Rising claim denials and reimbursement delays are placing urgent care providers under increasing financial pressure as we approach 2026. The complexity of urgent care revenue cycle management is growing, and operational stress can quickly erode cash flow if not addressed proactively.
This guide delivers a focused roadmap for urgent care operators seeking to master urgent care revenue cycle management in the coming year. Inside, you will find proven strategies covering RCM fundamentals, step-by-step process optimization, technology adoption, compliance essentials, performance measurement, and key trends shaping the future.
Mastering these best practices means faster payments, fewer denials, and sustainable growth for your clinic. Start implementing these actionable insights now to position your urgent care operation for revenue cycle management success in 2026.
Understanding Urgent Care Revenue Cycle Management Fundamentals
Urgent care revenue cycle management is the backbone of financial stability for urgent care clinics. Understanding its fundamentals is crucial for optimizing cash flow, reducing administrative burden, and ensuring sustainable growth. Let’s break down the unique workflow, key stakeholders, and financial impact to set the stage for RCM excellence in 2026.
Defining Revenue Cycle Management in Urgent Care
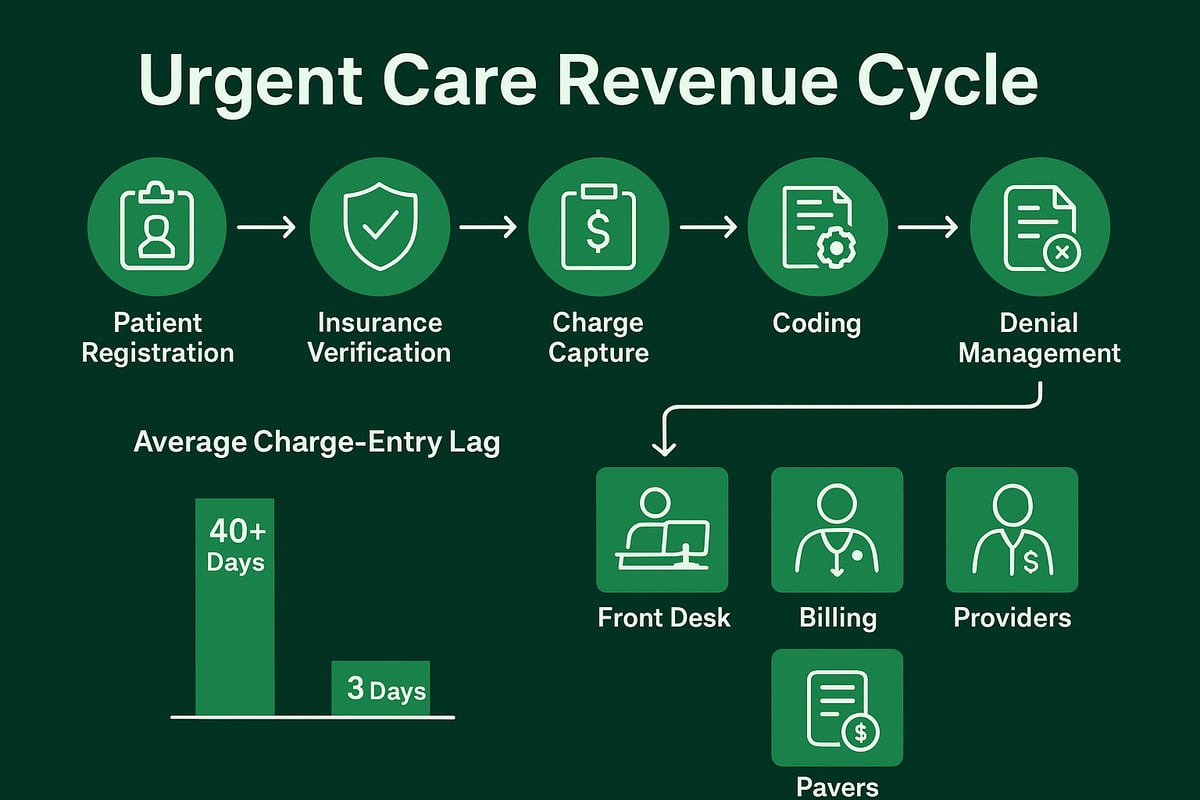
Urgent care revenue cycle management begins the moment a patient enters the clinic and continues through final payment collection. The workflow is designed to accommodate walk-ins, episodic visits, and high patient volumes, making speed and accuracy essential. The core steps include patient registration, insurance verification, charge capture, coding, claims submission, payment posting, and denial management.
