Rising administrative demands and shifting regulations are making medical billing costs a critical concern for healthcare providers in 2026. As financial pressures and compliance requirements intensify, understanding every facet of medical billing costs is essential for maintaining a healthy revenue cycle.
This guide breaks down the key components, emerging trends, and proven strategies around medical billing costs, equipping your organization with the knowledge to optimize financial performance. We will explore cost structures, the factors that influence expenses, regulatory changes shaping the landscape, cost management tactics, and what the future holds.
Ready to turn complexity into opportunity? Let’s uncover practical steps to control costs and improve your bottom line.
Understanding Medical Billing Cost Structures in 2026
Navigating medical billing costs in 2026 requires a clear grasp of how expenditures are structured and allocated. Transparency is essential for healthcare organizations aiming to optimize financial performance and make informed decisions. The following sections break down the critical components, models, and trends shaping cost structures this year.
Components of Medical Billing Costs
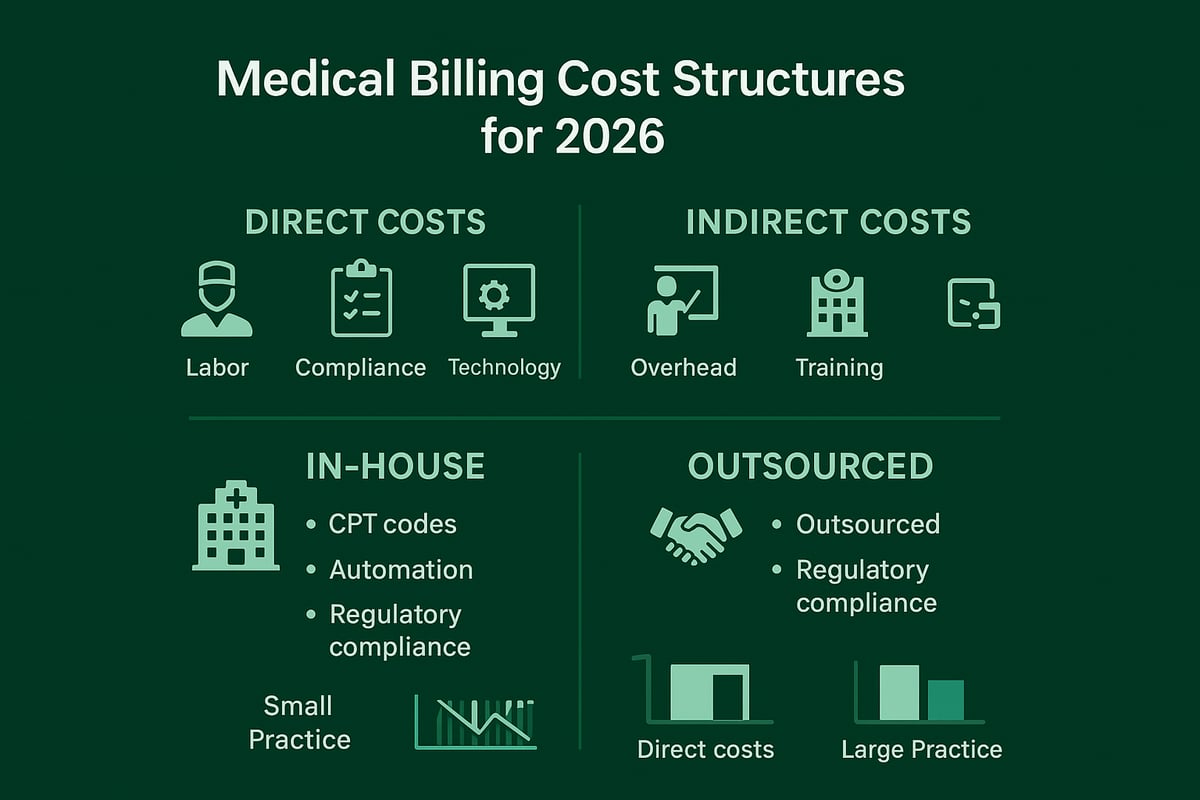
Medical billing costs consist of both direct and indirect expenses. Direct costs include labor for billing staff, technology platforms, and compliance-related activities. Indirect costs involve overhead, ongoing staff training, and administrative support.
