The healthcare insurance landscape is changing at a record pace. Is your organization ready to pay medical insurance efficiently in 2026? Staying ahead of new payment models, regulatory shifts, and technology is critical.
This guide provides healthcare professionals with a clear roadmap to pay medical insurance with confidence. Learn how to evaluate insurance types, adapt to evolving payment models, and implement actionable strategies that maximize reimbursements and reduce risk.
Urgent changes are coming. Discover how new technologies and payment systems can help your practice lower costs, minimize denials, and improve financial outcomes. Apply these insights today to secure your organization’s financial success in the years ahead.
Understanding the 2026 Medical Insurance Landscape
The 2026 landscape for those who pay medical insurance is more complex than ever. Healthcare organizations must stay agile, adapting to regulatory shifts, evolving payment models, and an increasingly digital world. This section unpacks the major forces shaping your financial and operational strategies over the next year.
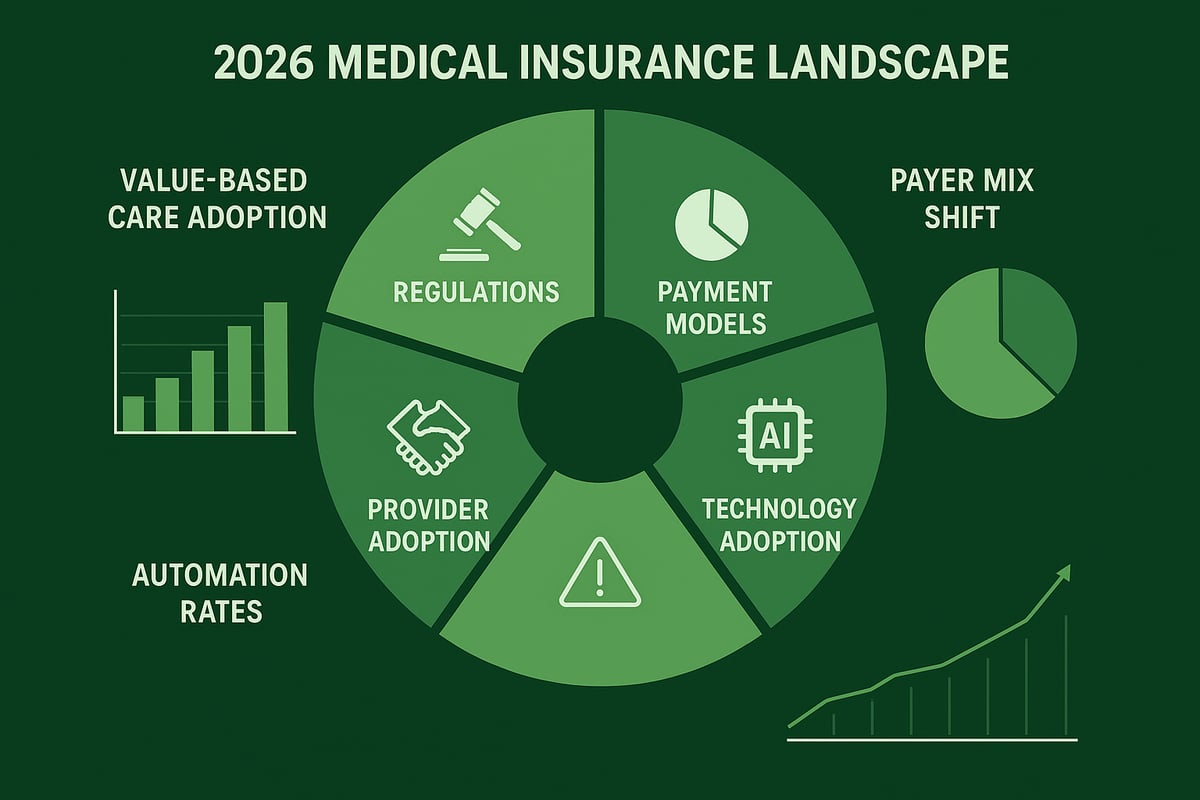
Key Changes in Insurance Regulations and Policies
Healthcare practices seeking to pay medical insurance efficiently in 2026 face significant regulatory shifts. Updates to the Affordable Care Act, Medicaid expansion, and surprise billing laws are reshaping compliance requirements nationwide. New payer mandates demand stricter claims documentation and faster submissions, while interoperability rules require seamless integration between EHR systems and payers.