Compared to primary care and specialty clinics, urgent care RCM must account for unpredictable patient flow and rapid service delivery. This environment increases the risk of delayed claims, high denial rates, and patient payment challenges. In fact, the average charge-entry lag in urgent care can exceed 40 days without optimized processes, as reported by Athenahealth.
Failing to address these pain points can have real consequences. For example, a clinic with inaccurate registration data and inconsistent eligibility checks may experience repeated claim denials, resulting in significant revenue loss. Leveraging denial management in medical billing strategies is key to minimizing these risks and maintaining a healthy revenue cycle.
Key Stakeholders and Roles in the Urgent Care RCM Process
The urgent care revenue cycle management process relies on collaboration among several key stakeholders. Front desk staff play a pivotal role in patient intake, capturing accurate insurance information, and collecting payments at the point of service. Billing and coding teams ensure that clinical documentation is translated into precise codes, preparing clean claims for submission.
Providers are responsible for delivering high-quality documentation that supports compliant coding and efficient billing. RCM service providers, such as our team, work behind the scenes to manage workflows, adapt to client-owned software, and coordinate with payers. Insurance companies and government programs review and reimburse claims, making payer relationships a vital part of the cycle.
Each stakeholder’s performance directly impacts the efficiency and accuracy of urgent care revenue cycle management. Missteps at any stage, from registration to payment posting, can cascade into delays, denials, or lost revenue.
The Financial Impact of RCM on Urgent Care Operations
Efficient urgent care revenue cycle management directly influences a clinic’s cash flow, staff workload, and ability to expand services. Streamlined RCM processes reduce days in accounts receivable, speed up reimbursements, and lower administrative costs. According to an Athenahealth case study, improving patient pay yield from 43 percent to 95 percent is possible with disciplined RCM practices.
On the other hand, poor RCM can threaten the viability of urgent care operations. Chronic claim denials, delayed payments, and unresolved patient balances increase financial stress and limit growth opportunities. By prioritizing RCM optimization, clinics can protect their bottom line and position themselves for sustainable success in a competitive healthcare landscape.
Step-by-Step Guide to Optimizing the Urgent Care Revenue Cycle in 2026
Optimizing urgent care revenue cycle management is critical for clinics aiming to thrive in 2026’s competitive healthcare environment. Each step in the revenue cycle directly impacts cash flow, operational efficiency, and the patient experience. By following a systematic approach, urgent care operators can minimize denials, accelerate collections, and position their organizations for sustainable growth.