Practices typically choose between in-house and outsourced billing models. Smaller clinics may allocate a higher percentage of costs to labor and software, while larger organizations invest more in compliance and infrastructure. For example, industry benchmarks show in-house medical billing costs can range from 7% to 12% of collections, compared to 4% to 8% for outsourced services.
Factors like CPT code complexity, claim volume, and the adoption of automation significantly impact how costs are distributed. Leveraging advanced tools can reduce manual work and errors, ultimately shifting cost allocations. Transparent cost structures, as outlined in a Medical billing services overview, are vital for accurate budgeting and strategic planning.
In-House vs. Outsourced Billing: Cost Comparison
Comparing in-house and outsourced models reveals distinct differences in medical billing costs. In-house billing requires investment in staff salaries, training, office space, and IT infrastructure. Outsourcing shifts many of these expenses to a third-party provider, often resulting in more predictable costs.
| Expense Category | In-House (Annual) | Outsourced (Annual) |
|---|---|---|
| Staffing & Training | $120,000 | Included |
| Technology/Software | $30,000 | Included |
| Overhead | $25,000 | Minimal |
| Error/Denial Costs | $15,000 | $5,000 |
| Total | $190,000 | $110,000 |
Hidden costs such as staff turnover, claim denials, and resubmissions can drive in-house costs up to 30% higher than outsourcing for some organizations. While outsourcing can reduce errors and provide compliance expertise, it may limit direct control over processes. In 2026, careful assessment of regulatory requirements is crucial when choosing the optimal model.
Hidden and Variable Costs in Medical Billing
Many organizations underestimate the hidden and variable aspects of medical billing costs. These can include:
- Claim resubmissions due to errors or denials
- Ongoing compliance updates and staff retraining
- Intensive payer negotiations and appeals
Payer mix and clinical specialty also drive cost variability. Practices with a higher proportion of complex claims or diverse payer requirements face increased administrative burdens. Failing to account for these costs can disrupt cash flow and expose organizations to compliance penalties. Conducting regular cost audits and tracking key performance indicators ensures accurate forecasting and cost control.
Pricing Models for Billing Services
Medical billing costs are shaped by the pricing models adopted by service providers. Common structures include:
- Percentage of collections (typically 4% to 8%)
- Flat monthly fees for predictable workloads
- Hybrid models combining both approaches
The shift toward value-based care and new reimbursement frameworks is driving the adoption of performance-based pricing, where fees are tied to outcomes like reduced denials or faster collections. This model can improve provider margins but requires clear contract terms and transparency.
When evaluating contracts, healthcare organizations should review service inclusions, clarify any potential hidden fees, and ensure alignment with their business goals. A careful approach to pricing model selection helps protect profitability and ensures scalable, sustainable operations.
Key Factors Influencing Medical Billing Costs in 2026
Understanding the forces shaping medical billing costs in 2026 is essential for healthcare organizations. Multiple factors, from evolving regulations to technological advancements, play a pivotal role in determining operational expenses and financial outcomes.
