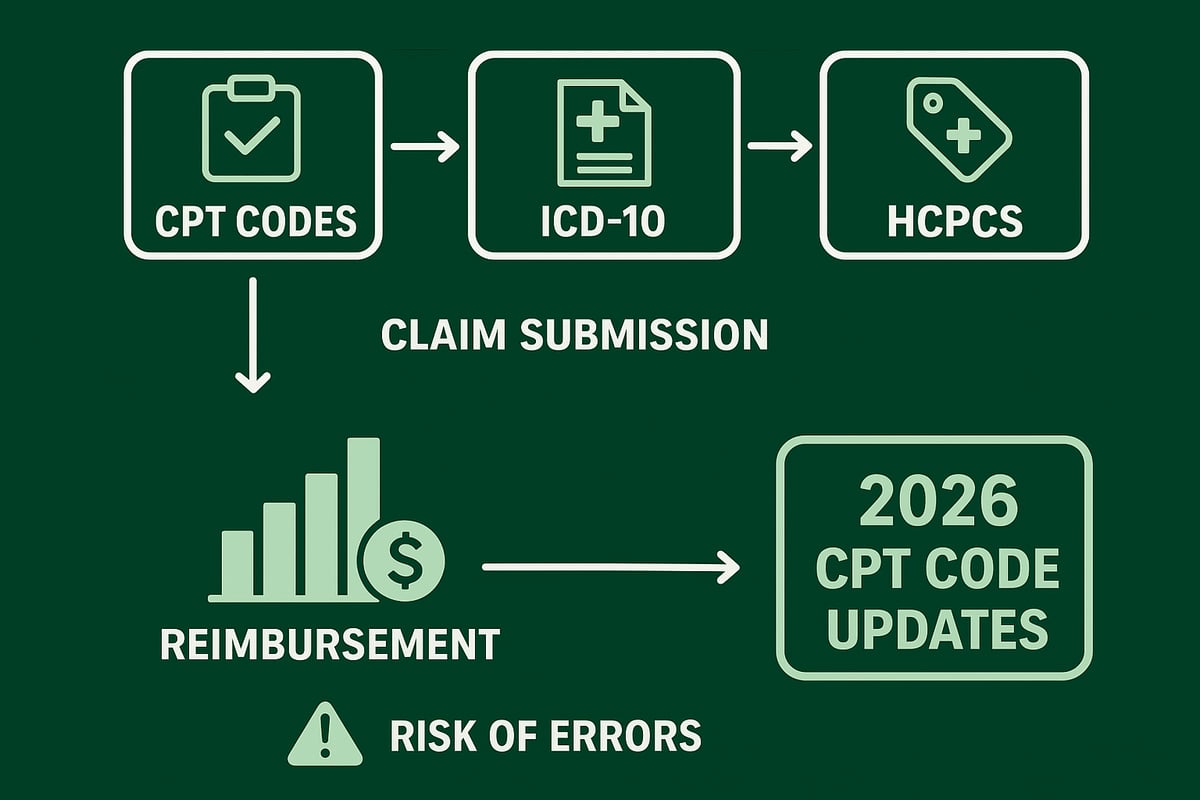
What Are CPT Codes and Why Are They Important?
CPT codes, or Current Procedural Terminology codes, are a set of medical codes used to describe procedures and services performed by healthcare professionals. They provide a universal language that all payers and providers understand. For example, when billing for the cpt code for suture removal, clinics rely on the correct code to ensure prompt and full reimbursement.
These codes are essential because they standardize medical billing, reduce ambiguity, and help avoid costly mistakes. For a detailed overview of their foundational role in claims, see CPT codes in healthcare claims.
Who Manages CPT Codes?
The American Medical Association (AMA) is responsible for maintaining and updating CPT codes. Each year, the AMA evaluates new technologies, procedures, and billing needs to update the code set. This ensures that the system remains current and relevant to providers’ needs, including the cpt code for suture removal as procedures and payer requirements evolve.
Oversight by the AMA means that codes are consistent across the industry, supporting compliance and reducing audit risks for clinics and organizations.