Step 1: Streamlining Patient Registration and Insurance Verification
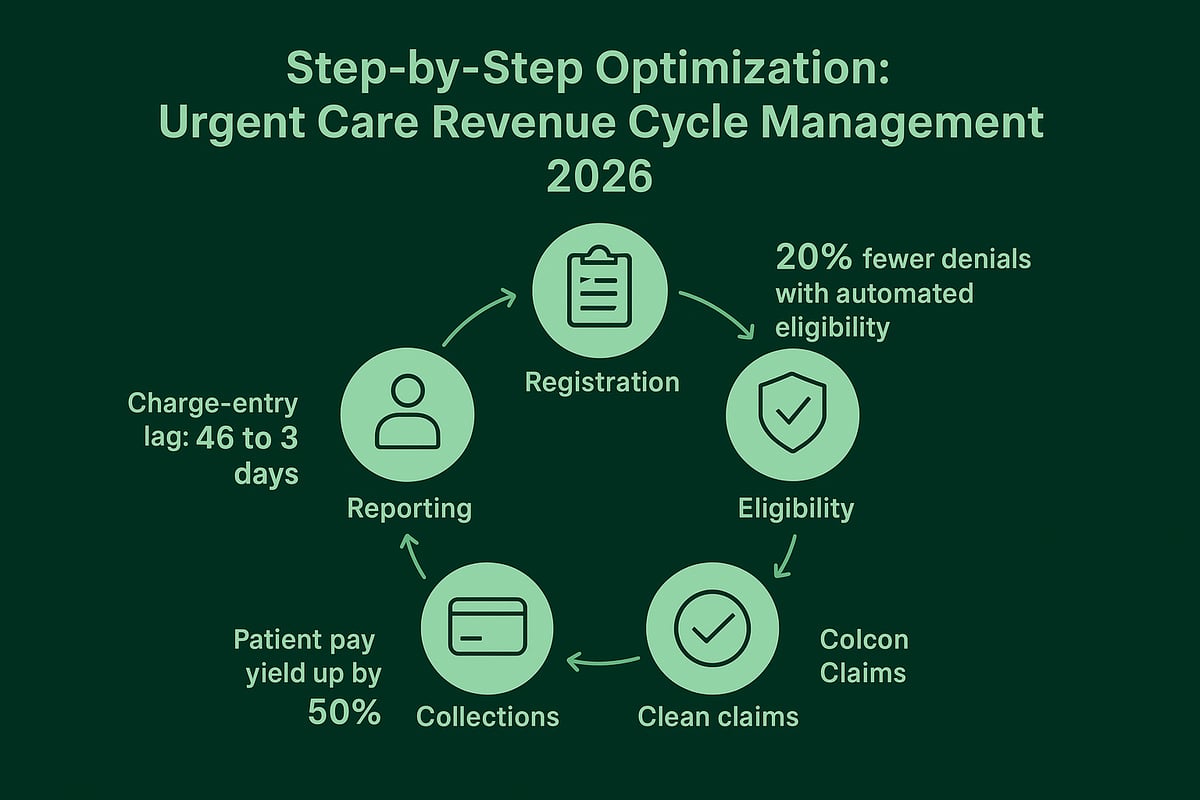
The first step in urgent care revenue cycle management is ensuring accurate patient registration and insurance verification. Front desk staff must capture correct demographic and insurance details from the outset. Real-time eligibility checks are essential for preventing downstream claim denials and reimbursement delays.
Best practices include:
- Using digital intake forms to reduce manual entry errors.
- Implementing automated eligibility tools that verify coverage before care is rendered.
- Training staff to confirm policy status and collect co-pays upfront.
According to industry data, clinics leveraging automated eligibility verification report 20% fewer claim denials. For a deeper dive into optimizing this stage, review the Eligibility verification services overview. By investing in these protocols, urgent care revenue cycle management becomes more efficient right from the start.
Step 2: Efficient Charge Capture and Medical Coding
Accurate and timely charge capture is a cornerstone of effective urgent care revenue cycle management. Providers must document every service rendered, ensuring coding teams have all the information needed for precise claim submission. Certified coders should use current ICD-10, CPT, and HCPCS codes tailored to urgent care procedures.
Frequent coding errors include:
- Upcoding or undercoding visits.
- Missing procedure modifiers.
- Incorrect diagnosis codes.
Ongoing education and routine audits help prevent costly mistakes. Even a single missed or misapplied code can result in lost revenue or compliance risk. Establishing an internal feedback loop between providers and coders is vital for continuous improvement and accuracy.
Step 3: Clean Claims Submission and Claims Management
Submitting clean claims is essential to optimize urgent care revenue cycle management outcomes. A “clean claim” is one that passes payer edits without errors, allowing for first-pass acceptance and faster reimbursement. Clinics should utilize claim scrubbing tools and AI-driven validation to catch issues before submission.
Key practices include:
- Verifying all required data fields are complete.
- Using automated claims engines to reduce charge-entry lag from 46 days to as few as 3.
- Tracking claim status in real time and responding quickly to payer edits.
