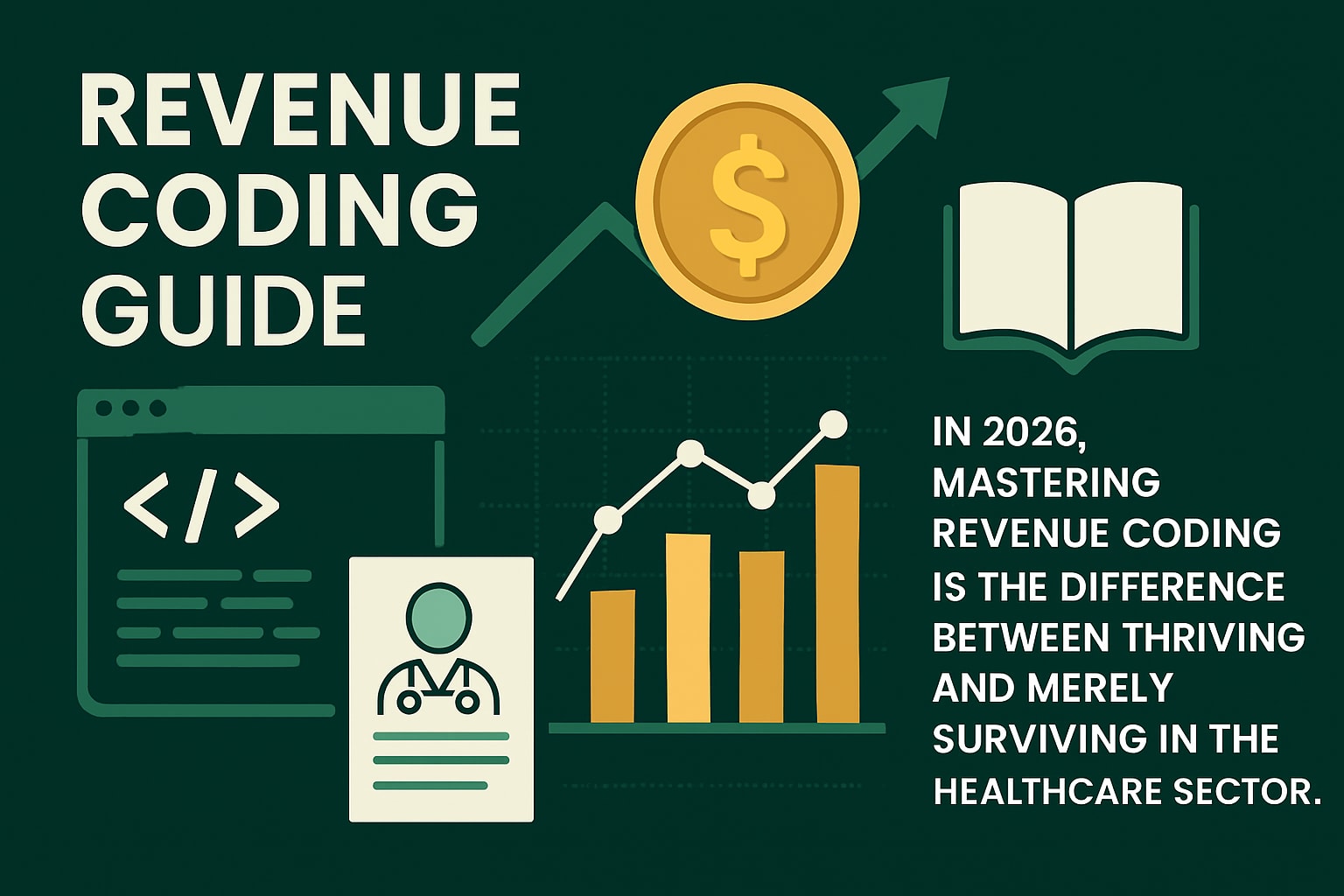
The landscape of physician rcm is rapidly evolving, bringing new complexities to healthcare practices as 2026 approaches. Physicians and healthcare organizations now face mounting financial pressures, from shrinking reimbursements to changing regulations that demand constant adaptation.
Operational challenges are growing, requiring providers to rethink traditional revenue management strategies. Mastering physician rcm has become essential for maintaining profitability and delivering quality patient care.
This guide offers a practical roadmap to success. We will explore RCM fundamentals, highlight emerging trends, walk through step-by-step optimization, discuss compliance and technology, and share expert strategies to help you maximize revenue in the years ahead.
Understanding Physician Revenue Cycle Management: The 2026 Perspective
Physician RCM is evolving rapidly, and understanding its core processes is critical for future-ready practices. As the healthcare environment grows more dynamic, mastering each phase of the revenue cycle will directly impact financial stability and operational efficiency. Let’s break down what you need to know heading into 2026.
![]()
Defining RCM and Its Core Components
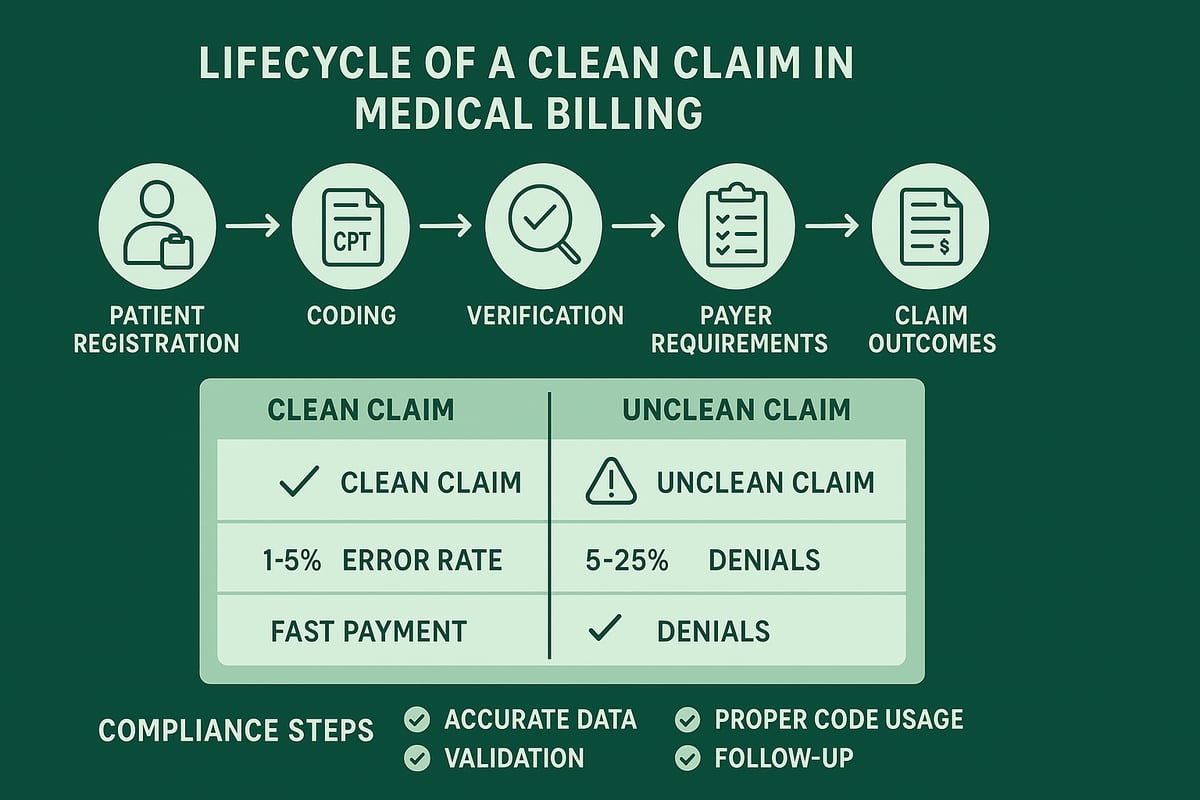
Physician RCM refers to the end-to-end process of managing a practice’s financial transactions, from the initial patient encounter to the final payment collection. The revenue cycle includes patient registration, insurance verification, charge capture, medical coding, claims submission, payment posting, denial management, and patient collections. Each component is essential for accurate reimbursement and compliance.
For example, if insurance verification is missed or incomplete, claims may be denied, causing delays and revenue loss. On average, claim denial rates for physician practices range from 5% to 10% (MGMA, 2023). Proper coding is especially vital—learn more about its role in medical coding in revenue cycle management. Every stage of physician rcm must be carefully managed for optimal results.