For example, the No Surprises Act now enforces stricter protections against unexpected billing, and telehealth coverage rules continue to evolve. According to recent data, over 70% of practices report being affected by these 2026 policy changes. To stay informed, review the 2025 Marketplace Integrity and Affordability Final Rule for insight into how these updates will impact your processes and compliance standards.
Evolving Insurance Payment Models
The way organizations pay medical insurance is shifting from traditional fee-for-service to value-based care, bundled payments, and capitation models. Accountable Care Organizations (ACOs) and risk-sharing contracts are gaining traction, rewarding providers for quality outcomes rather than volume of services.
Value-based models offer incentives for efficient, high-quality care but may introduce financial risk for underperformance. In contrast, fee-for-service remains predictable but can increase administrative burden. For instance, a primary care group transitioning to value-based reimbursement saw improved patient outcomes and a 15% boost in net collections, illustrating the potential upside of embracing new payment models.
Trends in Commercial and Government Payer Mix
Understanding shifts in payer mix is crucial for those who pay medical insurance and manage revenue streams. Medicare Advantage enrollment is projected to rise, while some insurers are scaling back plan offerings. Medicaid managed care continues its expansion, and high-deductible health plans remain popular in the employer-sponsored market.
By 2026, industry forecasts estimate Medicare Advantage will make up nearly 50% of all Medicare enrollments. Such trends can significantly impact practice revenue, requiring organizations to adjust their payer strategies to maintain stability and growth in a dynamic environment.
| Payer Type | Projected Share 2026 |
|---|---|
| Medicare Advantage | 48% |
| Medicaid MCOs | 22% |
| Commercial Plans | 30% |
The Role of Technology and Automation
Embracing automation is transforming how organizations pay medical insurance and manage the revenue cycle. AI-powered tools now streamline claims processing, payment reconciliation, and eligibility verification, reducing manual errors and administrative overhead. Real-time eligibility checks and automated prior authorizations help practices secure payments faster and minimize denials.
A recent industry survey found that over 60% of practices have adopted some form of automation in their revenue cycle management. Practices leveraging these technologies report up to a 20% reduction in claim denial rates, underscoring the importance of automation for operational efficiency and financial performance.
Challenges Facing Healthcare Providers
Even with new tools, challenges persist for those who pay medical insurance in 2026. Increased administrative demands, complex multi-payer contracts, and evolving documentation requirements add layers of difficulty. Practices often cite delayed payments, frequent denials, and underpayments as top pain points.
A recent survey revealed that 68% of healthcare organizations consider managing denials and navigating regulatory changes their primary concerns for the upcoming year. Addressing these issues requires a proactive approach, leveraging expert RCM support and continuous process improvement to ensure financial health.
Step-by-Step Guide: How to Pay and Manage Medical Insurance in 2026
Navigating how to pay medical insurance efficiently in 2026 requires a clear, actionable strategy. As regulatory demands and payer requirements evolve, healthcare organizations must adapt quickly to ensure financial health and compliance. This step-by-step guide outlines essential actions for B2B healthcare professionals to streamline payment workflows, minimize denials, and maximize revenue.
![]()
Step 1: Assess Your Practice’s Insurance Needs
Begin by evaluating your patient population and service portfolio. Analyze demographics, payer mix, and specialty-specific requirements. For example, a pediatric practice will have different considerations than an orthopedic clinic when deciding how to pay medical insurance on behalf of patients.
Assess whether being in-network or out-of-network with particular payers will benefit your organization. Review prior year claims data to identify which insurance types yield the best reimbursement rates and patient satisfaction. This foundational step helps you tailor your participation strategy for optimal results.
Step 2: Evaluate Available Insurance Plans and Networks
Compare plan types such as PPO, HMO, EPO, POS, Medicare Advantage, and Medicaid MCOs. Determine which options align with your clinical services and business goals. Examine reimbursement rates, coverage limitations, and network stability for each option as you decide how to pay medical insurance efficiently.
| Plan Type | Flexibility | Reimbursement | Network Breadth |
|---|---|---|---|
| PPO | High | Moderate | Broad |
| HMO | Low | Higher | Narrow |
| Medicare Adv. | Moderate | Varies | Expanding |
Analyze leading commercial payers in 2026 to select those with strong reputations and reliable payment histories.