A proactive approach to claims management shortens payment cycles and decreases administrative burden, ensuring the clinic’s financial health.
Step 4: Payment Posting and Patient Collections
Accurate, real-time payment posting is at the heart of urgent care revenue cycle management. Both insurance payments and patient balances must be recorded promptly to keep accounts current. Collecting patient balances at the point of service is highly effective, especially when supported by card-on-file and digital payment solutions.
Strategies to boost patient pay yield include:
- Offering multiple payment options (credit card, ACH, mobile).
- Sending automated reminders for outstanding balances.
- Training staff to discuss financial responsibility transparently.
Case studies show that implementing card-on-file automation can increase patient pay yield by over 50%. Improved collections reduce aged receivables and strengthen overall cash flow.
Step 5: Denial Management and Appeals
No urgent care revenue cycle management process is complete without robust denial management and appeals procedures. Systematic tracking and analysis of denials allow clinics to pinpoint root causes and implement targeted solutions.
Effective denial management steps:
- Categorize denials by type (eligibility, coding, authorization).
- Conduct root cause analysis to prevent repeat issues.
- Develop a workflow for timely appeals and follow-ups.
Continuous monitoring reveals patterns, enabling staff to refine front-end processes and reduce future denials. Quick, organized appeals can recover significant lost revenue, protecting the clinic’s bottom line.
Step 6: Accounts Receivable Management and Reporting
Strong accounts receivable (A/R) management and transparent reporting are final pillars of urgent care revenue cycle management. Clinics should monitor A/R aging, set clear collection benchmarks, and use dashboards to visualize performance.
Essential KPIs to track include:
- Clean claims rate
- Denial rate
- Days in A/R
- Patient pay yield
- Charge-entry lag
Regular performance reviews help identify bottlenecks and areas for improvement. By leveraging actionable data, clinics can make informed decisions, drive accountability, and sustain long-term financial growth.
Leveraging Technology, Automation, and RCM Service Partners
The landscape of urgent care revenue cycle management is transforming rapidly. As clinics scale and patient volumes surge, adopting advanced technology is no longer optional. Instead, it is central to optimizing financial performance, minimizing errors, and ensuring compliance. In this section, we explore how technology, automation, and skilled RCM service partners support urgent care operators in achieving sustainable growth and operational excellence.
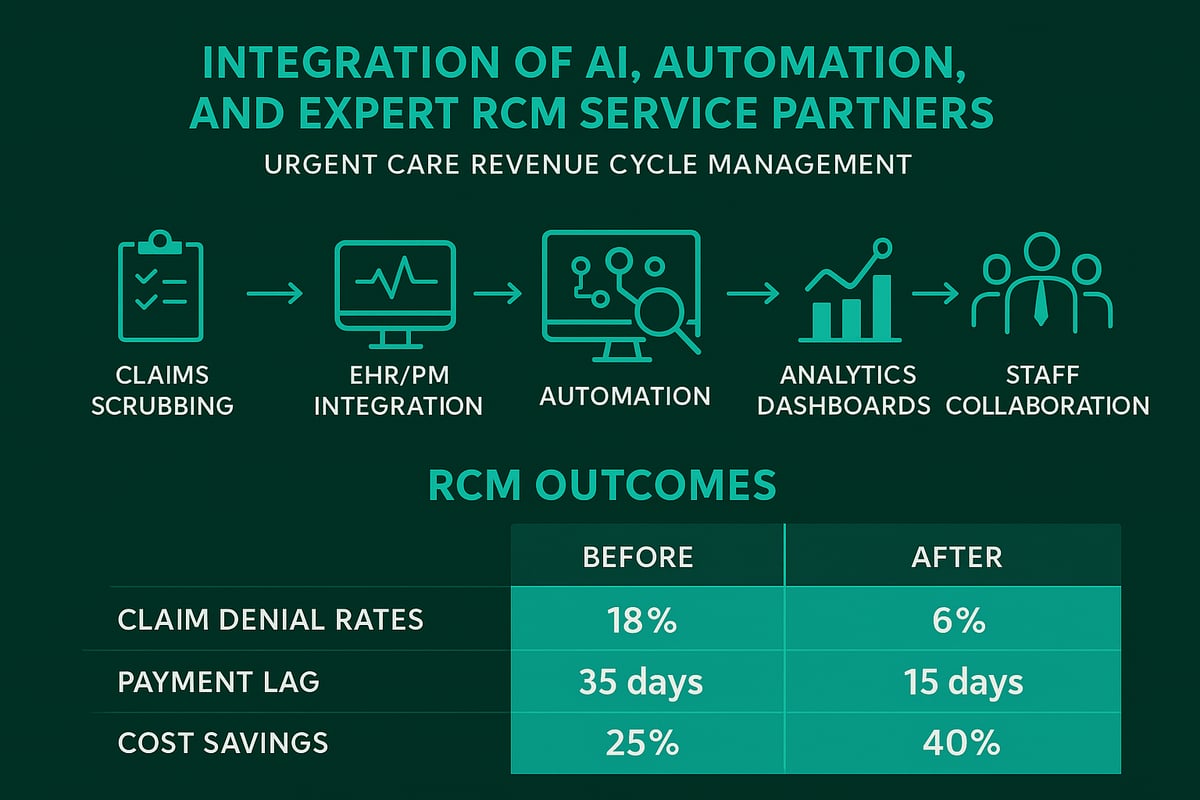
The Role of Technology in Modern Urgent Care RCM
Technology is reshaping every step of urgent care revenue cycle management. AI-powered tools now automate claims scrubbing, reducing manual errors and accelerating claim approvals. Automated workflows support seamless handoffs between front desk, billing, and clinical teams, ensuring that data moves accurately through the cycle.
