Oncology practices today are navigating a landscape shaped by rising costs, complex payer requirements, and evolving treatment protocols. As cancer care continues to advance, financial and regulatory demands are only increasing.
This guide to oncology revenue cycle management offers healthcare professionals a clear roadmap for optimizing financial performance and ensuring operational efficiency. Inside, you will discover proven strategies for managing every phase of the oncology revenue cycle, from patient intake through reimbursement.
Explore real-world solutions for overcoming billing challenges, leveraging technology, meeting compliance requirements, and maximizing collections. Gain expert insights to streamline workflows and empower your oncology practice for long-term success.
Understanding the Oncology Revenue Cycle
The oncology revenue cycle management process begins the moment a patient schedules an appointment and continues through to the final payment. Unlike general medical billing, oncology practices must navigate a web of unique complexities, including multiple overlapping treatments like chemotherapy, radiation, and infusion therapies. Each of these services brings its own set of codes and payer rules, which change frequently and require constant vigilance.
Accurate charge capture and thorough documentation are crucial in oncology revenue cycle management, especially for high-value and high-frequency services. Missing a single detail can trigger claim denials, delayed reimbursements, or even compliance risks. For example, a coding error in chemotherapy billing may result in significant revenue loss and additional administrative burden.
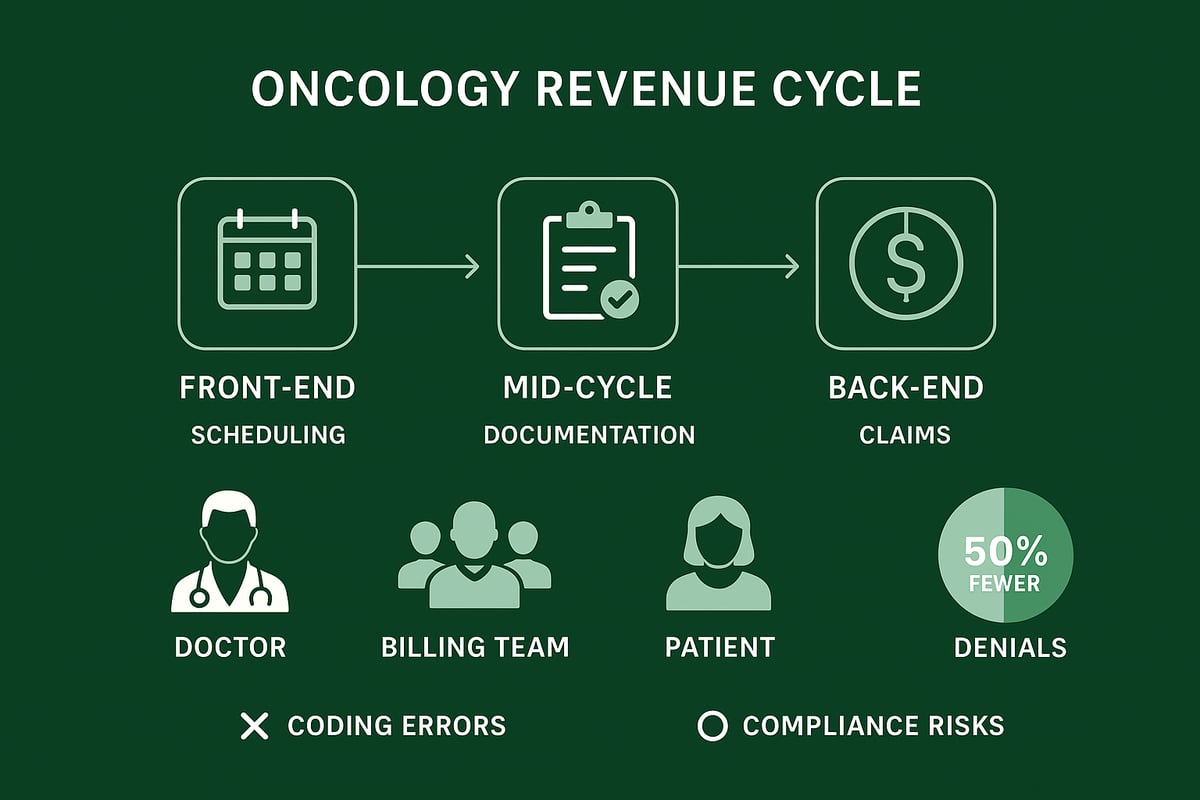
Stakeholders involved in this process include:
- Physicians, who provide clinical care and documentation
- Billing teams, responsible for coding, charge capture, and claim submission
- Payers, who review and reimburse claims
- Patients, who may face out-of-pocket costs and require transparent communication
Errors at any stage can have cascading effects. Claim denials and payment delays are common, but with optimized oncology revenue cycle management processes, practices have reported up to 50% fewer denials according to IDS Healthcare.