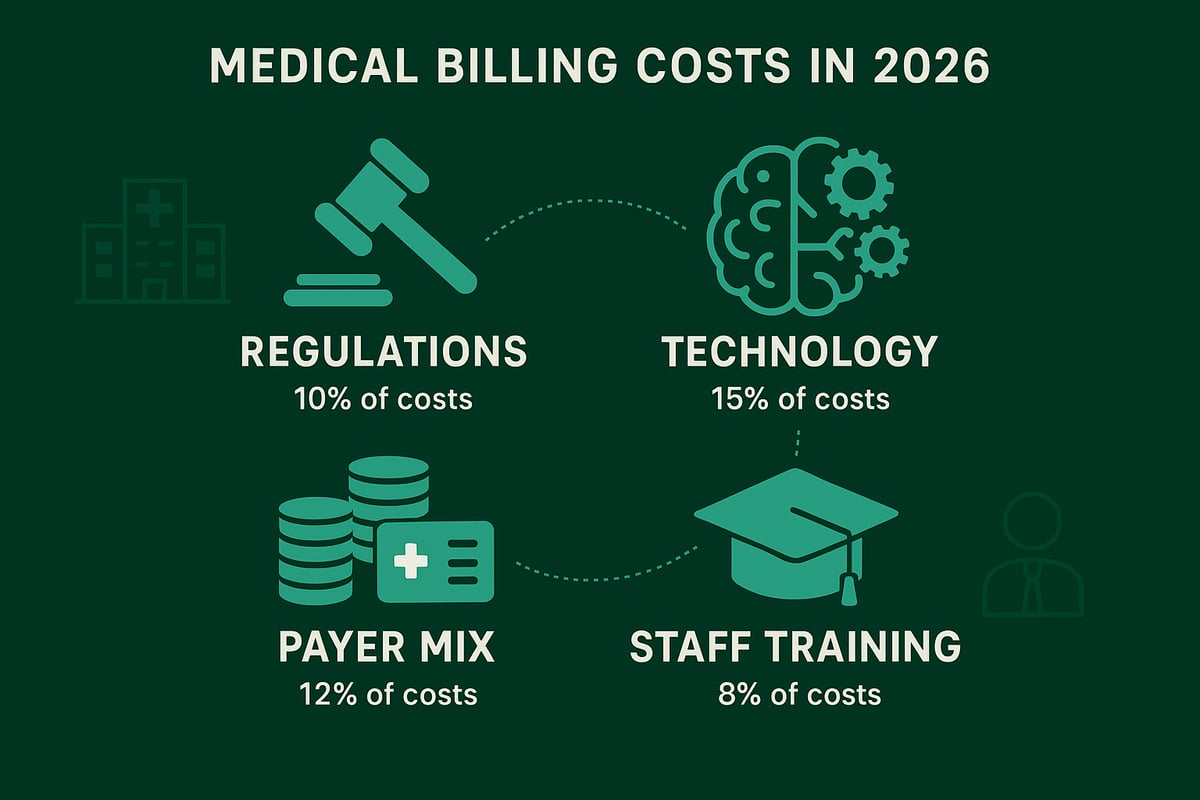
Regulatory and Compliance Changes
In 2026, regulatory shifts are a primary driver of medical billing costs. Healthcare providers must navigate updates related to HIPAA, the No Surprises Act, and evolving state mandates. These changes increase the burden of documentation and require frequent staff training, legal consultation, and periodic audits.
Compliance expenses include not only direct costs for education and policy updates but also the risk of incurring fines for non-compliance. For example, failure to meet documentation requirements or transparency mandates can lead to substantial penalties. According to Medical cost trend: Behind the numbers: PwC, regulatory changes are a significant contributor to rising medical billing costs, compelling organizations to invest in proactive compliance strategies.
Technology Adoption and Automation
The adoption of advanced technology is reshaping medical billing costs. Artificial intelligence, robotic process automation, and seamless EHR integration are streamlining repetitive billing tasks, reducing manual errors, and decreasing claim denial rates. Practices leveraging automation often report up to 20 percent fewer denials, which translates into direct cost savings.
However, transitioning to automated systems involves upfront investments in integration and ongoing technology support. Balancing these initial expenses against long-term efficiency gains is crucial. As organizations evaluate new solutions, they must ensure compatibility with existing workflows and maintain industry-standard security protocols. Technology, when thoughtfully implemented, is a catalyst for managing medical billing costs effectively.
Payer Mix and Reimbursement Rates
The payer mix—comprising Medicare, Medicaid, and private insurance—directly affects medical billing costs for healthcare providers. Each payer type comes with unique reimbursement rates, administrative requirements, and complexity levels. Practices with a higher proportion of government payers may face lower reimbursement but encounter less administrative friction, while those dealing with multiple commercial payers often experience increased variability and overhead.