CPT, ICD-10, and HCPCS: The Coding Triad
Medical billing relies on three major code sets: CPT, ICD-10, and HCPCS. Each serves a unique purpose:
| Code Set | Purpose | Example Use |
|---|---|---|
| CPT | Describes procedures/services | cpt code for suture removal |
| ICD-10 | Diagnoses | Wound infection |
| HCPCS | Supplies, drugs, non-physician services | Durable medical equipment |
These code sets work together to create a complete picture of the patient encounter, ensuring accurate billing and supporting claims for services like suture removal.
The Impact of CPT Codes on Revenue Cycle Management
Accurate CPT code usage is critical for the financial health of clinics and healthcare organizations. Errors, such as using the wrong cpt code for suture removal, can result in claim denials, underpayments, or even compliance violations. For example, if a procedure is coded incorrectly, payers may reject the claim or bundle it with other services, impacting revenue.
Common errors include:
- Selecting outdated codes
- Missing required modifiers
- Failing to match diagnoses and procedures
- Incomplete documentation
Each of these can disrupt the revenue cycle and require additional resources for correction and appeals.
2026 Trends and the Value of Ongoing Staff Education
The medical billing landscape is dynamic, with annual updates to the CPT code set. In 2026, new codes and revisions are being introduced, reflecting shifts in outpatient procedures and payer expectations. Staying current is essential, especially when using the cpt code for suture removal, as payers may change their policies or documentation requirements.
Ongoing staff education is vital. Regular training ensures billing teams understand the latest coding changes, reducing errors and supporting compliance. Clinics that invest in education and process improvement position themselves for greater financial stability and fewer denied claims.
Suture Removal: Clinical Overview and Billing Challenges
Suture removal is a routine yet crucial part of patient care in outpatient, emergency, and primary care settings. Providers encounter suture removal in diverse clinical scenarios, such as follow-up visits after surgery, wound management in urgent care, and post-injury care in family medicine. Every healthcare organization must understand the correct process for coding and billing these encounters, as the cpt code for suture removal is often misunderstood or misapplied.
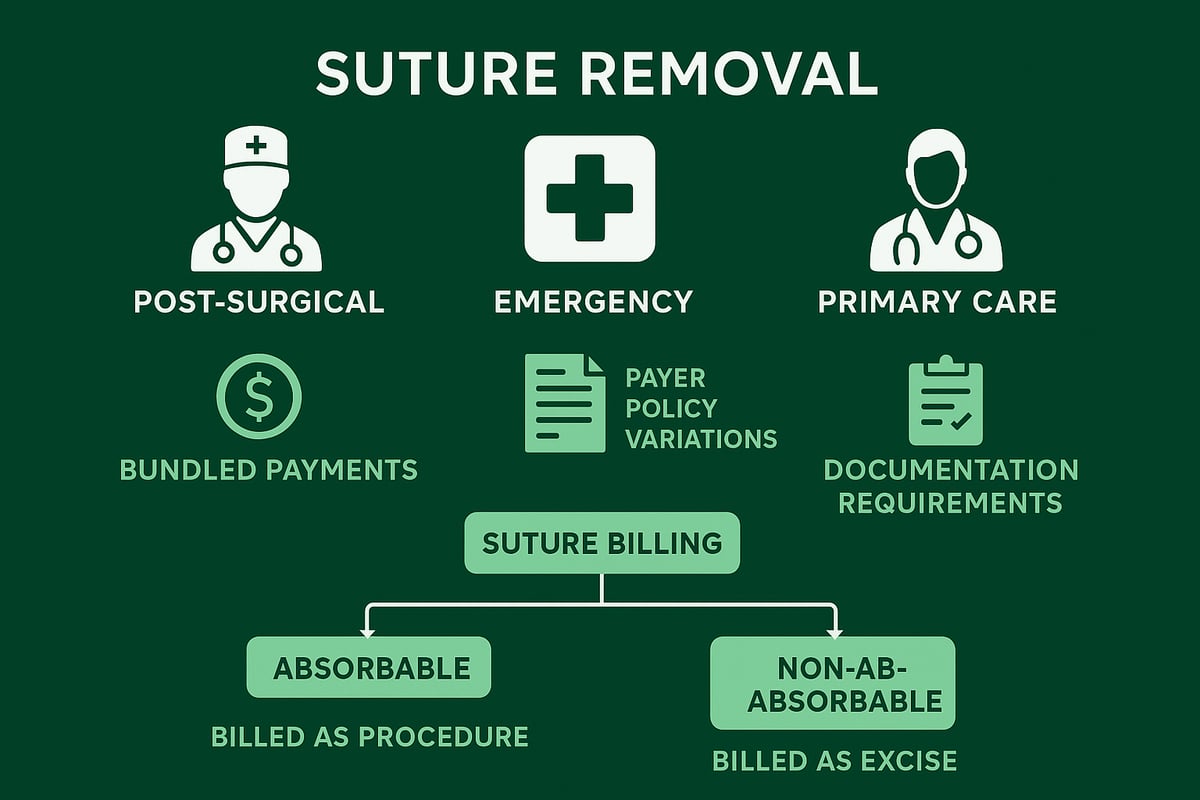