Step 3: Verify Patient Eligibility and Benefits
Before each visit, conduct real-time eligibility checks to confirm coverage, copays, and deductibles. This step reduces claim denials and accelerates payments as you pay medical insurance for your patients. Use automated verification tools and follow eligibility verification best practices to streamline the process.
Key tips:
- Verify coverage at every encounter
- Document copay and deductible information
- Use integrated platforms for timely updates
Robust eligibility processes can significantly lower claim denial rates and administrative workload.
Step 4: Optimize Claims Submission and Payment Collection
Submit claims electronically using standardized formats such as EDI and 837P/I. Meeting payer-specific filing deadlines and avoiding common errors is crucial to pay medical insurance without delays. Employ claim scrubbing and pre-adjudication tools to ensure clean submissions.
Best practices:
- Validate all coding before submission
- Monitor claim rejection trends
- Follow up on pending payments proactively
Efficient claims management shortens payment cycles and improves cash flow for your practice.
Step 5: Manage Denials, Appeals, and Underpayments
Identify the main causes for denials in 2026, such as coding errors, lack of medical necessity, or missing prior authorizations. When you pay medical insurance, track denial trends and implement a structured appeals process for various payers.
Denial management steps:
- Review and categorize all denials
- Submit appeals with supporting documentation
- Analyze patterns to prevent future issues
Industry data shows that proactive denial management can recover a significant portion of previously lost revenue.
Step 6: Stay Compliant with Evolving Regulations
Keep pace with regulations such as HIPAA, the No Surprises Act, and price transparency mandates. Regularly train staff on compliance updates and conduct internal audits to ensure you pay medical insurance in accordance with legal requirements.
Compliance checklist:
- Update policies as laws change
- Educate staff on new documentation standards
- Use risk assessments to identify vulnerabilities
A practice fined for non-compliance in 2025 highlights the importance of ongoing vigilance in this area.
Step 7: Leverage Data Analytics for Financial Optimization
Utilize analytics to monitor payer performance, reimbursement trends, and contract value. By tracking key performance indicators, you can identify high-value contracts and renegotiation opportunities to pay medical insurance more strategically.
Important KPIs:
- Days in accounts receivable (A/R)
- Denial rates
- Net collection percentages
Practices that leverage analytics-driven strategies have seen measurable improvements in margins and operational efficiency.
Comparing Payment Models: Fee-for-Service vs. Value-Based Care
Selecting the right payment model is crucial for healthcare organizations aiming to efficiently pay medical insurance and enhance financial stability in 2026. The landscape is more dynamic than ever, and understanding how each model impacts cash flow, compliance, and patient outcomes is essential.
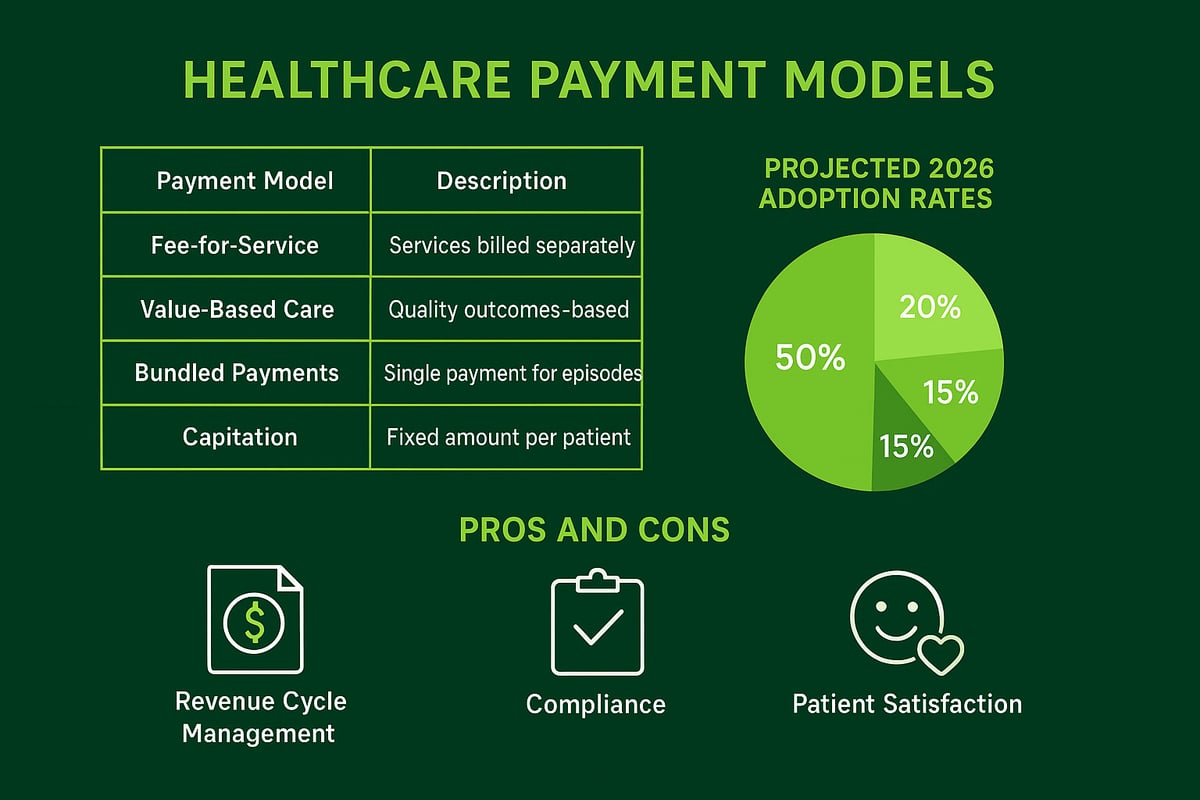
Overview of Payment Models in 2026
In 2026, healthcare practices have several options for structuring how they pay medical insurance and receive reimbursements. The main models include fee-for-service, value-based care, bundled payments, and capitation.