Integration with EHR and practice management systems streamlines patient information flow, helping urgent care clinics maintain speed and accuracy. Billing workflows can be customized to support hybrid models, such as urgent care with primary care or telehealth, without sacrificing efficiency.
Scalability is another major benefit. As clinics expand to new locations, modern RCM technology ensures consistent processes and reporting across the organization. Using advanced analytics, managers can monitor real-time KPIs and identify areas for improvement. For best practices on submitting clean claims and leveraging automation, see Medical claim submission services.
Selecting the Right RCM Service Provider
Choosing an RCM service provider with urgent care revenue cycle management expertise is crucial. Look for partners with proven experience in the urgent care sector, certified billing and coding staff, and a strong track record of compliance.
Adaptability is key. The best providers work within your existing software and systems, minimizing disruption and leveraging your data for maximum results. Transparent communication and dedicated account management ensure your clinic’s needs are always prioritized.
Many clinics see significant improvements in financial performance after partnering with dedicated experts. These providers not only handle billing and coding but also deliver ongoing support and proactive advice, freeing your team to focus on patient care.
Greenhive Billing Solutions: Expert RCM Services for Urgent Care
Greenhive Billing Solutions specializes in urgent care revenue cycle management for clinics and multi-specialty practices. Our experienced team offers eligibility verification, claims processing, denial management, and a clean claims guarantee, all delivered through secure, HIPAA-compliant workflows.
We tailor our services to each client’s needs, adapting to your systems and processes. With transparent pricing and actionable analytics, clinics gain full visibility into their revenue cycle. Our clients benefit from nationwide support and dedicated account managers who ensure questions are answered and challenges resolved quickly.
The real-world impact is clear. Practices working with Greenhive typically save up to $47,000 annually versus in-house billing, with faster collections and fewer denials. This combination of expertise and technology positions urgent care operators for long-term success in a competitive market.
Best Practices for Technology Adoption and Change Management
Successful urgent care revenue cycle management transformation requires more than just technology. Staff training is essential to ensure everyone understands new tools and workflows. Change management strategies help teams adapt smoothly, reducing resistance and maximizing adoption.
Data security and HIPAA compliance must remain top priorities. End-to-end encryption, secure access controls, and regular risk assessments protect sensitive patient and financial data. Continuous process improvement, fueled by analytics and team feedback, ensures your revenue cycle remains agile and responsive to industry changes.