Value-based care and bundled payment models are also influencing the cost landscape. Specialty practices, in particular, report higher administrative costs due to complex payer negotiations and compliance with bundled payment requirements. Monitoring payer mix trends is essential for forecasting and controlling medical billing costs.
Staff Expertise and Training
Investing in staff expertise remains a cornerstone of controlling medical billing costs. Certified billing and coding professionals are better equipped to manage claim submissions, minimize errors, and keep up with regulatory updates such as ICD-11 and CPT code changes.
Ongoing training ensures staff remain current with industry standards, which leads to higher claim acceptance rates and fewer denials. Practices that implement regular education programs and performance reviews consistently report improved financial outcomes. The correlation between skilled staff and optimized medical billing costs underscores the importance of continuous professional development.
Navigating Billing Transparency and Patient Cost Estimates
As medical billing costs continue to climb in 2026, healthcare organizations face mounting pressure from both regulators and patients for greater price transparency. New mandates require providers to offer more accurate, upfront patient cost estimates, making transparency not just a compliance issue but a strategic necessity. According to recent projections, double-digit healthcare cost increases are expected to persist, further intensifying the need for clear communication with patients about their financial responsibilities. Providers are responding by investing in online estimator tools, patient portals, and real-time data integration to meet these expectations.
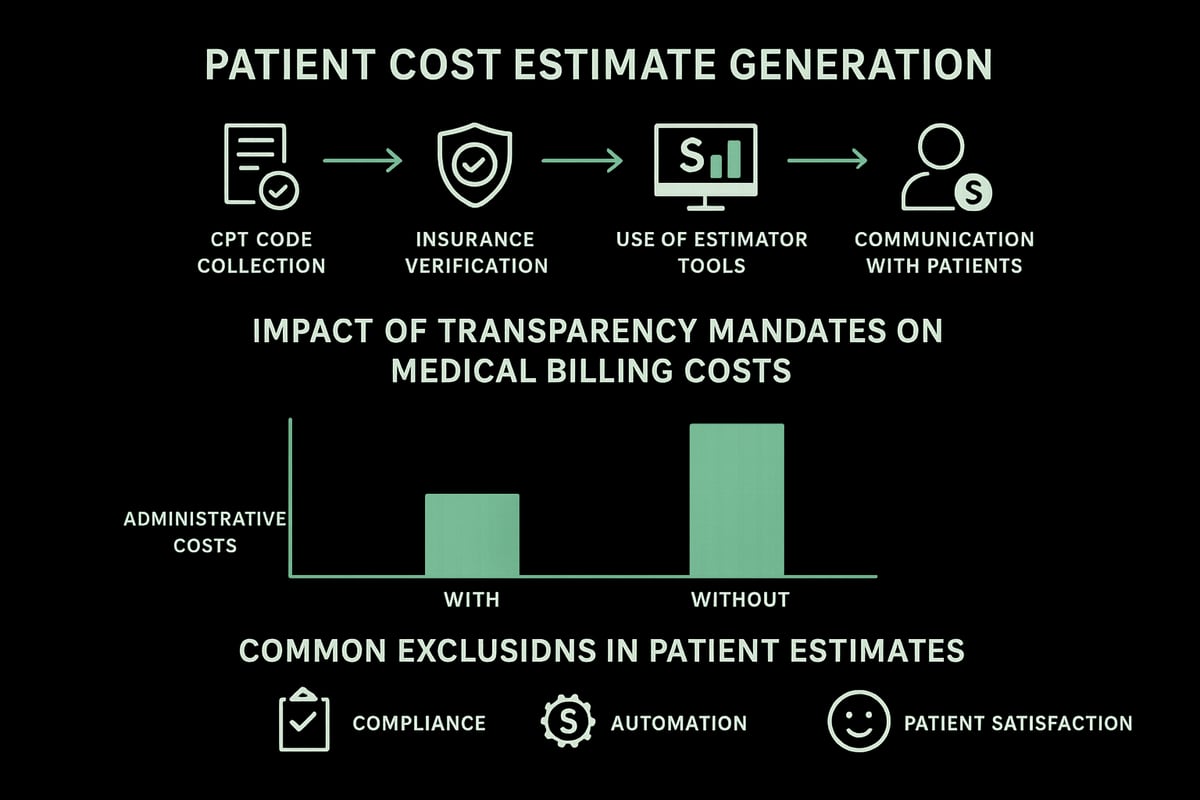
The Push for Price Transparency in 2026
Price transparency has become a cornerstone of patient trust and regulatory compliance in the healthcare sector. New laws require practices to provide upfront estimates of medical billing costs before services are rendered. Tools like patient portals and real-time cost estimators, such as UCHealth’s My Health Connection, are increasingly common. However, estimating costs for complex or bundled procedures remains a challenge for many providers.