Fee-for-service remains familiar, rewarding providers for each service delivered. However, the shift toward value-based care is accelerating, with 64% of organizations expecting increased adoption by 2025, as highlighted by this survey. Bundled payments and capitation are also gaining traction, providing alternative ways to manage costs and outcomes.
Understanding the prevalence and growth rates of each model helps organizations align their strategies with industry trends and payer expectations.
Pros and Cons for Providers
Each payment model affects how organizations pay medical insurance and manage their revenue cycles. Below is a summary:
| Model | Pros | Cons |
|---|---|---|
| Fee-for-Service | Predictable revenue, simple structure | High admin burden, incentivizes volume |
| Value-Based Care | Rewards quality, reduces waste | Risk of lower payments, complex reporting |
| Bundled Payments | Streamlined payments, potential savings | Cost overruns if not managed well |
For example, a multi-specialty group that transitioned to value-based contracts saw improved patient outcomes but faced challenges with data reporting and risk sharing.
Financial and Operational Considerations
When deciding how to pay medical insurance under different models, organizations must address several operational areas:
- Revenue cycle impact: New billing, coding, and documentation requirements.
- Staff training: Teams must understand new workflows and quality metrics.
- Technology investment: Tracking performance and compliance requires robust analytics.
- ROI: Many practices report improved margins after implementing value-based contracts.
Evaluating these factors helps practices determine readiness and avoid unexpected disruptions during transitions.
Choosing the Right Model for Your Organization
There is no one-size-fits-all solution for how practices pay medical insurance. Assessing organizational readiness, patient population needs, and payer relationships is vital.
Negotiating favorable contracts and considering hybrid approaches can help mitigate risk. For instance, a large clinic may blend fee-for-service and value-based contracts to balance stability with quality incentives.
Hybrid models provide flexibility and support smoother adaptation in a shifting regulatory environment.
Case Studies: Transitioning to New Payment Models
A small family medicine practice embraced value-based care in 2025, leading to higher patient satisfaction scores and reduced unnecessary procedures. Their success stemmed from investing in better data analytics and ongoing staff education to support their pay medical insurance strategies.
However, not all transitions are seamless. Common pitfalls include underestimating reporting needs and failing to renegotiate payer contracts. Learning from industry peers can help organizations avoid costly mistakes and maximize results.
Navigating Regulatory and Compliance Challenges
Healthcare providers face an increasingly complex regulatory environment as they strive to pay medical insurance efficiently in 2026. Keeping up with evolving rules, documentation standards, and payer requirements is critical to avoid penalties and optimize reimbursement. Let’s explore the major compliance hurdles and how to overcome them.