Key RCM Challenges Facing Physicians
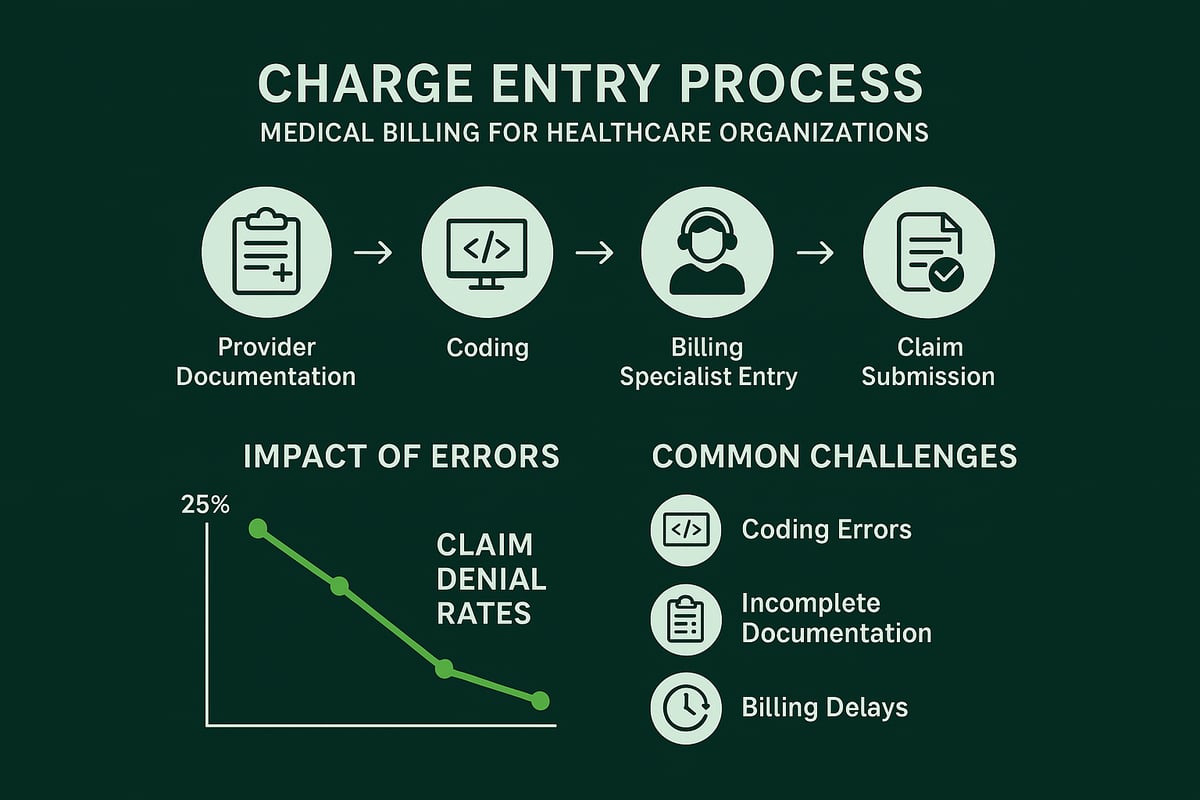
Physician RCM faces mounting challenges as payers introduce new reimbursement models and increase scrutiny. Administrative burdens are growing due to more complex billing requirements and ongoing staff shortages. Common pain points include delayed payments, high claim denial rates, and revenue leakage, all of which threaten practice profitability.
Coding errors, for instance, can significantly delay reimbursement as claims are rejected or require resubmission. Practices must dedicate resources to denial management and process improvement. Addressing these obstacles is paramount for effective physician rcm, especially as the industry shifts toward value-based payments and increased compliance demands.
The Financial Impact of Effective RCM
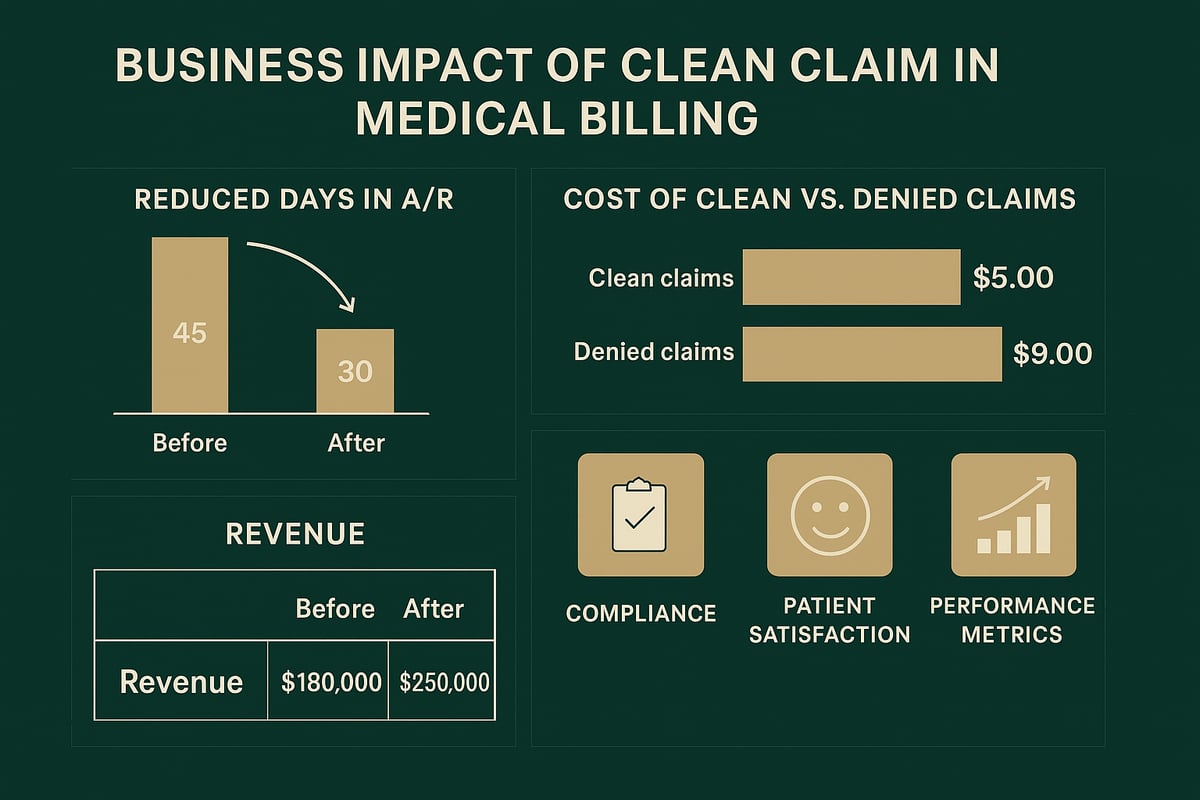
An optimized physician RCM process drives higher cash flow and profitability. Practices that invest in robust RCM systems and skilled staff see a measurable difference. According to the AMA (2023), practices with strong revenue cycle management achieve 15% to 20% higher net collections compared to those with weaker processes.
| Clinic Type | Net Collections Increase | Denial Rate |
|---|---|---|
| In-house RCM | Moderate | Higher |
| Outsourced RCM | Higher | Lower |
For example, a clinic leveraging outsourced RCM services may experience faster reimbursements and fewer denials than one relying solely on in-house resources. Effective physician rcm ensures that every dollar earned is collected efficiently.
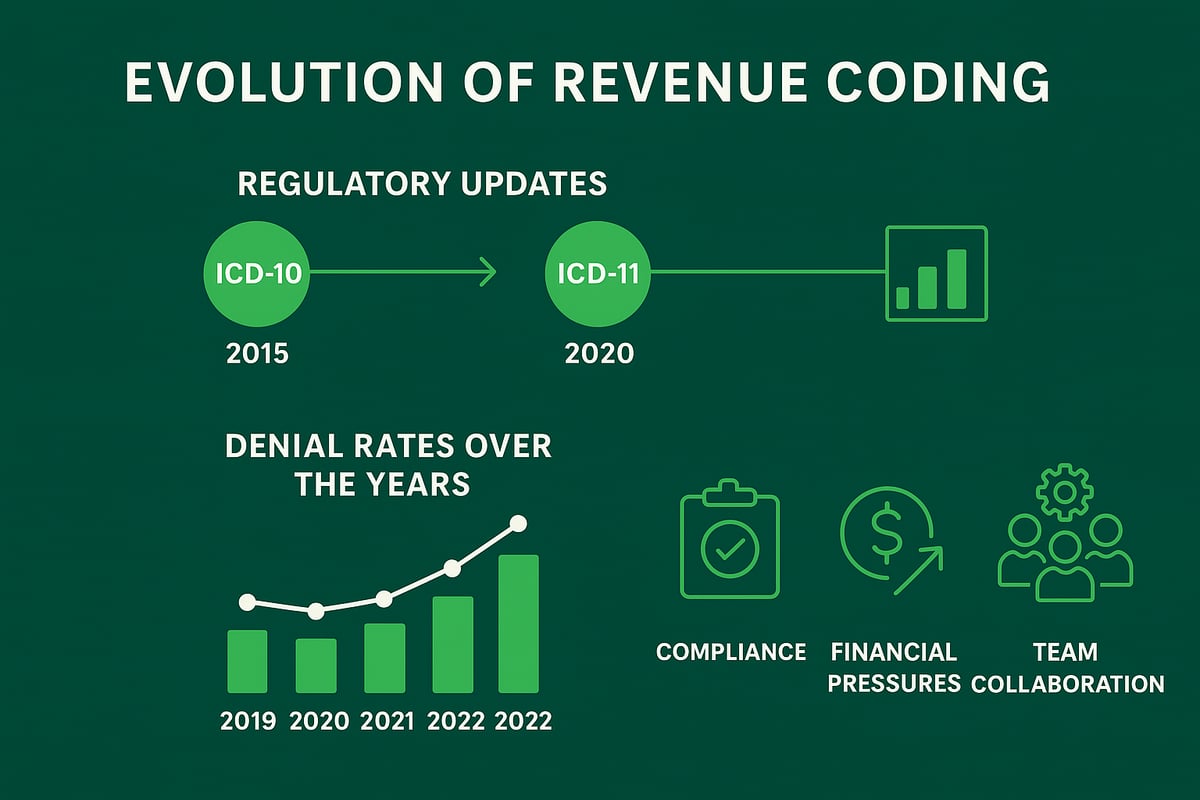
Evolving Regulatory and Payer Landscape
The regulatory environment for physician RCM will see significant changes by 2026. New mandates on price transparency and interoperability require practices to adapt their workflows and documentation. Compliance with evolving rules such as MIPS and MACRA is essential to avoid penalties and maintain eligibility for incentive payments.