One key distinction in suture management is between absorbable and non-absorbable sutures. Absorbable sutures break down naturally and rarely require removal, so billing for their removal is unusual. Non-absorbable sutures, however, require active removal and trigger specific billing considerations. The cpt code for suture removal depends on suture type, location, and provider involvement, making precise documentation critical for compliance and reimbursement.
Billing for suture removal presents several challenges. Many practices are surprised to learn there is no single, dedicated cpt code for suture removal in most situations. Instead, removal is often considered part of a bundled service, particularly if it occurs during the global period of a procedure. Variations in payer policies add further complexity, as Medicare, Medicaid, and commercial insurers may each interpret the cpt code for suture removal differently. For a detailed breakdown of recent code changes and practical billing advice, refer to A guide to the new codes for suture/staple removal.
The global surgical package is a major factor impacting reimbursement for suture removal. If a patient returns to the surgeon’s office within the global period, removal is generally included in the original procedure payment and is not separately billable. However, if another provider performs the removal outside the global period, the encounter may qualify for an evaluation and management (E/M) code. This highlights the importance of knowing when the cpt code for suture removal can be appropriately used and how payer rules differ depending on location and provider.
Improper billing for suture removal can lead to lost revenue and compliance risks, including claim denials and audits. In 2026, regulatory attention to minor procedure billing and documentation is expected to intensify, with increased scrutiny from payers and auditors. Staying current with updates to the cpt code for suture removal and investing in ongoing staff education are essential steps for maintaining revenue integrity and minimizing compliance exposure.
Coding for Suture Removal: Step-by-Step Guide
Accurately coding for suture removal is essential for healthcare organizations to secure proper reimbursement and maintain compliance. This step-by-step guide breaks down the process for applying the correct cpt code for suture removal, ensuring your billing team captures every detail. Each step addresses critical compliance points relevant to 2026, minimizing risk and optimizing your revenue cycle.
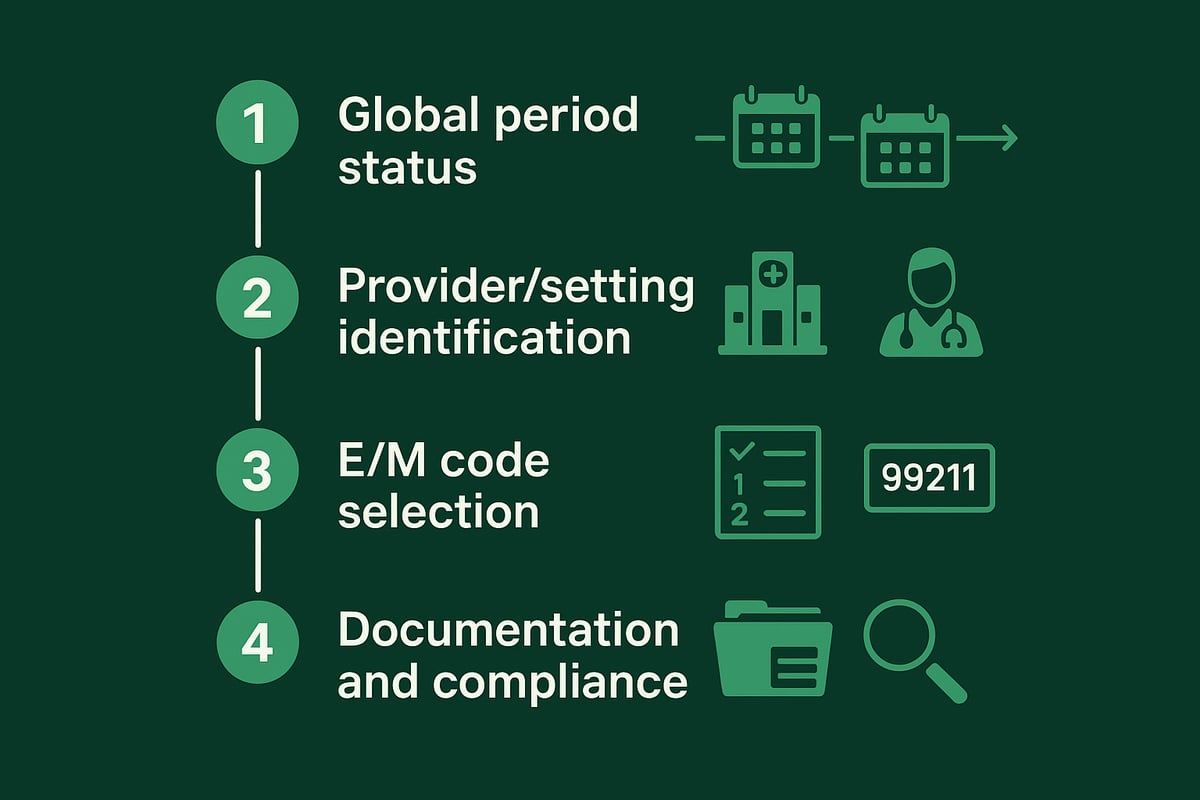
Step 1: Determine Surgical Global Period Status