![]()
Key 2026 Regulatory Changes Impacting Payments
The regulatory landscape for those who pay medical insurance will shift dramatically in 2026. Significant updates to HIPAA, the Affordable Care Act, and state-level rules will require providers to adapt swiftly. Price transparency mandates are top of mind, with the Centers for Medicare & Medicaid Services introducing new hospital price transparency policy changes effective January 1, 2026.
Other changes include stricter billing disclosure requirements and enhanced enforcement of the No Surprises Act. Practices must also adjust to telehealth policy updates and expanded Medicaid coverage in several states. Staying proactive about these regulations is essential for organizations aiming to pay medical insurance accurately and compliantly.
Best Practices for Compliance Management
To pay medical insurance and maintain compliance, healthcare organizations need robust management protocols. Developing comprehensive compliance checklists helps ensure all regulatory bases are covered. Ongoing staff education is vital, as rules and payer expectations continue to evolve.
Many practices benefit from engaging compliance consultants or leveraging managed services to streamline audits. Regular internal reviews can catch issues early and prevent costly mistakes. By prioritizing compliance as a core operational goal, organizations strengthen their ability to pay medical insurance without unnecessary risk.
Common Pitfalls and How to Avoid Them
Common pitfalls when trying to pay medical insurance compliantly include incomplete documentation, outdated policies, and insufficient staff training. Manual errors, such as incorrect coding or missing disclosures, can trigger audits or denials.
Table: Common Compliance Pitfalls
| Pitfall | Solution |
|---|---|
| Incomplete documentation | Regular documentation audits |
| Outdated policies | Update protocols annually |
| Coding errors | Ongoing coder education |
| Manual processing | Leverage RCM service providers |
Addressing these pitfalls ensures providers can pay medical insurance efficiently and minimize compliance risks.
Preparing for Future Regulatory Shifts
Preparing to pay medical insurance in the years ahead means anticipating future changes. Monitor legislative updates, subscribe to payer bulletins, and participate in industry associations for early insights.
Agile processes and adaptable workflows will help practices pivot when new rules are introduced. Building a culture of compliance readiness ensures your organization is always prepared to pay medical insurance and meet regulatory demands, regardless of what the future holds.
Technology and Automation in Medical Insurance Payments
Automation has become a cornerstone for organizations seeking to pay medical insurance efficiently in 2026. As the industry evolves, leveraging advanced technology is no longer optional but essential for optimizing payment workflows and maintaining compliance.
The Rise of Automation in Revenue Cycle Management
Healthcare providers are rapidly adopting automation tools to streamline the revenue cycle. Automated solutions now handle tasks such as eligibility verification, claims submission, and payment posting, which significantly reduces manual errors and administrative costs.
Key benefits include:
- Faster payment cycles
- Improved accuracy in claims processing
- Lower operational costs
Industry data shows that practices using automation see up to a 30% increase in efficiency. For organizations striving to pay medical insurance seamlessly, leveraging medical insurance claims processing services can be a game changer.
Integrating AI and Machine Learning
Artificial intelligence is reshaping how providers pay medical insurance by enhancing every stage of the claims lifecycle. AI-driven tools predict claim denials, automate coding, and reconcile payments with impressive accuracy.
Use cases include:
- Predicting and preventing denials before submission
- Automating claim status follow-ups
- Identifying revenue leakage in real time
Practices utilizing AI in their workflows report a measurable increase in clean claim rates. The result is a more reliable and transparent process for managing insurance payments and maximizing reimbursements.
Streamlining Eligibility Verification and Prior Authorization
Verifying patient eligibility is critical to pay medical insurance correctly and avoid costly denials. Automated real-time checks ensure every visit is covered, reducing manual workload and improving the patient experience.
Modern platforms:
- Instantly confirm coverage and copay details
- Automate prior authorization requests
- Reduce claim denials due to eligibility errors
Data reveals that robust eligibility verification can decrease denial rates by over 20 percent, directly impacting a practice’s bottom line.
Cybersecurity and Data Protection
As technology adoption increases, so does the risk of cyber threats. Protecting patient and practice data is essential for any organization that aims to pay medical insurance securely and maintain regulatory compliance.
Best practices include:
- Implementing HIPAA-compliant security protocols
- Conducting regular risk assessments and staff training
- Using advanced encryption and multi-factor authentication
Recent breaches highlight the need for a proactive security strategy. Investing in data protection safeguards both financial operations and patient trust.