Value-based care models are also shifting how services are billed and reimbursed. Physicians must adjust their RCM processes to accommodate bundled payments and quality reporting. Staying informed and proactive with physician rcm strategy will help practices remain competitive and compliant as regulations continue to evolve.
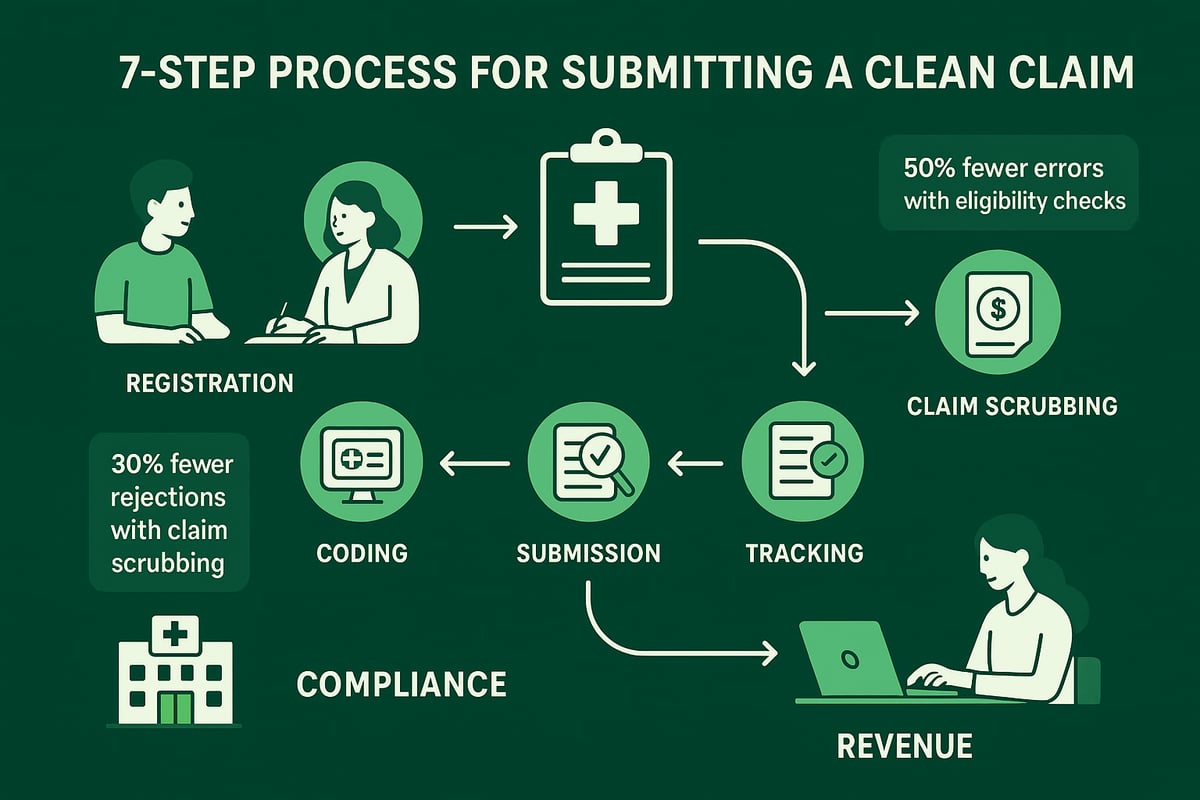
Step-by-Step Roadmap to RCM Success for Physicians
Achieving optimal results with physician rcm requires a systematic approach. By breaking the revenue cycle into clear, actionable steps, healthcare organizations can address each stage with precision and purpose. Let’s walk through the essential steps that drive efficiency, compliance, and profitability for physician practices.
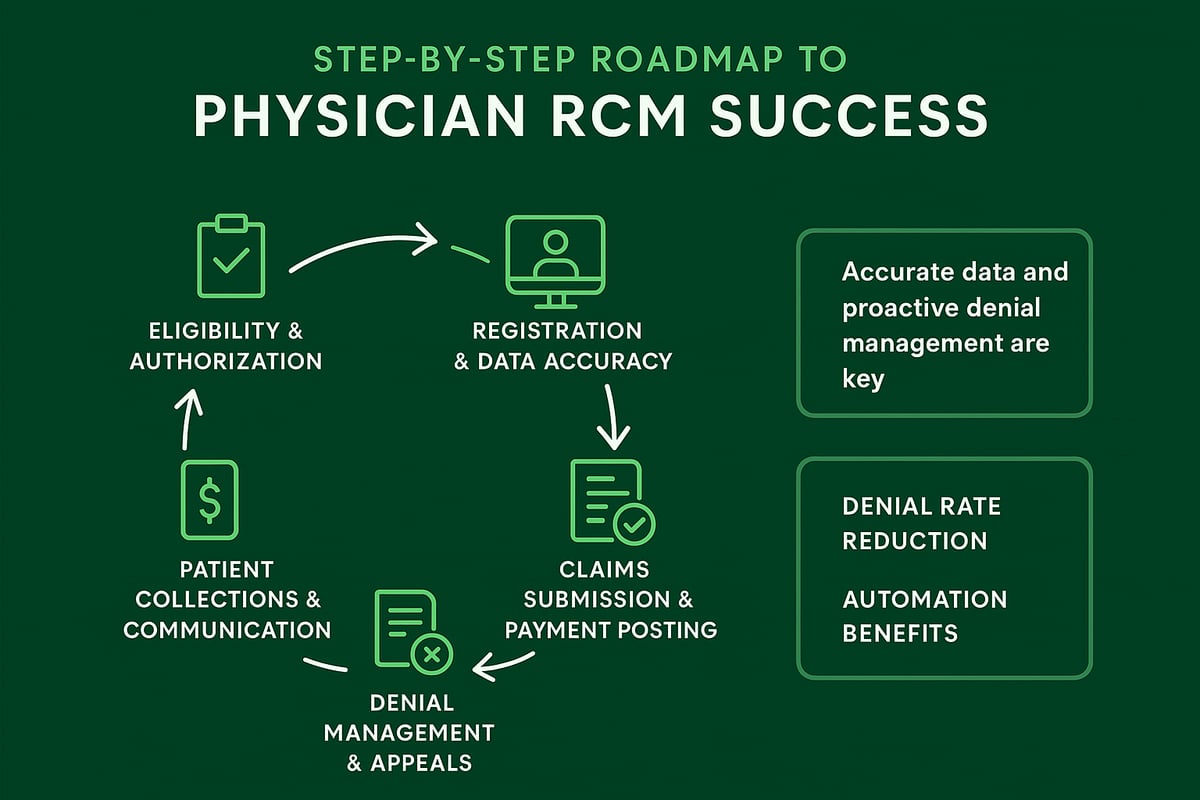
Step 1: Pre-Visit Optimization—Eligibility & Authorization
The first step in physician rcm is confirming insurance eligibility and securing prior authorizations before the patient visit. This prevents costly claim denials and reduces the risk of payment delays. Automated eligibility checks not only save staff time but also improve accuracy.
Streamlining prior authorization is critical. By adopting digital tools and standardized workflows, practices can minimize manual errors and accelerate approvals. For a deeper dive into this process, review Prior authorization in medical billing for proven strategies.
A real-world example: Practices that automate eligibility verification see measurable reductions in denied claims, leading to a smoother revenue cycle.
Step 2: Patient Registration & Data Accuracy
Accurate patient registration forms the backbone of physician rcm. Collecting complete demographic and insurance details at the outset ensures downstream billing processes run smoothly.
To reduce registration errors, implement double-check protocols and regular staff training. Digital registration platforms can prompt for missing data, minimizing omissions.
Consider this scenario: Incorrect patient details can result in claim rejections, impacting revenue and delaying payments. Prioritizing data accuracy at registration safeguards the entire revenue cycle.
