Accurate payment posting is more critical than ever in healthcare revenue cycle management as we approach 2026. Many practices struggle with understanding the right cpt code for posting payment, which can lead to claim delays and lost revenue.
Confusion around CPT codes often results in denied claims and compliance risks, making it essential for organizations to master this process. By ensuring correct CPT code selection, your team can optimize reimbursement, minimize errors, and stay ahead of industry changes.
This expert guide will walk you through CPT code fundamentals, highlight the 2026 updates, provide a step-by-step payment posting process, and share compliance tips and best practices for maximizing your revenue cycle performance.
Understanding CPT Codes and Payment Posting
Accurate payment posting is the backbone of healthcare revenue cycle management. To optimize reimbursement and minimize errors, professionals must fully understand the cpt code for posting payment and its impact across workflows. This section unpacks the essentials, from code fundamentals to real-world challenges.
What Are CPT Codes?
CPT codes, or Current Procedural Terminology codes, are standardized numeric codes assigned to medical, surgical, and diagnostic services. These codes enable healthcare providers to communicate uniform information about procedures to payers for billing and reimbursement.
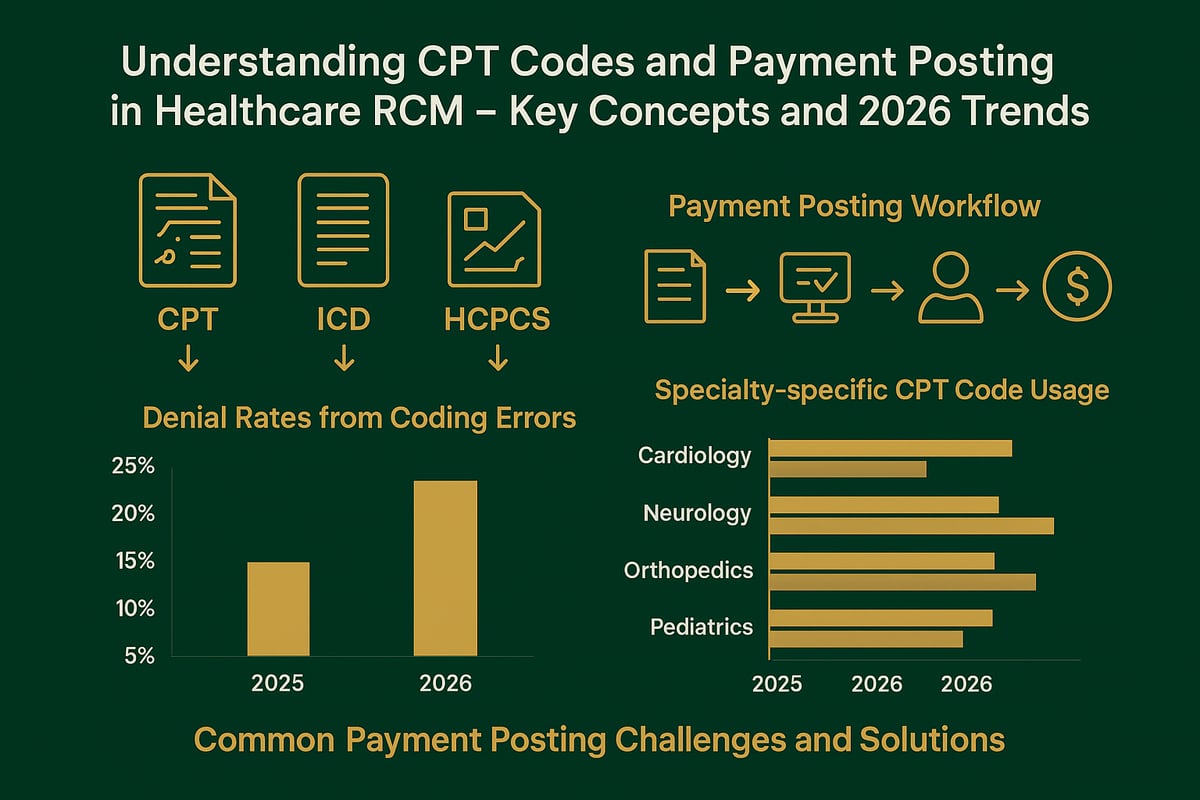
CPT codes differ from ICD codes, which classify diagnoses, and HCPCS codes, which cover supplies and non-physician services. For example, CPT 99213 represents a standard office visit, while ICD-10 E11.9 codes for diabetes.