The first step in coding for suture removal is understanding the surgical global period. The cpt code for suture removal may be bundled or separately billable depending on timing. The global period is a set timeframe after surgery (0, 10, or 90 days) during which routine post-operative care, including suture removal, is typically included in the original procedure payment.
To verify if suture removal falls within the global period, check the date of the original surgery and the assigned global period length. For instance, if sutures are removed 7 days after a minor procedure with a 10-day global period, the service is likely bundled and not separately billable.
However, there are exceptions. If a different provider removes the sutures or if unrelated care is provided, modifiers may be needed to clarify billing. Modifiers such as 24 (unrelated E/M during global period), 25 (significant, separately identifiable E/M), or 79 (unrelated procedure during global period) play a crucial role. Understanding how and when to use these modifiers is vital; common mistakes can lead to denials. For a deeper dive on this, see Common errors with medical modifiers.
Proper documentation is necessary to track global periods and support modifier use. Each payer may enforce the global period differently, so always review payer policies before applying any cpt code for suture removal.
Step 2: Identify the Performing Provider and Setting
The next step is determining who is performing the suture removal and where the service takes place. This directly impacts which cpt code for suture removal is appropriate and how reimbursement is handled. If the original surgeon removes the sutures in their office within the global period, billing separately is usually not permitted.
If another provider, such as a primary care physician or urgent care clinician, performs the removal, especially after the global period, separate billing becomes possible. The setting (office, clinic, hospital, ER) also affects reporting and payment.
Consider this example: A patient has surgery at a hospital and returns to a primary care office for suture removal after the global period. The primary care provider may bill using an appropriate E/M code. Coordination of care documentation, such as clear referral or transfer notes, supports billing and compliance.
Always ensure the documentation clearly states the provider, setting, and care context. This protects your organization if the cpt code for suture removal is questioned during an audit or denied by a payer.
Step 3: Select the Appropriate E/M Code
When a standalone cpt code for suture removal is not available, Evaluation and Management (E/M) codes are typically used. Selecting the right E/M code depends on the complexity of the service, decision-making involved, and the time spent.