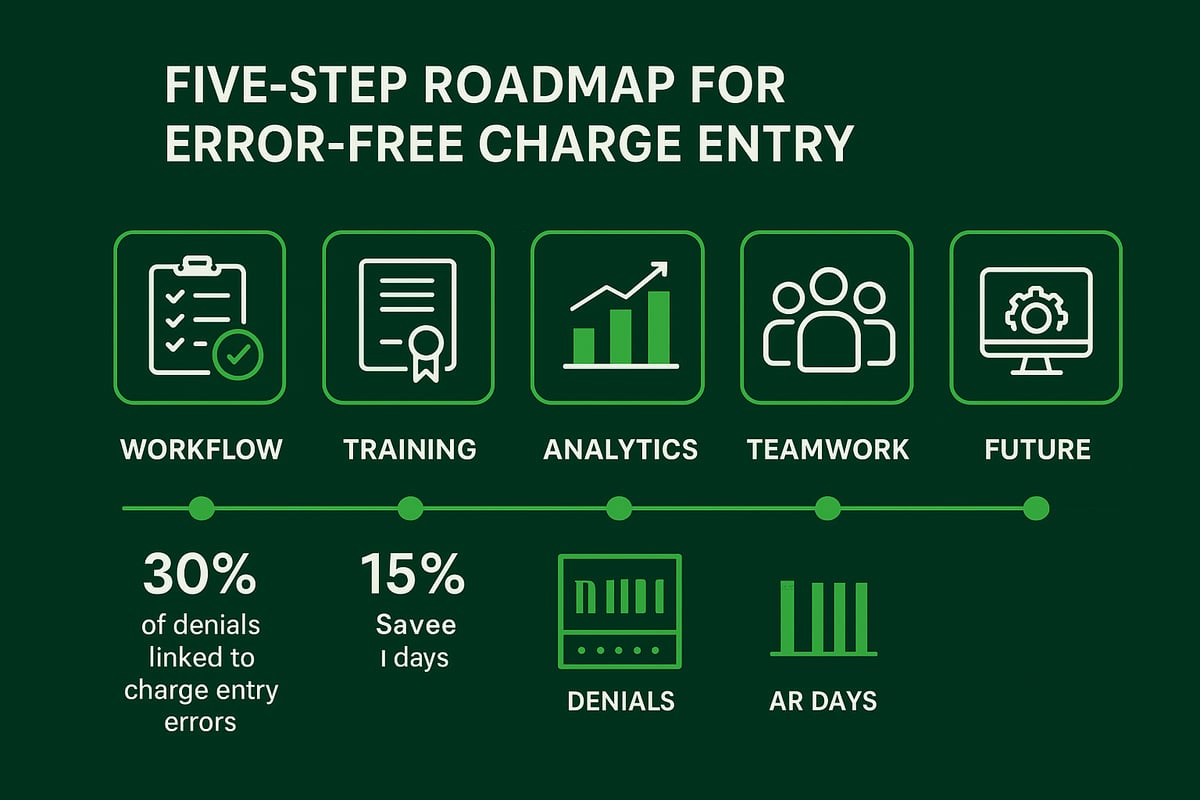
Step 3: Charge Capture and Medical Coding Best Practices
Timely and accurate charge capture is a cornerstone of physician rcm. All rendered services must be documented promptly to avoid missed revenue opportunities.
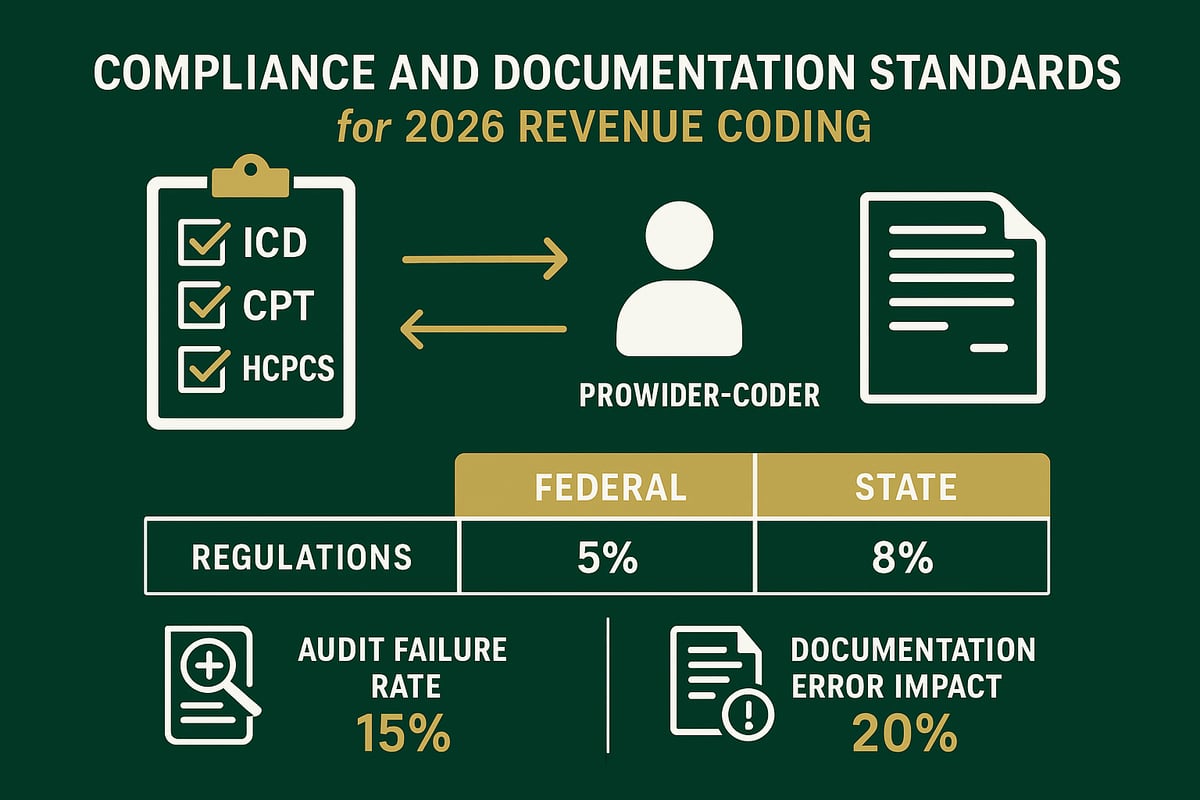
Adherence to ICD-10, CPT, and HCPCS coding standards is essential. Conduct regular coding audits to ensure compliance and identify areas for improvement.
For example, practices that perform routine coding reviews experience fewer denials and reduced compliance risks. Investing in skilled coders and robust audit processes protects your bottom line.
Step 4: Claims Submission and Payment Posting
Efficient claims submission is vital for physician rcm success. Submitting clean claims expedites reimbursement and keeps cash flow steady.
Leverage clearinghouses and automated claim scrubbing to detect errors before submission. Timely payment posting allows for fast reconciliation and identification of outstanding balances.
Consider this: Practices using clearinghouses report faster claims processing and fewer rejections. This proactive approach ensures revenue is captured without unnecessary delays.