Accurate code assignment is crucial. Incorrect use of a cpt code for posting payment can result in claim denials or compliance issues. For a foundational overview, see What is a CPT code for insurance.
The Payment Posting Process in Healthcare RCM
Payment posting refers to recording payments and adjustments in the practice management or EHR system. This includes insurance payments, patient payments, and contractual adjustments. Proper payment posting directly affects accounts receivable and cash flow.
The process starts with reviewing remittance advice, matching payments with billed services via the cpt code for posting payment, and entering data accurately. A streamlined workflow minimizes posting errors and ensures financial clarity for healthcare organizations.
The connection between CPT codes and payment posting is vital, as each posted payment must correspond to the correct code for regulatory compliance and reporting.
Why Correct CPT Code Selection Matters for Payment Posting
Selecting the right cpt code for posting payment has a significant impact on claim acceptance and denial rates. Incorrect coding can slow reimbursement, increase denial rates, and trigger compliance audits.
For instance, a mismatched CPT code can lead to immediate claim rejection. According to industry data, coding errors account for nearly 30% of denied claims. This highlights the importance of vigilance in code selection during payment posting.
Mistakes not only delay payments but also expose organizations to audit risks and potential penalties. Precision in this step is non-negotiable.
Common CPT Codes Used in Payment Posting
Certain CPT codes appear frequently in payment posting across specialties. Evaluation and Management (E/M) codes, such as 99213 and 99214, are common for primary care. Procedure codes (e.g., 93000 for EKG) and ancillary codes (e.g., 36415 for venipuncture) are also widely used.
Specialties have unique nuances. For example, orthopedics may use more surgical codes, while radiology relies on imaging procedure codes. In 2025-2026, E/M and preventive care codes continue to be the most utilized for cpt code for posting payment activities.
Recognizing these patterns helps billing teams prioritize accuracy and anticipate payer scrutiny.
Challenges in CPT Coding and Payment Posting
Common challenges in cpt code for posting payment include misreading payer rules, manual entry errors, and misunderstanding code changes. Payer-specific requirements add complexity, and trends show increased audits and recoupments tied to coding mistakes.
Typical pitfalls:
- Posting payments to incorrect codes
- Overlooking bundled service rules
- Missing documentation for high-value codes
To address these, organizations can implement regular training, internal audits, and standardized workflows. Proactive measures reduce revenue loss and support compliance in an evolving regulatory landscape.
The 2026 CPT Code Updates for Payment Posting
The landscape of CPT codes is evolving rapidly, and 2026 brings significant updates that every healthcare organization must address. Understanding the cpt code for posting payment is essential to ensure compliance, optimize reimbursement, and avoid costly claim denials. Below, we break down the key changes, their impact on the revenue cycle, how to prepare your billing team, and the best resources for staying ahead.