Common E/M codes for suture removal include:
| Code | Description | Typical Use Case |
|---|---|---|
| 99211 | Minimal service | Simple, nurse visit |
| 99212 | Problem-focused, low complexity | Brief physician encounter |
| 99213 | Expanded problem-focused | More complex or symptomatic |
For instance, a nurse removing sutures with minimal assessment may use 99211, while a physician managing symptoms or complications may select 99212 or 99213. The cpt code for suture removal must align with the documentation of medical necessity, complexity, and provider involvement.
Document all elements required for E/M support, including patient history, examination, and decision-making. Be aware of payer audit triggers, such as upcoding or insufficient notes tied to the cpt code for suture removal.
Step 4: Ensure Accurate Documentation and Compliance
Thorough documentation is the backbone of compliant billing for suture removal. Each record should include the date of the original surgery, wound status, number of sutures removed, and any patient symptoms or complications. This information substantiates the cpt code for suture removal and reduces the risk of denials.
Incomplete or vague documentation is a leading cause of audit findings and claim denials. Integrate best practices by using EHR templates, checklists, and regular staff training. For example, 2025 audit reviews highlighted missing surgery dates and unclear wound assessments as top documentation errors.
To maintain compliance, periodically review staff performance and update training as payer rules evolve. A robust documentation process supports accurate use of the cpt code for suture removal and ensures your organization is prepared for any payer review or audit.
Real-World Scenarios and Case Studies in Suture Removal Coding
Understanding how the cpt code for suture removal is applied in real practice is essential for accurate billing and compliance. Below, we explore common scenarios faced by healthcare organizations and revenue cycle teams, offering insight into coding decisions, claim outcomes, and audit risks.
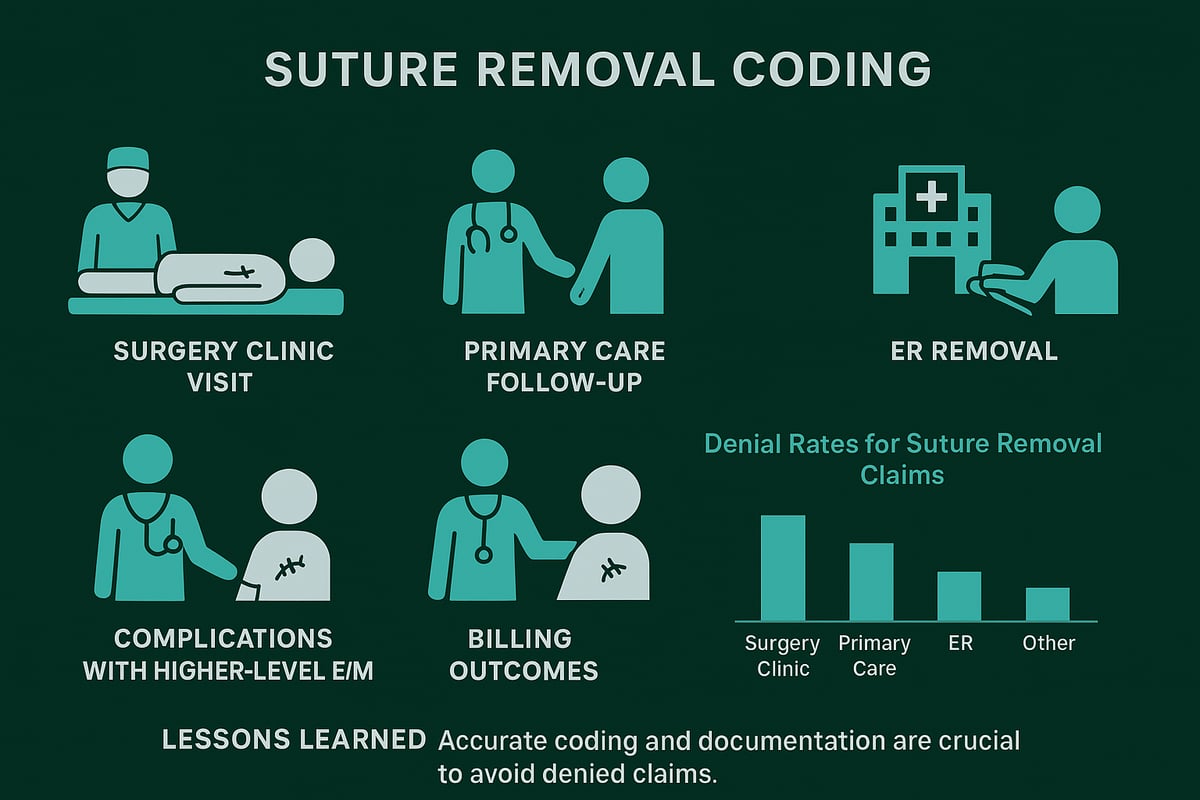
Scenario 1: Suture Removal Within Global Period by Original Surgeon
A patient returns to the surgeon’s office seven days after a procedure for routine suture removal. Because this visit falls within the global surgical period, the cpt code for suture removal is considered bundled with the original surgical procedure. No additional billing is allowed for the removal itself. Documentation should note the visit and removal, but reimbursement is included in the initial payment.