To better understand the workflow, the oncology revenue cycle can be divided into three main phases: front-end (scheduling, eligibility verification), mid-cycle (documentation, coding), and back-end (claims submission, payment posting, and denial management). For a detailed breakdown of these stages, visit the Revenue cycle medical billing process resource.
A well-structured approach to managing each phase helps practices minimize errors, maximize reimbursements, and maintain compliance.
Step-by-Step Oncology Revenue Cycle Management Process
Navigating the oncology revenue cycle management process requires a clear, structured approach. Each phase—from patient access to claim resolution—demands attention to detail and collaboration from multiple stakeholders. Let’s break down the journey into three critical stages.
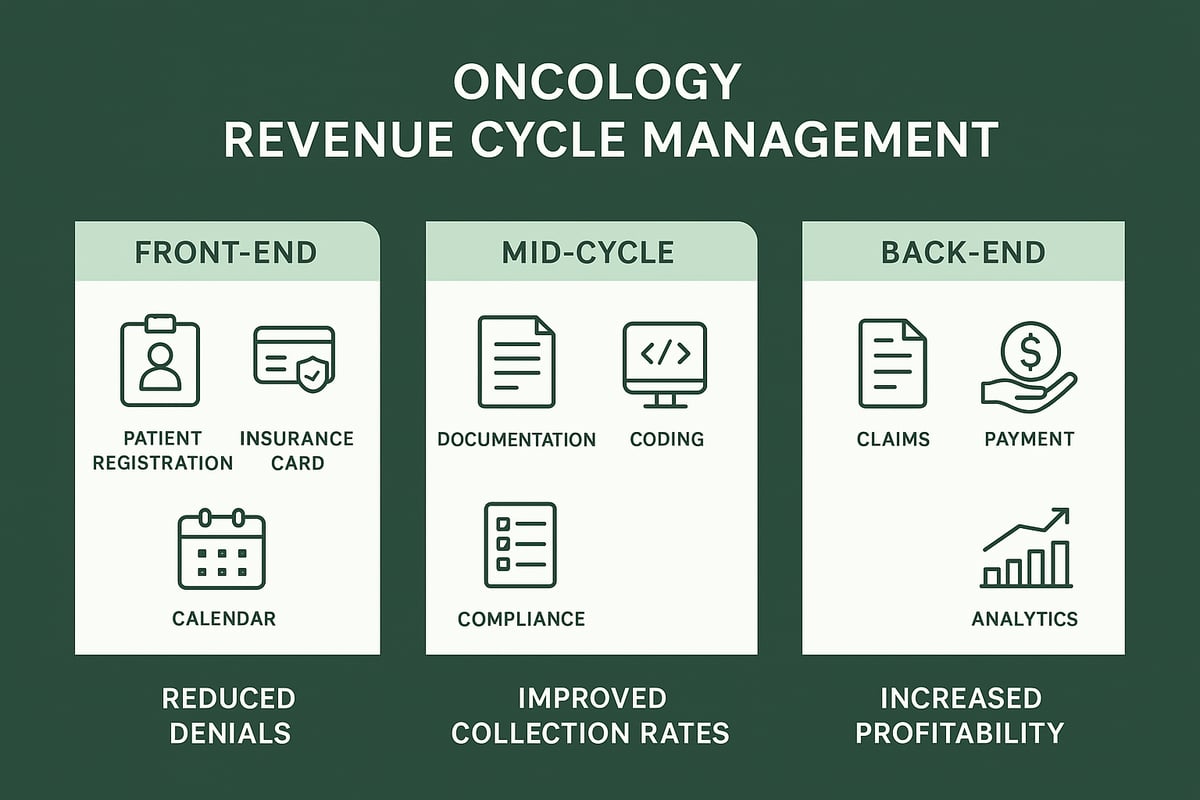
Front-End: Patient Access and Eligibility Verification
The first phase of oncology revenue cycle management centers on accurately capturing patient information and confirming insurance eligibility. This step is crucial for preventing denials before care even begins.