Key Changes in CPT Codes Relevant to Payment Posting
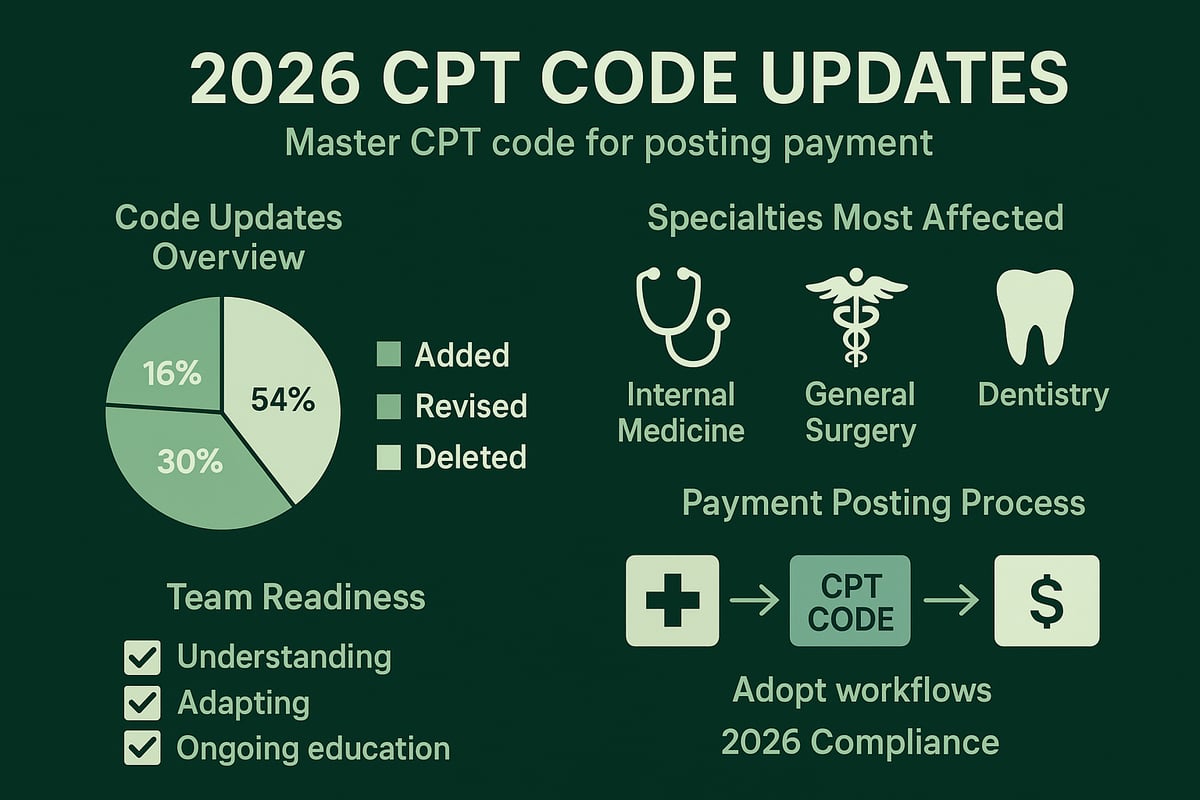
The 2026 update introduces a substantial number of modifications to the cpt code for posting payment. According to the AMA releases CPT 2026 code set, more than 250 codes have been revised, with notable additions and deletions spanning high-volume specialties such as cardiology, orthopedics, and telehealth.
For example, new codes have been introduced for emerging procedures in digital health and remote patient monitoring, while some legacy codes have been consolidated or deleted. This means that practices must carefully review the codes most relevant to their specialty to ensure the proper cpt code for posting payment is selected for each service.
A summary table of the changes:
| Change Type | Number of Codes | Impacted Specialties |
|---|---|---|
| New Codes | 90 | Telehealth, Cardiology |
| Revised Codes | 120 | Primary Care, Orthopedics |
| Deleted Codes | 40 | General Surgery, Radiology |
Staying current with these changes is crucial, as approximately 18% of all CPT codes used in payment posting will be affected in 2026.
Implications for Revenue Cycle Management
The 2026 CPT code changes directly influence every aspect of the cpt code for posting payment process. New and revised codes can alter how services are billed, how claims are submitted, and how quickly payments are processed. Practices must update their billing workflows, ensuring that EHR and practice management systems reflect the latest cpt code for posting payment.
Adjustments in payer contracts and reimbursement schedules may be required, especially where new codes offer higher or lower reimbursement rates. For instance, a multispecialty clinic that rapidly updated its charge master and retrained staff saw a 15% improvement in first-pass claim acceptance after adopting the 2026 codes.
Payers are also updating their adjudication logic, and early industry feedback indicates that proactive practices will experience fewer denials and faster payments when they implement the updated cpt code for posting payment promptly.