Scenario 2: Suture Removal by a Different Provider After Global Period
A patient sees their primary care physician for suture removal 15 days post-surgery, after the global period has ended. The cpt code for suture removal now allows for billing, typically using an appropriate E/M code. The provider must document the date of the original procedure, wound assessment, and removal details. This scenario increases reimbursement opportunities, provided documentation is complete.
Scenario 3: Emergency Room Suture Removal Bundled with ER Visit
A patient presents to the emergency department for urgent suture removal due to discomfort. The cpt code for suture removal is not billed separately here; instead, the removal is bundled with the ER visit E/M code. Accurate documentation of symptoms and removal is crucial. Denials can occur if attempts are made to unbundle the service improperly.
Scenario 4: Suture Removal in Primary Care for Surgery Performed Elsewhere
A patient who had surgery at a hospital visits their regular primary care clinic for suture removal. The cpt code for suture removal is assigned using the appropriate E/M code, as the provider is not the original surgeon and the global period does not apply. Coordination notes and a clear referral are essential for compliance and successful reimbursement.
Scenario 5: Complications During Suture Removal and Higher-Level E/M Codes
Sometimes, suture removal is complicated by infection or wound dehiscence. In these cases, the cpt code for suture removal can be paired with a higher-level E/M code, reflecting the added complexity. Detailed documentation of the complication and medical decision-making supports the claim and reduces audit risk.
Data: Claim Denials and Audit Lessons
Below is a summary of recent data on claim denials related to the cpt code for suture removal:
| Setting | Denial Rate (%) | Common Denial Reason |
|---|---|---|
| Surgeon’s Office | 4 | Global period bundling |
| Primary Care Clinic | 8 | Incomplete documentation |
| Emergency Department | 6 | Unbundling errors |
Lessons from payer audits highlight the need for:
- Precise global period tracking
- Comprehensive wound and procedure notes
- Correct use of E/M codes for suture removal
For more in-depth strategies to reduce denials, see our guide on Denial management in medical billing.
Staying updated with cpt code for suture removal rules and payer requirements ensures clean claims, fewer denials, and optimized revenue for your practice.
Documentation Best Practices for Suture Removal Billing
Accurate and detailed documentation is vital for correct billing when using the cpt code for suture removal. Proper records not only support claims but also protect your practice from denials and compliance issues. Let us explore the best practices every clinic and healthcare organization should implement.
Key Elements for Documentation
Every encounter involving the cpt code for suture removal must include these elements:
- Patient identification and demographics
- Date and type of original surgery
- Location and status of the wound
- Number and type of sutures removed
- Any complications or symptoms reported
A detailed note ensures the claim accurately reflects the service provided. Missing or incomplete information is a common reason for payer denials.
Tools, Templates, and Checklists
Using standardized templates or checklists streamlines the process and reduces errors. These tools prompt staff to capture every detail needed for the cpt code for suture removal, such as wound healing progress and referral source.
- Pre-built EHR templates
- Printable checklists for minor procedures
- Digital prompts for required fields
Integrating these resources into daily workflows saves time and improves consistency across your team.
Linking Documentation to Code Selection
Documentation must always support the CPT or E/M code chosen. If the cpt code for suture removal is billed as part of a global package, note the surgical date and global period status. For separate E/M coding, include the medical necessity and complexity addressed during the visit.