By investing in staff development and robust security, clinics can fully realize the benefits of RCM technology and service partnerships. This proactive approach safeguards revenue and positions urgent care organizations for future growth.
Compliance, Regulatory Updates, and Risk Mitigation in 2026
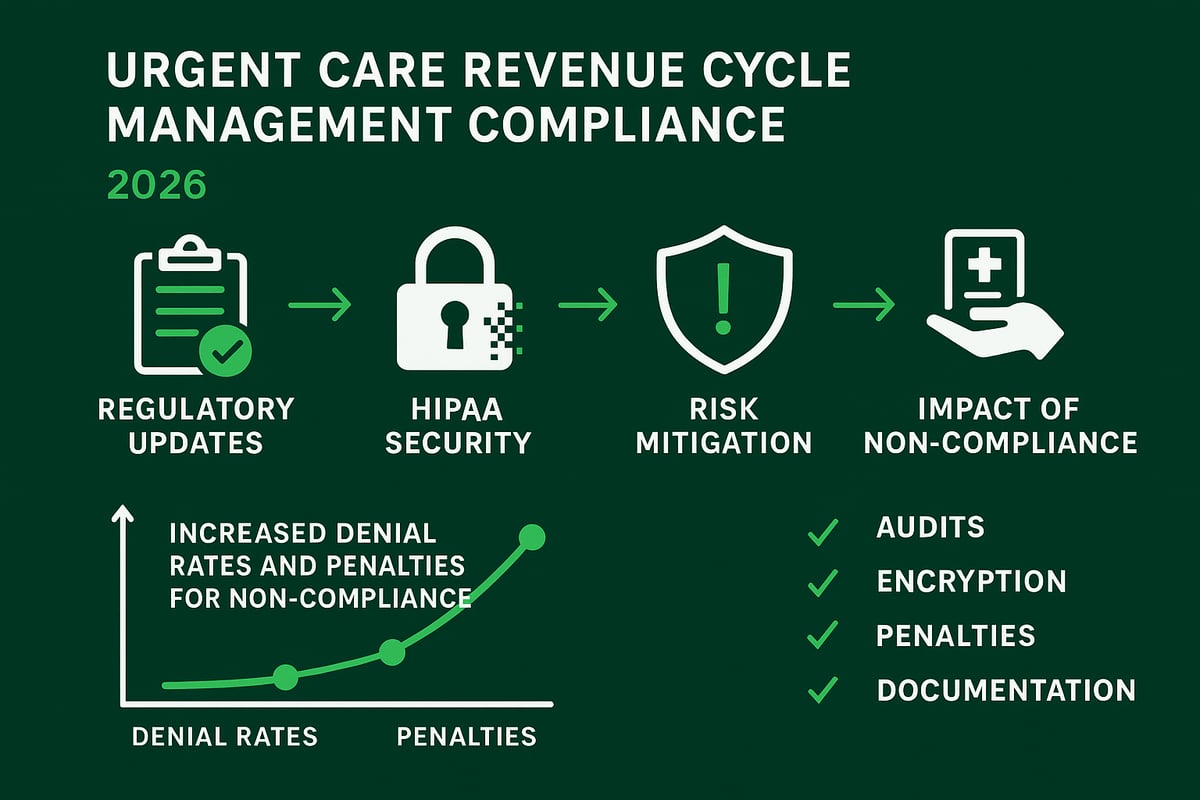
Staying compliant in urgent care revenue cycle management is more complex than ever as regulations evolve in 2026. Providers must proactively monitor changes to payer policies, coding updates, and telehealth billing rules to avoid costly missteps. With the industry trending toward value-based care models, documentation and reporting requirements have become more rigorous.
Regular compliance audits and thorough documentation reviews are essential. Clinics should adapt quickly to new CMS and private payer requirements, leveraging resources like Mastering Revenue Cycle Management for up-to-date best practices. By embedding compliance into every stage of urgent care revenue cycle management, organizations can maintain steady cash flow and minimize risk.