By verifying coverage and securing prior authorizations for complex oncology treatments, practices reduce administrative errors and delays. Automated eligibility checks streamline workflows, allowing staff to focus on patient care. For example, implementing real-time verification tools can cut down manual workload and speed up patient onboarding.
Mid-Cycle: Documentation, Coding, and Charge Capture
During the mid-cycle, thorough clinical documentation and precise coding are essential for accurate billing. Certified coders play a vital role in assigning correct ICD-10, CPT, and HCPCS codes, ensuring all oncology services are properly recorded.
Effective charge capture strategies help prevent lost revenue, especially for bundled or high-cost therapies. Staying compliant with evolving guidelines and MIPS requirements is also critical. Leveraging medical coding revenue cycle management services can further reduce errors and support ongoing education for staff. AI-assisted scribing and pre-charting tools are valuable for easing clinician workload and improving accuracy.
Back-End: Claims Submission, Payment Posting, and Denial Management
The final stage of oncology revenue cycle management focuses on submitting clean claims, posting payments promptly, and managing denials proactively. Timely claims submission reduces rejection rates and speeds up reimbursement.
Accurate payment posting allows for real-time revenue tracking, while analytics identify recurring issues and optimize collections. Proactive denial management—such as investigating root causes and appealing denied claims—helps maximize revenue. By continuously monitoring these activities, oncology practices can enhance financial performance and reduce compliance risks.