Review the AMA releases CPT 2026 code set for the latest requirements on documentation supporting new or revised codes. Keeping up with these changes is essential for compliance.
Reducing Denials Through Proactive Documentation
Proactive documentation is your first defense against denials. Regular staff training, internal audits, and clear policies help ensure every cpt code for suture removal is supported by robust records.
- Conduct periodic chart reviews
- Provide feedback on documentation gaps
- Use checklists to verify completeness before claim submission
A 2025 audit showed that incomplete suture removal notes led to a 12% increase in claim denials. Strong documentation helps practices successfully appeal denied claims and maintain steady cash flow.
Compliance, Staff Roles, and 2026 Trends
Assign clear roles for documentation accuracy. Providers, nurses, and billing staff should know their responsibilities. As digital tools advance, consider AI-assisted documentation features that prompt for missing details or flag inconsistencies.
For Medicare and payer-specific compliance, consult the 2026 Complete Table of Contents for current guidelines related to the cpt code for suture removal.
Embracing digital solutions and ongoing staff education positions your practice for success in 2026 and beyond. Accurate documentation is not just a regulatory requirement; it is a foundation for revenue integrity and operational excellence.
The Impact of Proper Suture Removal Coding on Revenue Cycle Management
Accurate use of the cpt code for suture removal is crucial for maintaining revenue integrity in outpatient clinics and healthcare organizations. Even minor discrepancies in coding can delay reimbursements, impact cash flow, and strain provider-payer relationships. When the cpt code for suture removal is applied correctly, claims move smoothly through the adjudication process, reducing the need for time-consuming appeals or corrections.
Coding Accuracy and Financial Outcomes
Using the correct cpt code for suture removal prevents claim denials and underpayments that can erode practice profitability. For example, improper bundling or the use of an incorrect code may result in payers rejecting claims outright, leading to lost revenue and increased administrative costs.
A table summarizing the financial impact:
| Coding Accuracy | Denial Rate | Avg. Reimbursement Time | Revenue Loss (%) |
|---|---|---|---|
| Precise | <5% | 14 days | 0–2% |
| Inaccurate | >15% | 30+ days | 5–10% |
Staff education and regular audits are essential. As outlined in Medical coding service types explained, understanding various coding categories directly influences billing outcomes, especially for minor procedures like suture removal.
Denial Management and Audit Strategies
Proactive denial management is vital for practices that routinely bill the cpt code for suture removal. Regular coding audits detect patterns of error, enabling targeted staff training and process correction before significant revenue leakage occurs.
Key audit steps include:
- Reviewing documentation for completeness and accuracy
- Verifying modifier use when appropriate
- Comparing billed codes to payer-specific guidelines
Practices that implement robust audit cycles see measurable reductions in denial rates and faster payment cycles.
Process Improvement and Education
Continuous education on the cpt code for suture removal helps teams stay current with evolving payer policies and coding regulations. Workshops, coding updates, and scenario-based training sessions foster a culture of accuracy and compliance.
Best practices include:
- Integrating regular feedback from denial trends
- Assigning responsibility for monitoring regulatory updates
- Maintaining clear documentation protocols
These measures ensure teams can adapt quickly to changes, such as new CPT code revisions impacting general surgery and related specialties.
KPIs and Revenue Optimization
Monitoring key performance indicators tied to the cpt code for suture removal is essential for sustained revenue cycle health. Important KPIs to track include:
- Denial rate for minor procedures
- Time to reimbursement (days)
- Percentage of claims paid on first submission
- Number of coding-related appeals
- Audit pass rate
By focusing on these KPIs, organizations can quickly identify bottlenecks and implement targeted improvements, ensuring optimal revenue flow and compliance in suture removal billing.
If you’re feeling the pressure of keeping up with evolving CPT code requirements for suture removal, you’re not alone. Navigating documentation, compliance, and payer variations can be overwhelming, especially with the 2026 updates on the horizon. At Greenhive Billing Solutions, we understand how critical accurate coding is for your practice’s financial health and efficiency. If you want personalized guidance or need help streamlining your revenue cycle, let’s connect and talk through your specific challenges—your peace of mind starts with the right support.
Book Your Free Consultation