Preparing Your Team for 2026 CPT Code Changes
Preparation is the foundation for successful adaptation to the 2026 cpt code for posting payment updates. Start by scheduling regular training sessions to upskill billing and coding staff. Update all internal coding manuals, cheat sheets, and workflow diagrams to reflect the new and revised codes.
Effective communication between clinical and billing teams is essential. Share code changes in team meetings and encourage staff to ask questions. Consider implementing a readiness checklist that includes:
- Verification of updated cpt code for posting payment in billing systems
- Staff attendance at coding update workshops
- Review and revision of payer-specific coding guidelines
- Regular internal audits of posted payments
By proactively preparing your team, your organization can minimize disruption and maintain accurate, compliant payment posting.
Resources for Staying Current with CPT Code Changes
Access to reliable resources is a critical element in mastering the cpt code for posting payment as regulations evolve. The American Medical Association (AMA) is the primary source for official CPT code updates, offering annual codebooks, webinars, and online tools. Industry associations such as AAPC and AHIMA provide certification courses, coding bootcamps, and newsletters tailored to 2026 changes.
Participate in online training and workshops for hands-on application of new codes. Subscribe to reputable publications that summarize key updates and provide practical tips for payment posting. Finally, establish a routine for ongoing education and compliance checks to ensure your team remains confident and current with every cpt code for posting payment update.
Step-by-Step Guide: Posting Payments Using CPT Codes in 2026
Accurate payment posting is the backbone of effective revenue cycle management for healthcare organizations. Mastering each step of the process ensures that every cpt code for posting payment is correctly applied, leading to optimized cash flow, reduced errors, and full compliance.
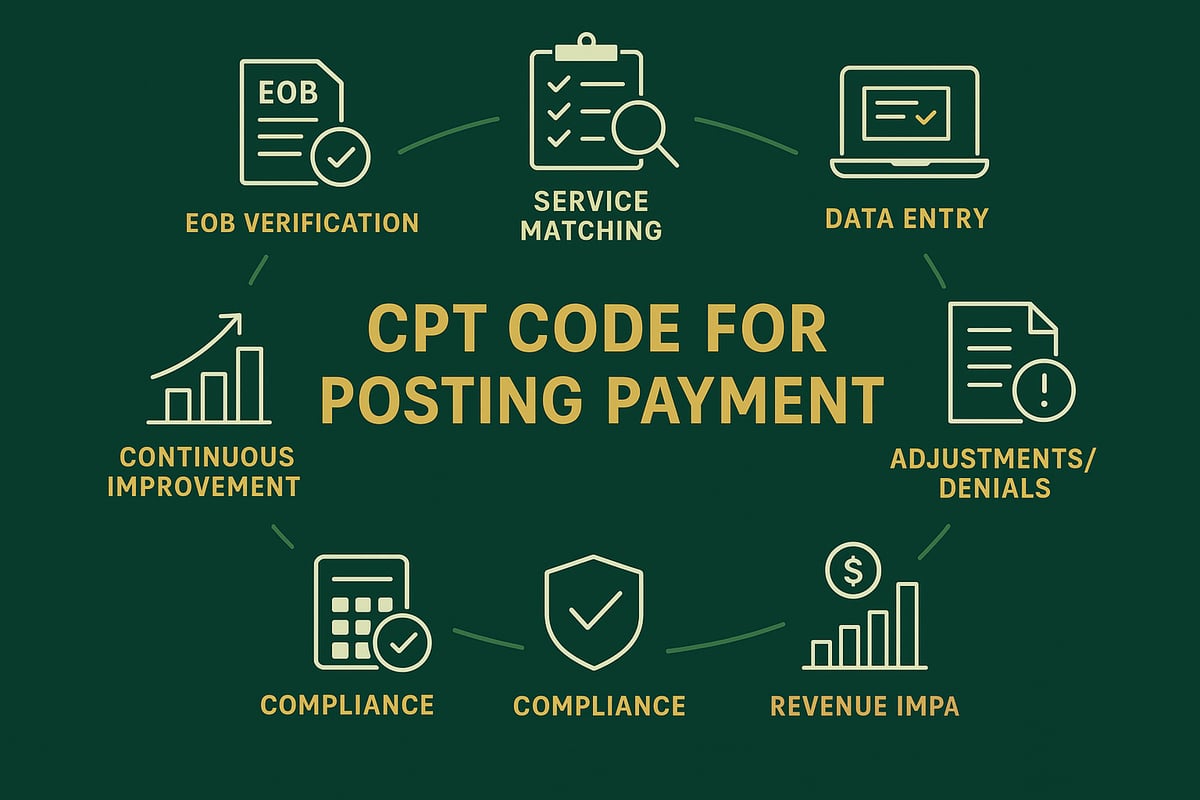
Step 1: Verifying the Explanation of Benefits (EOB)
Begin every payment posting session by thoroughly reviewing the Explanation of Benefits (EOB) provided by payers. The EOB outlines the services billed, the approved cpt code for posting payment, amounts paid, patient responsibility, and any denials or adjustments.