Staying Ahead of Regulatory Changes
The 2026 regulatory landscape for urgent care revenue cycle management is dynamic. Payer policies, coding standards, and telehealth billing requirements continue to shift, impacting reimbursement workflows. Value-based care is gaining traction, requiring urgent care centers to prove quality and efficiency in documentation.
To keep pace, clinics should:
- Conduct routine compliance audits.
- Review documentation standards regularly.
- Monitor CMS and private payer updates.
- Train staff on new billing and coding changes.
Being proactive enables urgent care revenue cycle management teams to minimize errors and optimize reimbursement.
HIPAA and Data Security Essentials
Protecting patient data is at the core of urgent care revenue cycle management. HIPAA compliance demands end-to-end encryption, secure data storage, and regular risk assessments. Staff must be trained on privacy protocols and breach prevention to safeguard sensitive information.
Key data security steps include:
- Using encrypted communication channels.
- Storing records on secure, access-controlled platforms.
- Providing regular HIPAA training for all staff.
- Developing incident response plans for potential breaches.
These measures ensure urgent care revenue cycle management processes remain secure and compliant.
Avoiding Common Compliance Pitfalls
Urgent care revenue cycle management faces recurring compliance risks. Incomplete documentation and coding mistakes can trigger denials or audits. Missed eligibility or authorization checks lead to claim rejections. Outdated payer contracts and fee schedules often result in underpayments.
To avoid these pitfalls, clinics should:
- Standardize documentation templates.
- Employ certified coders and conduct regular audits.
- Verify eligibility at every patient encounter.
- Update payer contracts and fee schedules annually.
Addressing these areas strengthens urgent care revenue cycle management and reduces the likelihood of compliance failures.
The Cost of Non-Compliance
Non-compliance in urgent care revenue cycle management carries significant financial and reputational consequences. Practices may face hefty fines, delayed reimbursements, and increased denial rates. Regulatory scrutiny can also damage provider reputation, eroding patient and payer trust.
For example, clinics with unresolved compliance issues have seen a spike in denials and lost revenue. Investing in compliance protocols not only prevents penalties but also supports long-term operational stability and growth. Prioritizing compliance is essential for the ongoing success of urgent care revenue cycle management.
Measuring, Monitoring, and Improving RCM Performance
Staying competitive in urgent care revenue cycle management requires rigorous performance measurement, actionable monitoring, and a relentless focus on improvement. By leveraging the right KPIs, data-driven insights, and continuous feedback, urgent care operators can boost collections, reduce denials, and streamline workflows for 2026 and beyond.
Key Performance Indicators (KPIs) for Urgent Care RCM
To optimize urgent care revenue cycle management, every clinic should monitor a core set of KPIs. These metrics provide a snapshot of financial health and uncover areas that need attention. The most impactful KPIs include clean claims rate, denial rate, days in accounts receivable (A/R), patient pay yield, and charge-entry lag.
Below is a table summarizing standard benchmarks for urgent care centers:
| KPI | Industry Benchmark | Description |
|---|---|---|
| Clean Claims Rate | 95%+ | Percentage of claims accepted on first pass |
| Denial Rate | <5% | Percentage of total claims denied |
| Days in A/R | <30 days | Average time to collect payment |
| Patient Pay Yield (PPY) | 90-95% | Collected patient responsibility |
| Charge-Entry Lag | <3 days | Time from service to claim entry |
Using advanced healthcare revenue cycle analytics empowers leaders to track these KPIs in real time, quickly identify trends, and act before issues escalate. Consistently reviewing these indicators is essential for urgent care revenue cycle management success.
Data-Driven Decision Making
Data is the foundation for driving operational change in urgent care revenue cycle management. By analyzing KPI trends, clinics can pinpoint bottlenecks, such as spikes in denial rates or delays in posting payments. Monthly performance reviews, supported by visual dashboards, help stakeholders spot recurring issues and prioritize solutions.
Root cause analysis plays a critical role in understanding persistent problems. For example, if days in A/R suddenly increase, leaders can drill down to see if payer response times or coding errors are to blame. Incorporating insights from industry sources, such as the U.S. Revenue Cycle Management Market Report 2025, ensures urgent care groups remain aligned with national trends and regulatory expectations.