Technology and Automation in Oncology RCM
The rapid adoption of technology is transforming oncology revenue cycle management. Practices are leveraging AI and automation to streamline billing workflows, cut administrative tasks, and boost accuracy. By integrating with over 40 EHR and EMR platforms, these solutions enable seamless data exchange, which reduces bottlenecks and improves the patient experience.
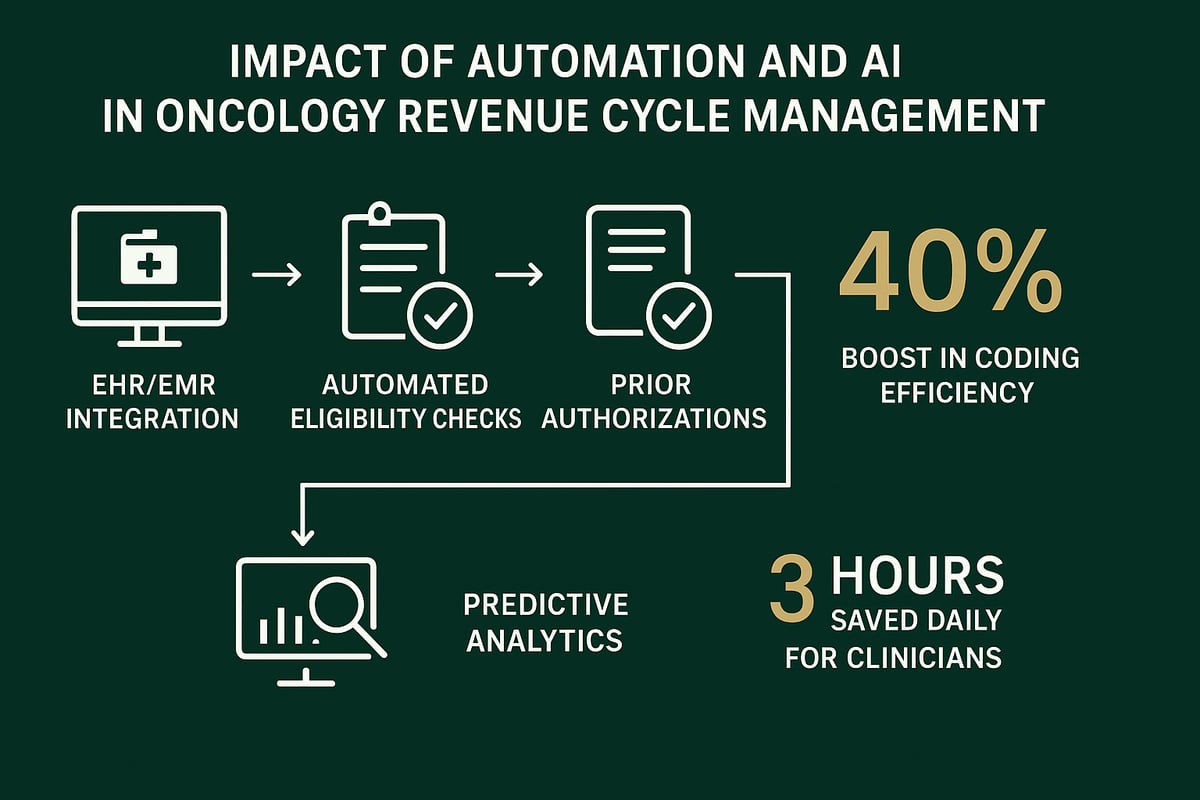
Automated eligibility verification and prior authorization tools help prevent costly denials before patient visits. AI-driven claim scrubbing and coding engines improve clean claim rates by identifying errors in real time. These advances not only reduce manual workload but also lead to significant cost savings. For example, clinics using AI-powered RCM solutions reported annual savings exceeding $50,000.
The table below summarizes the core benefits of technology in oncology revenue cycle management:
| Benefit | Impact |
|---|---|
| Coding efficiency | 40% increase, fewer errors |
| Clinician time saved | 3 hours daily |
| Denial reduction | Fewer rejections, faster reimbursement |
| Seamless EHR/EMR integration | Improved data flow and workflow |
| Predictive analytics | Identifies denial trends, optimizes cash flow |
Predictive analytics further empower practices to monitor claim patterns, proactively address denial trends, and improve cash flow. When evaluating new technology, it is crucial to match solutions to the size and specialty of your practice. For deeper insights into mastering these advances, consider resources like Achieving Revenue Cycle Management Mastery.
By embracing automation and analytics, oncology revenue cycle management becomes more efficient, accurate, and profitable for your organization.