Check that all CPT codes listed on the EOB match those billed. Discrepancies often arise due to payer edits or bundling rules. If the cpt code for posting payment does not align with your records, flag it for investigation.
Common issues to watch for:
- Missing or altered CPT codes
- Incorrect allowed amounts
- Unexplained denials
Best practice: Use a standardized checklist to confirm that every cpt code for posting payment is correctly documented on the EOB before proceeding.
Step 2: Matching Payments to Services Rendered
After EOB verification, cross-reference payments with the original services provided. This step ensures each cpt code for posting payment accurately maps to the clinical services performed.
Address complexities such as:
- Bundled vs. unbundled services
- Multiple services under a single payment
- Partial payments or split payments across codes
For example, a cardiology visit may include both an E/M code and a procedure code. Ensure each cpt code for posting payment is matched to the corresponding line item.
Documentation tip: Maintain detailed service logs for every encounter to back up the code selection and payment application.
Step 3: Data Entry and System Posting
Enter payments into your EHR or practice management system, assigning the correct cpt code for posting payment to each transaction. Accurate data entry is essential to avoid downstream errors and audit issues.
Decide whether to use manual posting or automation:
- Manual: Greater control, but higher risk of human error
- Automated: Faster, but requires robust system mapping
Error prevention strategies include double-verification and built-in system alerts. For a full overview of the payment posting process, see our Payment posting services overview.
Case example: In a mid-sized clinic, batching payments by cpt code for posting payment reduced reconciliation time by 30%.
Step 4: Handling Adjustments, Write-Offs, and Denials
Adjustments and write-offs are common in payment posting. Each must be correctly linked to the appropriate cpt code for posting payment for accurate financial reporting and compliance.
Types of adjustments include:
- Contractual write-offs
- Patient responsibility adjustments
- Denials due to coding errors
When denials are received, analyze the root cause. Was the cpt code for posting payment entered incorrectly, or did the payer apply a new policy? Post denials and adjustments promptly, documenting the rationale and follow-up actions.
Best practice: Use a denial log categorized by cpt code for posting payment to identify trends and training needs.
Step 5: Reconciling Payments and Reporting
Reconciliation verifies that posted payments match actual bank deposits and payer remittances. Track each cpt code for posting payment to ensure no revenue is missed or misapplied.
Steps for reconciliation:
- Compare posted payments to bank statements
- Generate reports by cpt code for posting payment
- Investigate and resolve discrepancies
Use analytics to spot payment trends, such as frequent underpayments for specific codes. A reconciliation checklist can streamline this monthly process and highlight potential issues early.
Step 6: Ensuring Compliance and Audit Readiness
Every cpt code for posting payment must be fully documented to withstand internal and external audits. Adhere to HIPAA and payer-specific requirements for record-keeping and data security.
Set up robust audit trails in your payment posting workflow:
- Document the user, date, and rationale for each entry
- Regularly review posted transactions for compliance
Quality assurance checks, such as random audits of posted payments by cpt code for posting payment, help prevent costly errors and penalties.