Selecting the Right Technology Partners
Choosing the right technology partner is vital for successful automation and integration. Providers should evaluate vendors based on their experience, interoperability with existing systems, and level of support.
Key criteria:
- Proven track record in healthcare RCM
- Seamless integration with EHR and billing platforms
- Access to knowledgeable support teams
A thoughtful selection process ensures that your pay medical insurance workflows remain agile, compliant, and future-ready.
Maximizing Financial Performance: Strategies for 2026
Achieving optimal financial results in 2026 requires healthcare organizations to refine every aspect of their revenue cycle. To successfully pay medical insurance, practices must negotiate favorable contracts, streamline billing, invest in ongoing staff training, leverage outsourced expertise, and closely track performance metrics. Here are the essential strategies for maximizing your financial outcomes in a rapidly evolving landscape.
Contract Negotiation and Payer Relations
Strong contract negotiation is foundational for any organization aiming to pay medical insurance efficiently. Begin by reviewing your current payer contracts and preparing for renewal discussions well in advance. Focus on reimbursement rates, timely payment terms, and clear dispute resolution procedures.
Key terms to address during negotiations include:
- Fee schedules and carve-outs
- Timely filing and payment deadlines
- Denial and appeal processes
- Value-based care incentives
For example, a mid-sized clinic improved its revenue by renegotiating rates with its top three payers, resulting in a 15% increase in collections over 12 months. Building positive payer relationships and understanding your leverage can make a measurable difference in your financial outcomes.
Revenue Cycle Optimization Techniques
To pay medical insurance more effectively, practices must streamline both front-end and back-end billing operations. Start with accurate patient registration, eligibility verification, and pre-authorization checks. On the back end, ensure claims are coded correctly and submitted promptly.
Consider these optimization steps:
- Regularly audit workflows for bottlenecks
- Implement claim scrubbing and pre-adjudication services
- Standardize denial and appeal management processes
Outsourcing denial management can be especially beneficial. For deeper insight, see how denial management in medical billing improves cash flow and accelerates reimbursements. Optimized workflows decrease days in A/R and reduce costly errors, supporting your ability to pay medical insurance on time.
Staff Training and Continuous Education
Investing in staff education is critical for financial success as you pay medical insurance in 2026. Well-trained employees minimize coding mistakes, reduce denials, and ensure compliance with evolving regulations.
Best practices for ongoing education:
- Schedule quarterly training on coding and billing updates
- Encourage certification (e.g., CPC, CPB) for billing staff
- Provide compliance training for all team members
For instance, a multi-specialty group that implemented a certification program saw claim accuracy rates climb by 20%. Creating a culture of accountability and learning ensures your team stays current and agile.
Leveraging Outsourced Revenue Cycle Management Services
Outsourcing revenue cycle management (RCM) can offer significant advantages for practices seeking to pay medical insurance more efficiently. RCM service providers bring specialized expertise, scalability, and proven compliance protocols.
Benefits of outsourcing include:
- Access to experienced billing professionals
- Ability to adapt quickly to payer changes
- Improved collections and reduced administrative burden
When selecting a partner, prioritize those with a track record of seamless integration, transparent communication, and strong industry references. Outsourcing is especially valuable for organizations lacking in-house RCM expertise or facing rapid growth.
Monitoring KPIs and Benchmarking Performance
Continuous performance monitoring is vital for organizations aiming to pay medical insurance with maximum efficiency. Key performance indicators (KPIs) such as denial rates, net collection percentages, and days in A/R provide actionable insights.
Use dashboards and analytics to track:
| KPI | Best Practice Target |
|---|---|
| Denial Rate | <5% |
| Net Collection Rate | >95% |
| Days in A/R | <35 |
Advanced analytics help identify trends, benchmark against peers, and drive strategic improvements. Explore how revenue cycle analytics for practices can empower your team to react quickly and exceed industry standards. Ultimately, regular KPI tracking enables smarter decisions and better financial outcomes as you pay medical insurance in 2026.
As we’ve explored, the world of medical insurance payments in 2026 is full of new regulations, evolving payment models, and fast-changing technology. Navigating these complexities is no small feat, but with the right guidance, you can confidently optimize your practice’s financial performance and ensure compliance every step of the way. If you’re ready to take the next step in transforming your revenue cycle or have questions about specific challenges your organization faces, let’s connect. You deserve a tailored approach that fits your unique needs—Book Your Free Consultation and let’s build a smarter strategy together.