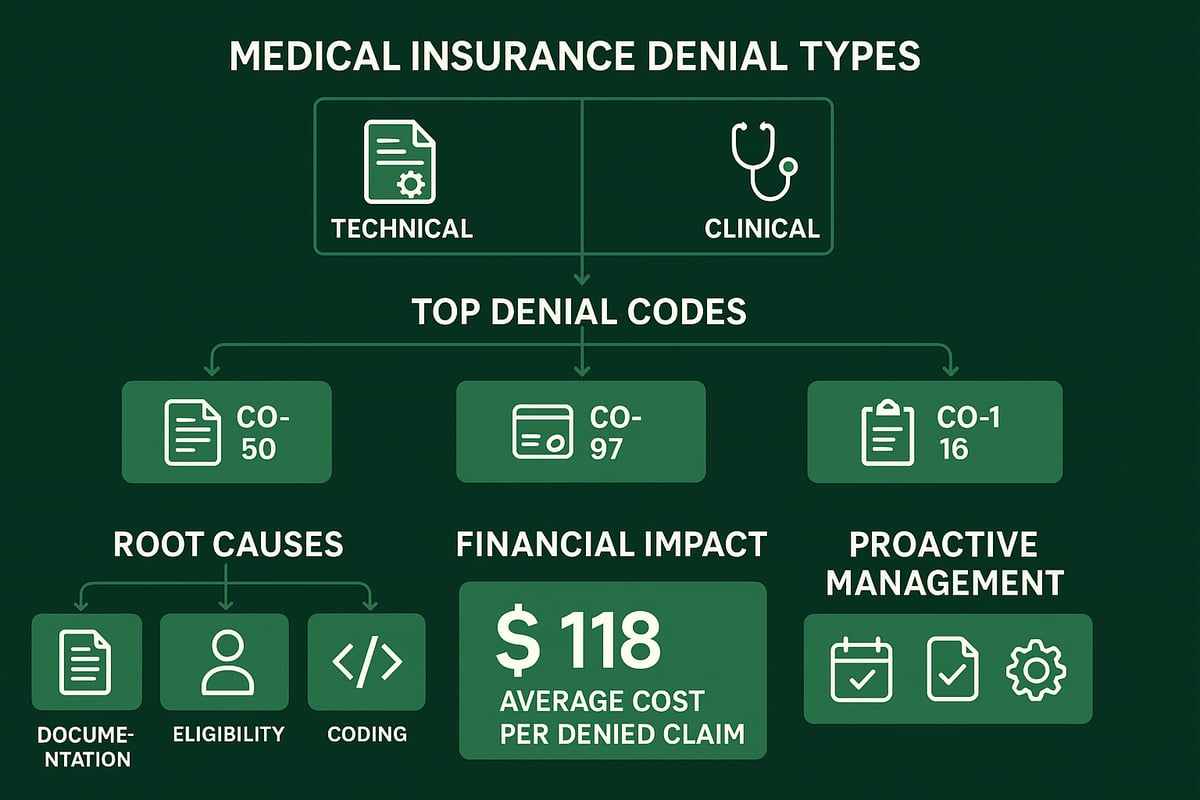
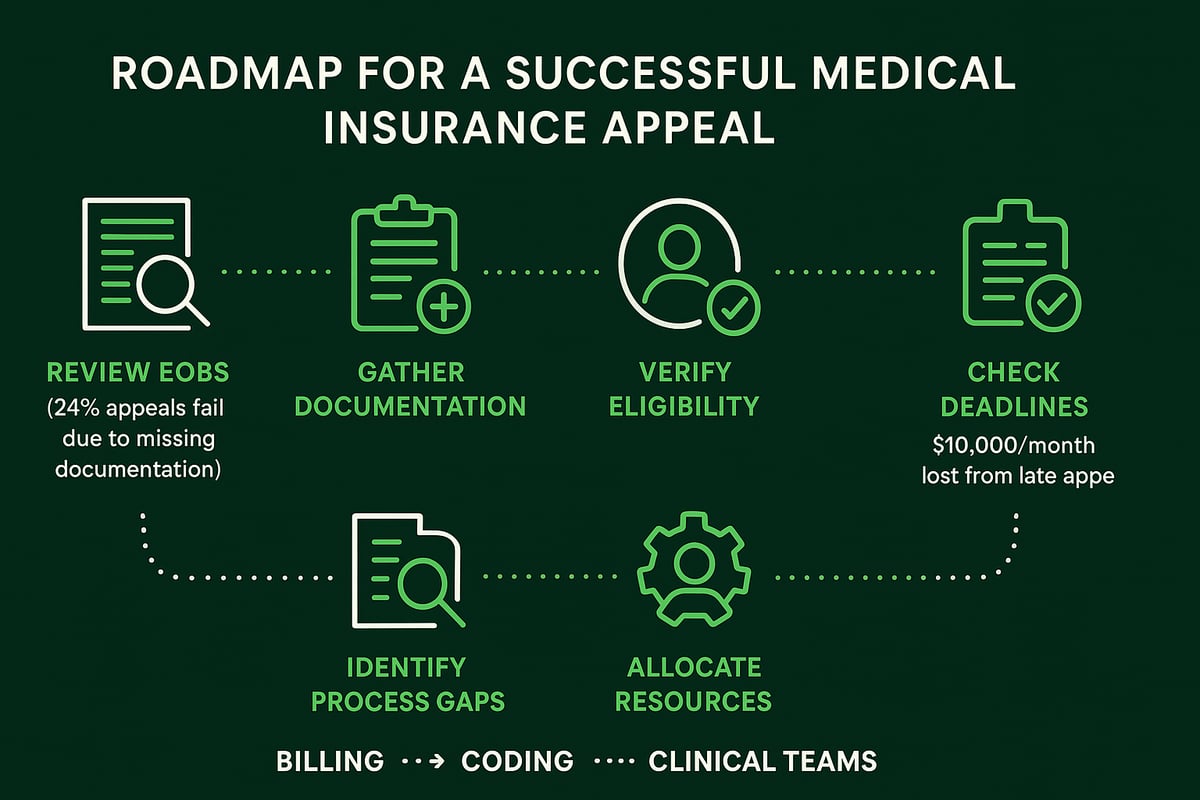
Step 5: Denial Management and Appeals
Proactive denial management is a critical component of physician rcm. Identifying the most frequent reasons for denials—whether eligibility, coding, or authorization—enables targeted improvements.
Establish a systematic process for analyzing denials and submitting timely appeals. Data shows that with effective denial management, practices can reduce denial rates by up to 50 percent.
By tracking trends and educating staff, organizations transform denials into learning opportunities, strengthening revenue cycle performance.
Step 6: Patient Collections and Financial Communication
The final step in physician rcm is optimizing patient collections and financial communication. Clear, transparent billing statements and flexible payment options encourage prompt payments.
Offer digital payment channels to meet patient preferences and increase collection rates. Transparent financial policies and proactive communication minimize confusion and foster trust.
For example, practices implementing online payment portals and payment plans report higher patient satisfaction and improved collection outcomes.
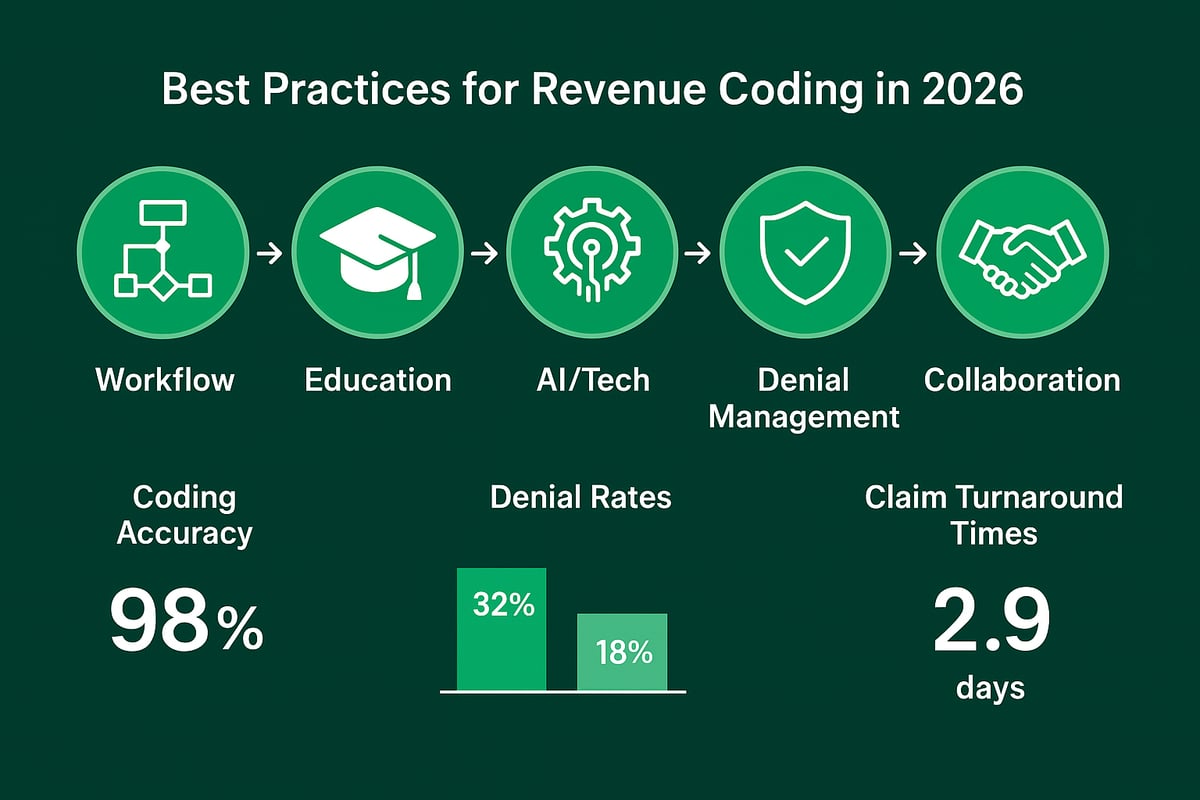
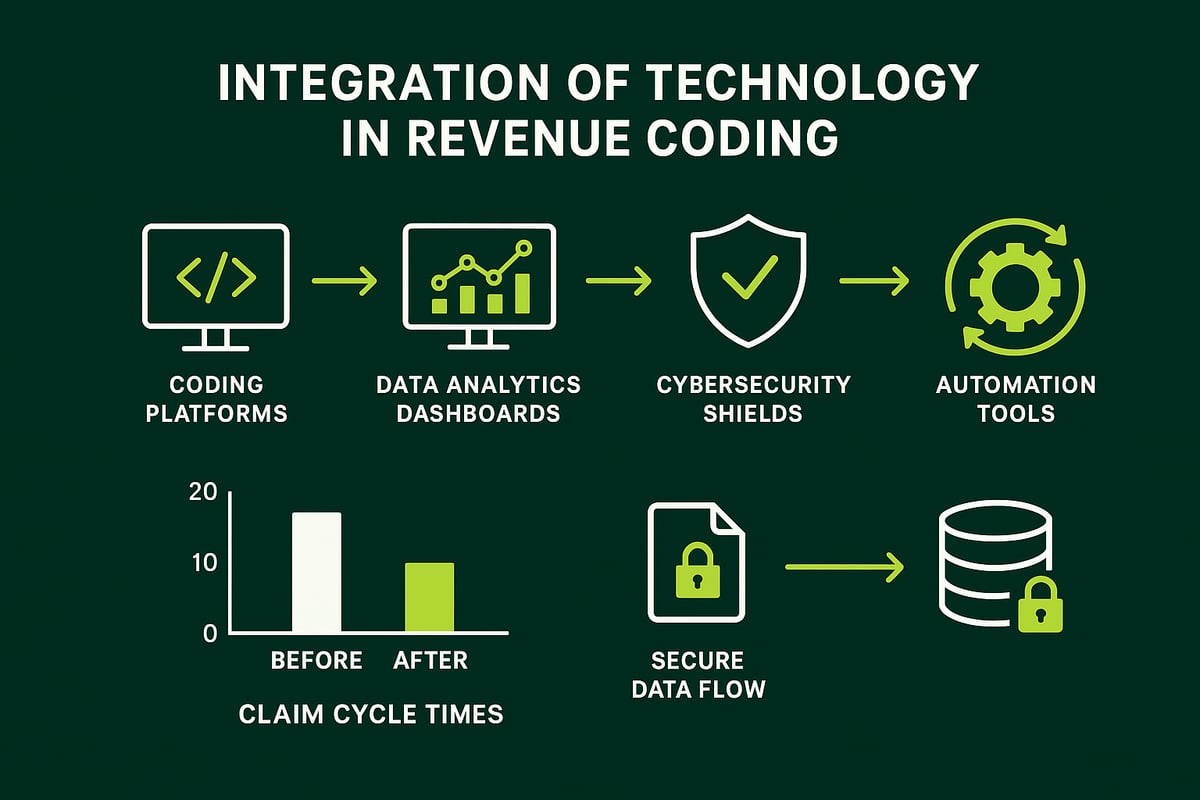
Leveraging Technology and Automation in Physician RCM
Technology is transforming physician rcm by streamlining workflows, reducing errors, and enabling a data-driven approach to revenue optimization. As the healthcare industry advances, leveraging automation and analytics is essential for maximizing collections, improving compliance, and minimizing operational costs. Below, we explore how digital solutions and emerging technologies are shaping the future of physician rcm.