Patient demand for transparency has surged by 25% since 2024, driven by the rising burden of out-of-pocket expenses and the overall increase in medical billing costs. Industry reports indicate that double-digit healthcare cost increases are projected to persist into 2026 and beyond, making accurate estimates essential for patient satisfaction and financial planning.
Steps to Providing Accurate Patient Estimates
Delivering precise patient estimates requires a structured approach. Providers must gather correct CPT codes for each procedure, verify insurance benefits, and input data into estimator tools. This process helps ensure that the medical billing costs communicated to patients are as accurate as possible.
Best practices include:
- Verifying patient eligibility and benefits before appointments
- Using up-to-date estimator tools integrated with billing systems
- Providing both written and online estimates for transparency
Clear communication is crucial. Practices should explain what is included in the estimate and address any exclusions, helping manage patient expectations. Written estimates often result in higher patient satisfaction compared to solely online estimates, as they provide an official record and reduce misunderstandings.
Exclusions and Limitations in Cost Estimates
Despite best efforts, some services are commonly excluded from standard cost estimates. Anesthesia, third-party laboratory work, and emergency interventions often fall outside initial projections, impacting the final medical billing costs for patients. Legal requirements now mandate that providers clearly disclose all exclusions upfront.
Failing to communicate these exclusions can lead to patient dissatisfaction and billing disputes. To mitigate these risks, organizations should:
- List all potential exclusions in both written and digital estimates
- Educate staff on legal disclosure requirements
- Regularly update estimate templates to reflect changes in regulations
Clarifying these limitations at the outset builds trust and reduces the likelihood of payment delays or disputes.
Impact of Transparency on Administrative Costs
The push for transparency has increased the administrative workload for many practices. Generating, updating, and delivering patient estimates requires coordination between billing, clinical, and administrative teams. Balancing operational efficiency with transparency is a challenge, especially as medical billing costs rise.
However, automation is helping to streamline this process. Practices leveraging automated estimation tools report up to 15% lower administrative costs, freeing staff to focus on higher-value activities. By investing in automation, healthcare organizations can meet transparency mandates while controlling operational expenses and maintaining compliance.
Strategies for Managing and Reducing Medical Billing Costs
Effectively managing medical billing costs is essential for healthcare organizations seeking to maintain profitability and compliance in 2026. With rising administrative demands and regulatory pressures, a multi-faceted approach is necessary to keep costs in check while optimizing revenue cycle performance.
Process Optimization and Workflow Automation
Streamlining workflows is a proven way to reduce medical billing costs. Begin by mapping the entire billing process, from patient registration through final payment, to identify inefficiencies and redundant steps.
Automating repetitive tasks, such as claim submission, eligibility verification, and denial follow-up, frees staff to focus on complex cases. Robotic process automation (RPA) can help practices cut claim cycle times by up to 30 percent. Practices that adopt automation not only see lower labor expenses but also experience fewer errors and faster reimbursements.