Proactive data utilization enables clinics to adjust workflows, update payer strategies, and maintain a competitive edge in urgent care revenue cycle management.
Continuous Improvement Strategies
Achieving excellence in urgent care revenue cycle management demands an ongoing commitment to process refinement. Regular staff training and coding audits help teams stay current with compliance requirements and payer updates. Establishing feedback loops among the front desk, billing, and providers ensures that errors are quickly corrected and best practices are shared.
Top-performing clinics adopt new technologies, such as automated eligibility checks and claim scrubbing, to further reduce manual errors. Benchmarking against industry leaders provides valuable perspective. For instance, one urgent care practice improved its patient pay yield from 43% to 95% after optimizing its revenue cycle processes.
To sustain growth, organizations must foster a culture of continuous improvement, leveraging data, teamwork, and innovation to navigate the evolving healthcare landscape.
Future Trends and Innovations in Urgent Care Revenue Cycle Management
Urgent care revenue cycle management is on the brink of significant transformation as we approach 2026. The industry is experiencing rapid growth, with evolving patient expectations and payer demands. Operators must stay proactive to remain competitive and profitable. According to the U.S. Urgent Care Centers: Growth & Outlook report, urgent care centers continue to expand, creating new opportunities and challenges for revenue cycle optimization.
AI and Automation: The Next Frontier
Artificial intelligence is revolutionizing urgent care revenue cycle management. Predictive analytics now help clinics forecast denials and payment delays, allowing for proactive interventions. Automated coding and claims management streamline workflows, reducing manual errors and freeing staff to focus on higher-value tasks. AI-driven patient engagement tools offer self-service billing and reminders, improving collections. These innovations are essential for handling higher patient volumes and complex payer requirements in urgent care revenue cycle management.
Value-Based Care and Alternative Payment Models
The shift from fee-for-service to value-based reimbursement is accelerating. Urgent care revenue cycle management must adapt to new documentation, coding, and reporting standards. Clinics are preparing for bundled payments and outcome-based incentives, which require precise tracking of clinical quality and patient outcomes. Success in this environment means aligning care delivery with financial performance, ensuring that urgent care revenue cycle management supports both patient satisfaction and fiscal health.
Telehealth and Hybrid Care Models
Telehealth remains a vital part of urgent care service delivery. Integrating virtual visits into urgent care revenue cycle management presents unique challenges, such as accurate coding for remote encounters and managing payer requirements for telehealth claims. Hybrid care models demand flexible workflows and billing expertise. Operators who streamline telehealth within their revenue cycle will be better positioned to capture revenue and meet changing patient preferences.
Patient Financial Experience and Transparency
Patients expect clarity and convenience in their financial interactions. Upfront cost estimates, digital payment options, and transparent billing are now essential elements of urgent care revenue cycle management. Enhancing the patient experience reduces bad debt and increases satisfaction. Clinics are adopting mobile payment platforms, automated reminders, and real-time eligibility checks to meet these expectations and improve financial performance.
Preparing for the Future: Action Steps for 2026 and Beyond
To thrive in 2026, urgent care operators must invest in scalable, adaptable urgent care revenue cycle management processes. Regularly updating policies, technology, and staff training is critical. Fostering a culture of compliance, innovation, and continuous improvement will ensure long-term success. Building strong partnerships with experienced RCM service providers and leveraging analytics will position clinics to navigate industry changes with confidence.
As we look ahead to 2026, you’ve seen just how vital a streamlined revenue cycle is for urgent care success—from timely insurance verification to minimizing denials and optimizing collections. If you’re ready to apply these strategies and want a partner who truly understands the unique challenges of urgent care RCM, let’s connect. At Greenhive Billing Solutions, we’re here to help you boost efficiency, maximize reimbursements, and future proof your operations with personalized support and transparent communication.
Take the next step toward financial clarity and sustainable growth—Book Your Free Consultation today.