![]()
The Role of Practice Management Systems and EHR Integration
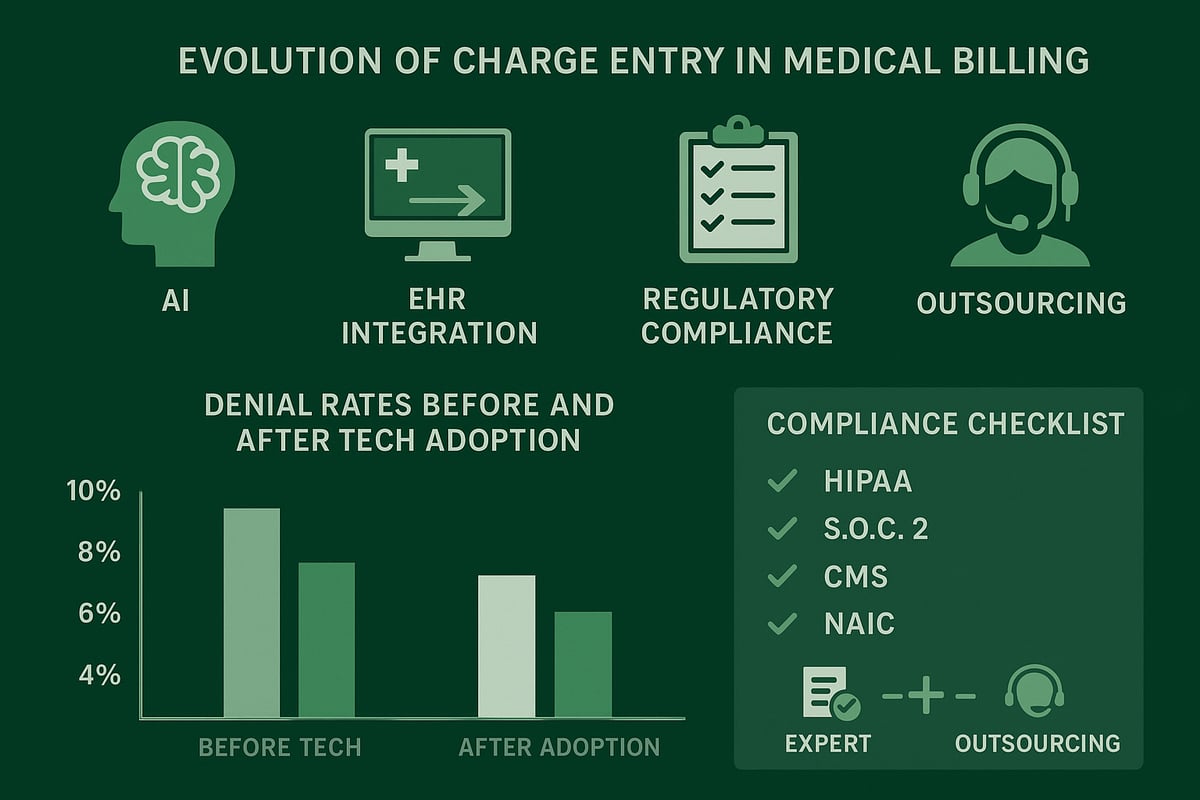
Modern physician rcm relies on seamless integration between Practice Management (PM) systems and Electronic Health Records (EHR). This connectivity enables real-time data exchange, eliminating manual data entry and reducing errors at every stage of the revenue cycle. Features such as automated eligibility verification and demographic validation allow staff to confirm insurance coverage instantly. For example, integrated EHR platforms can prompt staff when information is missing, reducing denied claims and improving overall physician rcm efficiency. These integrated systems also support compliance by maintaining audit trails and centralizing patient records for quick access.
Automation Tools for Claims Processing and Denial Management
Automation is a game-changer for physician rcm, especially in high-volume practices. Automated claims processing tools extract charge data directly from clinical documentation, validate codes, and submit claims electronically, reducing turnaround time by up to 30 percent. Denial management solutions flag issues early, allowing staff to resolve them before submission. Automated worklists prioritize claims that need attention, while batch processing accelerates payment cycles. By minimizing manual intervention, practices can focus on value-added tasks, ultimately driving better financial outcomes and freeing up resources for patient care.
Analytics and Reporting for Revenue Optimization
Data analytics is central to effective physician rcm. Dashboards and reporting tools provide visibility into key performance indicators such as denial rates, days in accounts receivable, and collection ratios. Practices can use this information to identify trends, spot bottlenecks, and benchmark against industry standards. For example, tracking denial patterns helps target process improvements and training needs. Leveraging healthcare revenue cycle analytics allows practices to make informed decisions that boost profitability and operational efficiency. Consistent use of analytics empowers leadership to set measurable goals and drive continuous improvement in physician rcm.
Cybersecurity and HIPAA Compliance in RCM Technology
As physician rcm becomes more digitized, protecting patient data is non-negotiable. HIPAA-compliant platforms use encryption, multi-factor authentication, and robust access controls to safeguard Protected Health Information (PHI). Regular vulnerability assessments and security audits are essential for maintaining compliance and mitigating cyber threats. Staff must be trained on privacy policies and incident response procedures to ensure quick action in case of breaches. By prioritizing cybersecurity, physician rcm providers build trust with clients and reduce the risk of costly penalties or reputational damage.
Adapting to Emerging Technologies (AI, RPA)
The future of physician rcm will be shaped by artificial intelligence (AI) and robotic process automation (RPA). AI-driven tools can assist with complex coding, flagging potential errors, and suggesting corrections in real time. RPA solutions automate repetitive tasks such as claims status checks, freeing staff for higher-level analysis. Some practices already use predictive analytics to forecast denials and optimize collection strategies. As these technologies evolve, physician rcm will become more proactive, resilient, and responsive to regulatory changes, ensuring long-term success for healthcare providers.
Compliance, Regulatory Updates, and Risk Management
Keeping up with compliance is essential for any physician rcm strategy. With new regulations and ongoing risk factors, practices must remain proactive. A strong compliance framework not only protects your organization but also supports financial health and operational efficiency.