According to Staying ahead of healthcare costs: Strategies for 2026 – WTW, targeted process improvements and digital tools are critical for controlling medical billing costs in a rapidly evolving landscape.
Staff Training and Performance Management
Continuous staff training is crucial for controlling medical billing costs. Certified billing professionals are better equipped to navigate complex coding updates and payer requirements, reducing costly errors and claim denials.
Implementing regular training sessions ensures staff remain current with industry standards such as ICD-11 and CPT code changes. Setting clear KPIs for accuracy and productivity, then conducting periodic performance reviews, helps maintain high standards across the team.
Practices that invest in ongoing education and credentialing report fewer denied claims and faster payment cycles. This not only improves cash flow but also minimizes rework and administrative overhead, directly impacting medical billing costs.
Leveraging Third-Party Billing Services
Outsourcing to specialized billing services offers significant advantages for managing medical billing costs. Third-party partners provide access to scalable resources, compliance expertise, and advanced analytics, reducing the need for in-house infrastructure and training.
A cost-benefit analysis often reveals that outsourcing can lead to lower operational expenses and higher net collections, especially as claim complexity and regulatory requirements increase. Practices that switch to expert billing partners see, on average, a 20 percent increase in net collections and fewer denied claims.
Selecting the right partner involves evaluating service scope, transparency, and support for your specialty. Outsourcing is particularly effective for organizations seeking to control medical billing costs without sacrificing quality or compliance.
How Greenhive Billing Solutions Can Optimize Your Revenue Cycle
Greenhive delivers comprehensive revenue cycle management tailored to healthcare providers’ unique needs. Our services, including insurance eligibility verification, claims processing, and denial management, are designed to minimize medical billing costs while maximizing collections.
We emphasize HIPAA compliance and transparent communication, providing detailed, data-driven reports for every client. A recent case study showed a medium-sized practice reduced overall medical billing costs by adopting Greenhive’s performance-based pricing model.
Our experienced team integrates seamlessly with existing EHR and PMS systems, adapting workflows to specialty-specific requirements. This ensures a smooth transition, ongoing support, and measurable financial improvement for our clients.
Monitoring and Benchmarking Billing Performance
Ongoing monitoring is vital for sustaining reductions in medical billing costs. Establish key metrics such as days in accounts receivable (A/R), denial rates, and net collection percentage to track progress.
Dashboards and analytics platforms provide real-time insights, enabling quick identification of bottlenecks and areas needing improvement. Regular benchmarking against industry standards helps practices set realistic goals and measure success.
Practices leveraging real-time analytics resolve billing issues up to 40 percent faster, resulting in better cash flow and fewer costly delays. Consistent performance tracking is the foundation for continuous improvement in medical billing costs.
Preparing for the Future: Trends and Predictions for Medical Billing Costs
As the healthcare landscape evolves, so do the drivers of medical billing costs. For healthcare organizations, anticipating these shifts is crucial for strategic planning and financial health. Below, we explore four key trends set to shape the future of medical billing costs through 2026 and beyond.
Impact of Evolving Payment Models
Healthcare payment models are rapidly transitioning from traditional fee-for-service to value-based care, bundled payments, and capitation. This evolution brings both opportunities and challenges for managing medical billing costs. Value-based models reward outcomes over volume, but often introduce greater billing complexity. Practices must adapt workflows to accommodate new requirements for data collection, reporting, and compliance.
For example, bundled payments require precise tracking across episodes of care, impacting administrative overhead. Organizations that invest in flexible billing workflows can better control medical billing costs and respond to payment model shifts. As payment structures become more complex, proactive billing strategies are essential for sustainability.
Advances in Billing Technology
Technology will be a major catalyst for reducing medical billing costs in the coming years. Predictive analytics, AI-driven coding solutions, and blockchain for secure transactions are gaining traction across the industry. These innovations promise to lower manual workloads, improve claim accuracy, and decrease denial rates.