Tip: Schedule quarterly compliance reviews to stay ahead of regulatory changes and payer audits.
Step 7: Continuous Improvement and Feedback Loops
Ongoing improvement is key to long-term success in payment posting. Gather feedback from billing and clinical teams on the cpt code for posting payment process.
Leverage analytics to identify patterns, such as recurring coding errors or delays. Implement process enhancements based on real-world data and staff input.
- Hold quarterly review sessions
- Update training materials as coding rules evolve
- Share best practices across teams
By refining your approach to cpt code for posting payment, you can maximize revenue, minimize denials, and ensure operational excellence.
Compliance, Risk Management, and Best Practices
Achieving accuracy and compliance with the cpt code for posting payment is not just about code selection. It requires a holistic approach combining regulatory awareness, denial management, internal controls, team training, and sometimes, the support of expert RCM service providers. Below, we outline the core best practices that every healthcare organization should follow to mitigate risk, ensure compliance, and drive revenue integrity in 2026.
![]()
Regulatory Requirements for CPT Coding and Payment Posting
Federal and state regulations set the foundation for the compliant use of the cpt code for posting payment. Healthcare organizations must adhere to Medicare and Medicaid rules, as well as payer-specific mandates. Documentation and record-keeping standards are strict, requiring detailed audit trails for every transaction.
Key regulatory requirements include:
- Accurate assignment and documentation of CPT codes for all posted payments
- Maintenance of thorough records for at least the minimum statutory period
- Adherence to payer-specific coding guidelines
- Timely reporting of adjustments and denials linked to CPT codes
Non-compliance can lead to financial penalties and increased audit risk. Regular reviews and updates to your compliance policies are essential to keeping pace with evolving requirements.
Minimizing Denials and Maximizing Reimbursements
Reducing denials tied to the cpt code for posting payment is essential for healthy cash flow. The most common denial reasons include incorrect code selection, insufficient documentation, and mismatches between billed and posted services. Clean claim submission starts with proper code validation and real-time eligibility checks.
Strategies to minimize denials:
- Implement front-end code validation and eligibility verification
- Train staff to recognize and avoid common coding pitfalls
- Establish a dedicated denial management workflow
- Monitor denial trends and adjust processes accordingly
For a deeper dive into denial management strategies and their impact on cash flow, see How denial management improves cash flow. Proactive denial management enables organizations to recover lost revenue and optimize their reimbursement rates.
Internal Controls and Quality Assurance
Robust internal controls are the backbone of accurate cpt code for posting payment. Double-checking codes, conducting regular audits, and leveraging technology for quality assurance help prevent costly errors.
Best practices for internal controls:
- Use a QA checklist for payment posting reviews
- Schedule monthly internal audits focused on CPT code assignment
- Implement technology solutions for error detection and workflow automation
- Track staff performance metrics for accountability
| QA Checklist Item | Frequency | Responsible Party |
|---|---|---|
| Double-check CPT code entries | Daily | Billing Staff |
| Audit random payment postings | Weekly | QA Lead |
| Review adjustment and denial trends | Monthly | RCM Manager |
| Update coding guidelines | Quarterly | Compliance Team |
Quality assurance protects against revenue leakage and strengthens audit readiness.
Training and Certification for Billing Staff
The cpt code for posting payment process is only as reliable as the team managing it. Certified and well-trained billing staff are critical for ongoing compliance and operational excellence. Industry-recognized certifications like CPC and CCS-P demonstrate expertise and commitment.
Ongoing staff development should include:
- Annual certification renewals and continuing education
- Monthly coding workshops and update sessions
- Access to industry webinars and newsletters
- Peer review and knowledge sharing forums
Sample Training Schedule:
Monday | Weekly Coding Update (30 min)
Wednesday | Case Study Review (15 min)
Friday | Open Q&A Session (20 min)
Quarterly | External Webinar/Training
Investing in education ensures your team stays current with cpt code for posting payment standards and regulatory changes.