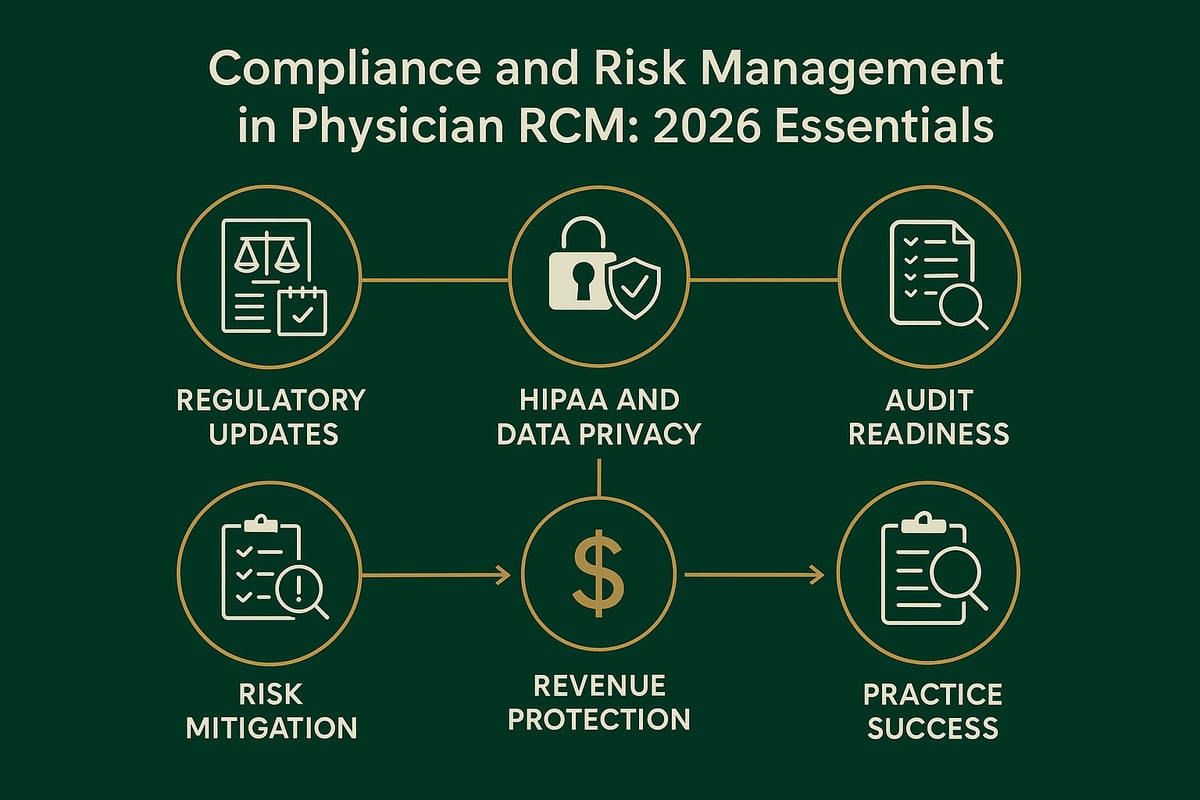
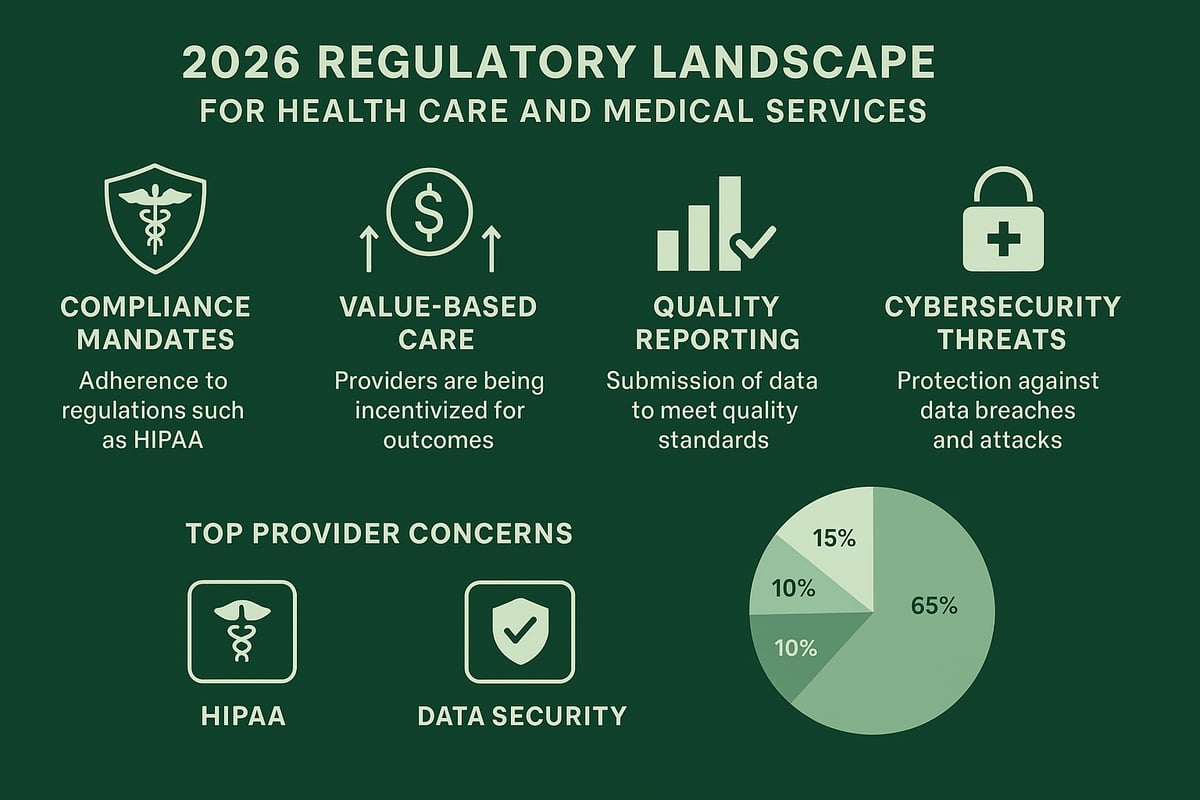
Navigating 2026 Regulatory Changes
The regulatory landscape for physician rcm is evolving rapidly as 2026 approaches. Practices must prepare for updates like expanded price transparency, new CMS billing rules, and stricter interoperability mandates. These changes impact billing workflows and demand timely adaptation.
For example, compliance with the No Surprises Act and adjustments for updated MIPS and MACRA reporting will require close attention. Staying current with regulations is not just about avoiding penalties—it is key to securing reimbursements and maintaining trust with payers.
Access to reliable data, such as the 2023 Physician Billing Report, helps practices benchmark their compliance efforts and identify gaps. Proactive planning gives your team a competitive edge in physician rcm.
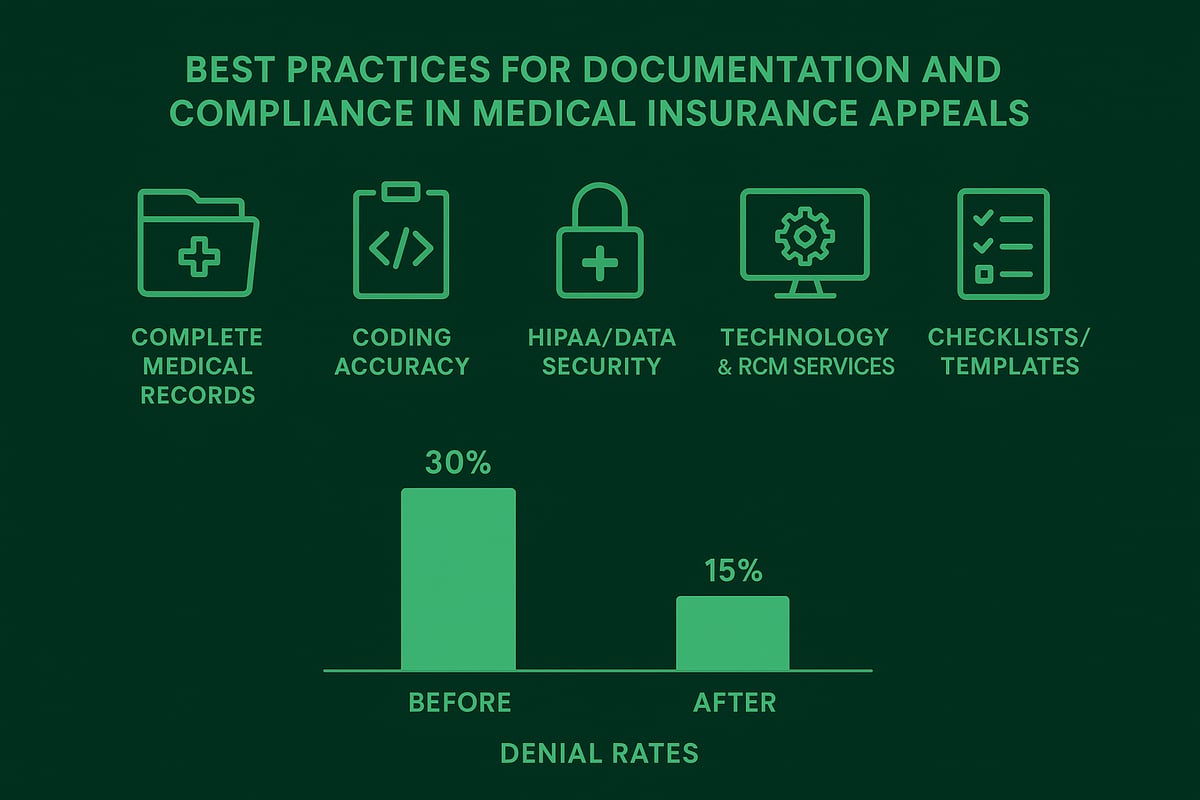
HIPAA, Data Security, and Privacy Considerations
Protecting patient information is non-negotiable in physician rcm. HIPAA compliance remains at the center of every billing and revenue cycle process. Practices must secure all protected health information (PHI), whether stored digitally or in physical records.