Practices leveraging advanced reporting and analytics for billing are better equipped to identify cost drivers and optimize billing performance. However, adopting new technologies requires upfront investment and ongoing staff adaptation. The organizations that successfully integrate these tools can expect measurable improvements in efficiency and cost control for medical billing costs.
Regulatory Outlook and Anticipated Changes
Federal and state regulations will continue to shape the landscape of medical billing costs. In 2026, practices should expect stricter transparency requirements and enhanced patient protection laws. For instance, the Centers for Medicare & Medicaid Services have proposed significant updates to reduce spending waste and improve payment accuracy, as detailed in their CMS Proposes Physician Payment Rule.
Anticipated changes to the No Surprises Act and other regulations will demand more robust compliance processes. Failing to stay ahead of these changes can result in costly penalties. Regular policy reviews and proactive staff training are vital to managing regulatory-driven medical billing costs.
Workforce and Talent Trends in Billing
The demand for certified billing professionals is on the rise, directly affecting medical billing costs for healthcare organizations. As billing processes become more complex, practices are increasingly turning to specialized firms and outsourcing solutions to fill the talent gap.
Remote work trends are also influencing recruitment and retention strategies. The rise of specialized billing service providers allows organizations to access expert talent while controlling overhead costs. Investing in ongoing staff education and leveraging external expertise will be critical for maintaining cost-effective and compliant billing operations.
Best Practices for Healthcare Providers to Control Billing Costs in 2026
Effectively controlling medical billing costs in 2026 requires a proactive, strategic approach. Healthcare organizations must implement best practices across auditing, communication, continuous improvement, and collaboration to safeguard financial performance.
Conducting Regular Cost Audits
Routine cost audits are essential for identifying hidden inefficiencies within your medical billing costs. Start by mapping each step of the billing workflow and documenting all associated expenses.
Use audit tools and checklists to ensure thorough reviews, such as:
- Labor and training costs
- Software and platform usage fees
- Claim denial and resubmission rates
- Compliance and regulatory expenses
Annual reviews often uncover overlooked charges or outdated processes, enabling timely corrections. By auditing regularly, healthcare providers gain a clear picture of their medical billing costs and can prioritize targeted improvements.
Enhancing Communication with Patients and Payers
Clear, proactive communication helps minimize errors and streamline claim resolution, directly impacting medical billing costs. Educate patients about their financial responsibilities and offer transparent estimates upfront.
Strengthen payer relationships by clarifying requirements and promptly addressing claim issues. Practices that focus on communication and denial management in medical billing report fewer denied claims and faster reimbursements.
Consider regular meetings with billing staff to review payer feedback and update scripts or templates. Improved communication reduces costly misunderstandings and supports a healthier revenue cycle.
Investing in Continuous Improvement
Establishing a culture of ongoing improvement is crucial for managing medical billing costs over time. Encourage staff to stay informed about regulatory updates and industry trends.
Implement quarterly process reviews to identify bottlenecks and outdated practices. Set measurable goals for billing accuracy, claim turnaround, and staff training participation.
By fostering innovation and adaptability, healthcare organizations can quickly respond to changes that influence medical billing costs. This commitment to improvement keeps operational expenses in check and boosts long-term efficiency.
Collaborating with Industry Partners and Associations
Collaboration with external partners and professional associations can provide valuable insights for optimizing medical billing costs. Leverage benchmarking data, shared resources, and best practice forums to stay competitive.
Participate in industry initiatives or join organizations tailored to your practice size. For example, small practices benefit from specialized support such as medical billing services for small practices, which helps control costs and improve compliance.
Regular engagement with peers and experts ensures your team remains aligned with evolving standards and cost-saving strategies.
Now that you’ve explored the key factors shaping medical billing costs in 2026—from evolving regulations to the impact of automation and the value of transparent communication—you might be wondering how to put these strategies into action for your own practice. At Greenhive Billing Solutions, we understand how important it is to optimize your revenue cycle while staying compliant and future ready. If you’re ready to discover tailored solutions that can simplify your billing process and improve your bottom line, let’s start a conversation about your unique needs. Book Your Free Consultation