Leveraging Professional RCM Services for CPT Coding and Payment Posting
Outsourcing the cpt code for posting payment function to an experienced RCM partner can deliver measurable benefits. Professional service providers ensure compliance, reduce error rates, and drive process efficiency, all while adapting to your systems and workflows.
Benefits of professional RCM services:
- Access to specialized coding expertise
- Scalable staffing for volume fluctuations
- Enhanced audit readiness and documentation support
- Cost savings compared to in-house teams
Consider a partnership with a trusted RCM provider to strengthen your payment posting processes and support your team with industry-leading best practices.
Technology and Tools for Accurate Payment Posting
Staying ahead in healthcare revenue cycle management requires the right technology and tools, especially when dealing with the cpt code for posting payment. For 2026, integrating robust systems and leveraging advanced solutions ensures accuracy, efficiency, and compliance throughout the payment posting workflow.
EHR and Practice Management System Integration
Seamless integration between EHR and practice management systems forms the backbone of precise payment posting. When working with the cpt code for posting payment, it is critical that your systems support accurate code mapping, real-time updates, and interoperability with billing platforms.
Key features to consider include:
- Customizable CPT code mapping modules
- Automated charge capture for posted payments
- Real-time eligibility checks
Workflows must be tailored to specialty-specific requirements. For example, integrating code libraries for CPT, ICD, and HCPCS ensures correct assignment and reduces errors. For a deeper understanding of medical coding distinctions, Different types of medical coding offers a comprehensive overview. Common challenges include data migration, system compatibility, and user training, all of which can impact posting accuracy.
Automation and AI in Payment Posting
Automation and AI are transforming how organizations approach the cpt code for posting payment. Automated solutions streamline repetitive tasks like payment matching, code validation, and denial management, reducing manual errors and boosting throughput.
AI-driven platforms can:
- Analyze EOBs to suggest the most appropriate CPT codes
- Flag discrepancies in real time
- Learn from historical posting patterns to enhance accuracy
Many billing teams report up to a 30% reduction in posting errors after implementing automation. To stay ahead of evolving requirements, training on the latest CPT changes is essential. For in-depth instruction and hands-on application, the Deep Dive Into the 2026 CPT® Coding Updates workshop is highly recommended. By leveraging automation, your team can focus on higher-value tasks while maintaining strict compliance.
Reporting and Analytics for Payment Posting
Effective reporting and analytics are vital for monitoring the success of your cpt code for posting payment strategy. Custom dashboards allow you to track key metrics such as payment posting turnaround times, denial rates by CPT code, and payer-specific trends.
Best practices include:
- Generating monthly and quarterly reports filtered by CPT code
- Using analytics to identify revenue leakage or posting bottlenecks
- Setting up alerts for outlier claims or payment variances
Data-driven insights help organizations refine workflows and make informed decisions. Regular review of posting analytics ensures that issues are addressed proactively, supporting continuous revenue optimization and compliance.
Security, Privacy, and Compliance Tools
Safeguarding sensitive payment data is non-negotiable when dealing with the cpt code for posting payment. Implementing HIPAA-compliant processes, strong encryption, and strict access controls is essential for protecting patient information and financial records.
Consider the following security measures:
- Encrypted data transmission and storage
- Automated audit trails for all payment posting actions
- Role-based access to sensitive coding and billing data
Regular internal audits verify compliance and preparedness for external reviews. Use a security checklist to ensure your billing team follows best practices for documentation and data handling. Proactive monitoring tools help detect anomalies early and reduce the risk of costly compliance breaches.
Navigating the complexities of CPT code updates and payment posting can feel overwhelming, especially with the 2026 changes on the horizon. You deserve clarity and confidence as you work to streamline your revenue cycle, minimize denials, and ensure compliance. If you’re looking for tailored guidance or want to explore the best strategies for your practice, we’re here to help. Let’s take the next step together toward maximizing your reimbursements and operational efficiency.
Book Your Free Consultation
Whether you have specific questions or need a comprehensive review, our experts are ready to support you.