Implementing strong access controls, encryption, and regular staff training helps minimize the risk of data breaches. The financial and reputational consequences of non-compliance can be severe, including regulatory fines and loss of patient trust.
A robust privacy policy, paired with routine security audits, is essential for every physician rcm operation. Prioritizing data security safeguards your practice and ensures uninterrupted revenue flow.
Risk Mitigation Strategies for Physicians
Effective risk management is a cornerstone of physician rcm success. Internal audits, ongoing staff education, and compliance checklists help detect and prevent costly errors before they impact revenue.
Best practices include:
- Conducting quarterly coding audits to catch mistakes early
- Updating policies as regulations change
- Providing regular compliance training for all billing staff
These steps reduce the likelihood of claim denials, fines, or payment delays. A proactive approach allows physician rcm teams to address vulnerabilities and maintain financial stability.
Documentation and Audit Readiness
Thorough documentation is critical for audit preparedness in physician rcm. Payers and government agencies are increasing their scrutiny of billing practices, making it vital to keep records accurate and up to date.
Key actions include:
- Maintaining detailed records of all billing activities
- Organizing supporting documentation for claims
- Reviewing files regularly to ensure completeness
Being audit-ready not only protects against penalties but also supports smoother reimbursement processes. Consistent documentation practices are a hallmark of an effective physician rcm program.
Expert Strategies for Maximizing Physician Revenue in 2026
Maximizing revenue in the evolving healthcare landscape requires a proactive and strategic approach to physician rcm. By leveraging expert strategies, physician practices can protect financial health, improve collections, and ensure long-term sustainability. Explore these six proven strategies for optimizing physician rcm in 2026.
Revenue Leakage Prevention and Recovery
Revenue leakage is a persistent challenge in physician rcm, often resulting in significant lost income. Common sources include missed charges, under-coding, and uncollected patient balances. To address these issues, practices should implement robust charge capture protocols and regular coding audits.
For example, coding errors or incomplete documentation frequently lead to denied claims or underpayments. Proactive denial management is crucial. Leveraging Denial management in medical billing strategies, such as root cause analysis and timely appeals, can recover lost revenue and reduce future denials. Continuous monitoring and process improvement are essential for sustainable revenue integrity in physician rcm.
Optimizing Payer Contract Negotiations
Contract negotiations with payers are a vital component of successful physician rcm. Analyzing current contracts, benchmarking rates, and understanding payer mix are key steps. Practices that regularly renegotiate agreements often see up to an 8% increase in reimbursement rates.
Effective negotiation involves reviewing terms for prompt payment, timely dispute resolution, and clear definitions of covered services. Data-driven insights help identify underperforming contracts and opportunities for improvement. A strategic approach to payer relationships ensures physician rcm remains aligned with financial goals and market trends.
Enhancing Patient Financial Experience
A positive patient financial experience is increasingly important in physician rcm. Transparent billing, clear communication, and flexible payment options build trust and improve collection rates. Practices can benefit from offering digital payment portals, multilingual support, and itemized statements.
According to the Power-up your private practice’s revenue-cycle management guide, focusing on patient engagement and process automation leads to higher satisfaction and faster payments. By prioritizing convenience and clarity, physician rcm professionals can reduce confusion and minimize outstanding balances.
Staff Training and Performance Management
Continuous staff education is essential for maintaining compliance and maximizing efficiency in physician rcm. Billing and coding teams should participate in certification programs and regular training sessions to stay updated on regulatory changes and best practices.
Performance monitoring, including productivity metrics and quality audits, helps identify areas for improvement. Investing in staff development leads to fewer errors, faster reimbursement, and increased morale. Well-trained teams are the backbone of effective physician rcm and ensure consistent, accurate revenue cycle processes.
Outsourcing RCM: When and Why to Consider It
Outsourcing can be a strategic option for physician rcm, especially for practices facing resource constraints or complex billing environments. Outsourced RCM providers offer specialized expertise, scalable staffing, and advanced analytics, often resulting in improved collections and lower denial rates.
Consider the following comparison:
| Factor | In-House RCM | Outsourced RCM |
|---|---|---|
| Upfront Costs | Higher | Lower |
| Staffing Flexibility | Limited | High |
| Technology Investment | Practice-funded | Provider-supplied |
| Expertise | Variable | Specialized |
Before choosing to outsource, evaluate practice needs, budget, and desired outcomes. The right partner can transform physician rcm operations for sustainable growth.
Greenhive Billing Solutions: Your Trusted RCM Partner
Greenhive Billing Solutions delivers comprehensive physician rcm services tailored to the unique needs of medical practices. Our offerings include insurance eligibility verification, claims processing, denial management, and advanced revenue analytics.
We operate with strict HIPAA compliance and employ certified experts to ensure accurate billing and maximum reimbursements. Our transparent, results-based pricing model means no setup fees or hidden costs, just measurable improvements in collections and reduced denials.
Seamless integration with existing EHR and PM systems enables smooth transitions for busy practices. Each client receives a dedicated account manager and 24/7 support for personalized physician rcm service. Partner with Greenhive Billing Solutions to unlock your practice’s full revenue potential.
Future Trends and Innovations in Physician RCM
Staying ahead in physician rcm requires awareness of emerging trends and a proactive approach to change. As the healthcare landscape evolves, practices that anticipate and adapt to new developments will remain competitive. Let's explore the innovations shaping the future of physician rcm.
The Shift to Value-Based Care and Alternative Payment Models
Value-based care is redefining physician rcm, requiring a move from fee-for-service to outcome-driven reimbursement. This transition introduces bundled payments and shared savings models, which align incentives with patient outcomes. Practices must update processes to capture quality metrics and report on care coordination. Adapting to these models demands robust data tracking and collaboration with payers. According to Top 10 Revenue Cycle Management Trends in Healthcare, staying current with these trends is critical for long-term revenue optimization and compliance. Physician rcm teams that embrace value-based contracts are better positioned for sustainable growth.
Interoperability and Data Exchange
Seamless data sharing is a cornerstone of modern physician rcm. Regulatory mandates in 2026 will push providers to adopt interoperable systems for exchanging information with payers, laboratories, and other care partners. Effective interoperability reduces claim errors, supports coordinated care, and helps meet reporting requirements. By investing in secure data exchange, practices can accelerate reimbursement cycles and enhance patient experiences. As interoperability becomes standardized, physician rcm providers must ensure their workflows integrate with diverse platforms, minimizing manual entry and maximizing data accuracy for every transaction.
Consumerization of Healthcare and Digital Payments
Patients expect convenient, transparent billing experiences, making digital payment solutions essential for physician rcm. The rise of mobile billing, online portals, and automated reminders empowers patients to manage their financial responsibilities with ease. Practices benefit from faster collections and reduced administrative overhead. Offering clear statements and flexible payment plans can boost patient satisfaction and loyalty. Embracing consumer-friendly technologies not only streamlines revenue collection but also positions physician rcm services as adaptable to evolving patient preferences in a competitive healthcare market.
Artificial Intelligence and Predictive Analytics
Artificial intelligence is transforming physician rcm by automating complex tasks such as coding, claim scrubbing, and denial prediction. Predictive analytics tools identify revenue risks before they impact cash flow, enabling proactive interventions. AI-driven insights help practices target process improvements, reducing bad debt and increasing net collections. As highlighted in the Top 10 Revenue Cycle Management Trends in Healthcare, leveraging these technologies can deliver measurable results. For B2B physician rcm, integrating AI and analytics elevates decision-making and operational efficiency.
Preparing for the Next Era of Physician RCM
To remain competitive in the future, physician rcm providers must prioritize adaptability and continuous improvement. This means monitoring regulatory changes, adopting proven innovations, and investing in staff training. Building a future-ready strategy involves partnering with experienced professionals who understand market dynamics and can deliver tailored solutions. As the healthcare revenue cycle management market is projected to grow significantly, forward-thinking practices will benefit from scalable, compliant, and patient-centric RCM services. Embracing change today ensures success in the dynamic landscape of 2026 and beyond.
As you look ahead to 2026, staying ahead in physician revenue cycle management means being proactive about challenges like regulatory changes, technology integration, and evolving patient expectations. Whether you want to strengthen compliance, streamline your billing processes, or maximize your reimbursements, having the right partner can make all the difference. We understand how complex and demanding RCM can be, and we’re here to help you navigate every step. If you’re ready to optimize your financial performance and reduce administrative headaches, let’s talk about how we can support your goals.
Book Your Free Consultation