Compliance and Regulatory Considerations for Oncology RCM
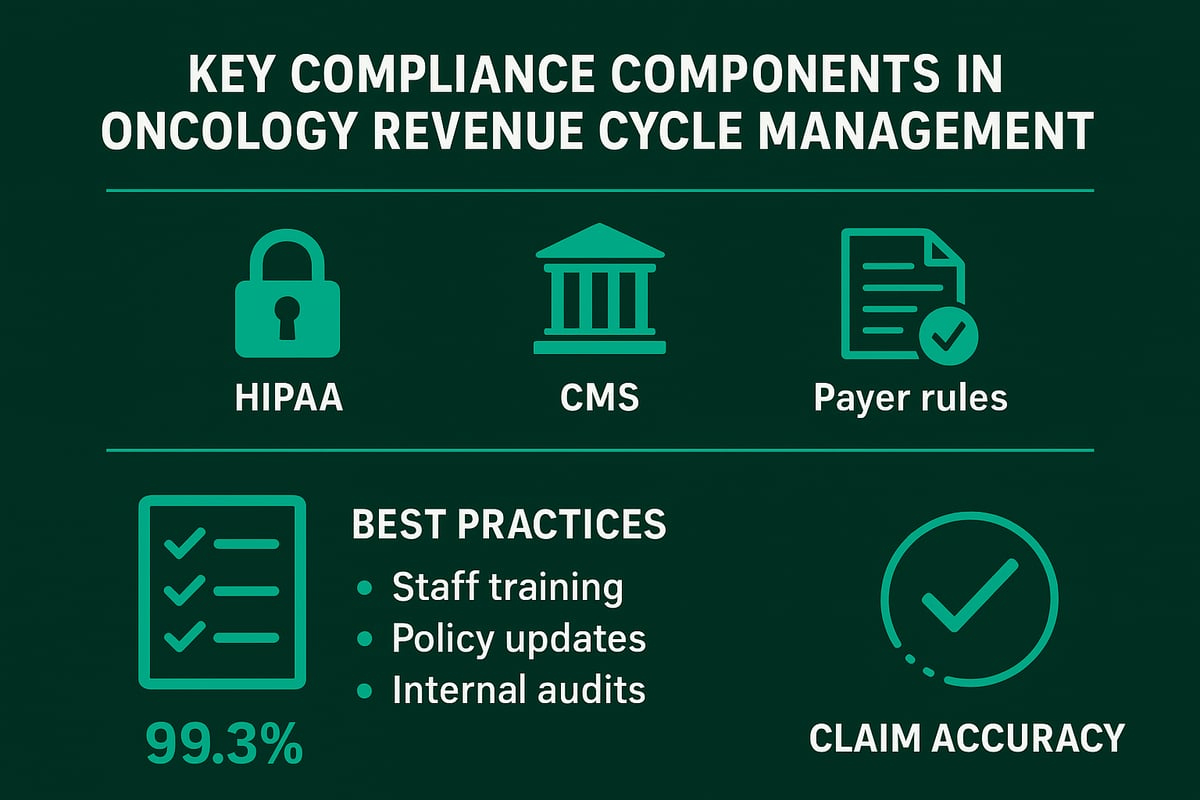
Maintaining compliance is a cornerstone of effective oncology revenue cycle management. Practices must navigate a complex landscape of regulations, including HIPAA, CMS guidelines, and payer-specific rules. Each regulation shapes the requirements for documentation, billing accuracy, and patient data security.
To ensure audit readiness, oncology providers should prioritize complete, timely, and secure clinical records. Regularly reviewing and updating policies helps teams stay aligned with the latest coding and reimbursement changes. Non-compliance can result in denied claims, financial penalties, and reputational harm.
Best practices for compliance include:
- Ongoing staff training on current regulations
- Frequent policy reviews and updates
- Conducting internal audits for early error detection
Understanding revenue cycle management compliance risks and implementing mitigation strategies is essential for reducing vulnerabilities in oncology revenue cycle management.
Many oncology centers using compliant RCM services report a 99.3 percent accuracy rate in claim submissions, highlighting the measurable value of a proactive approach.
Measuring Success: Key Metrics and Performance Benchmarks
To drive financial performance, oncology revenue cycle management relies on precise measurement and continuous improvement. Tracking the right metrics enables practices to spot inefficiencies, benchmark against industry standards, and ultimately maximize reimbursements.
Core KPIs for Oncology RCM
| Metric | Industry Benchmark |
|---|---|
| Clean Claim Rate | 95% or higher |
| Denial Rate | Below 10% |
| Days in AR | Fewer than 30 days |
| Net Collection Rate | 96% or higher |
Analytics dashboards play a vital role in oncology revenue cycle management. With real-time access to trends and performance indicators, leaders can quickly identify areas for process improvement. For a deeper dive into optimizing these KPIs, review Healthcare revenue cycle analytics.
Regular performance monitoring has a direct impact on operational efficiency. Practices leveraging data-driven strategies have achieved up to 18% improvements in accounts receivable and reduced AR days by two weeks. Consistent reporting and transparent communication with stakeholders ensure everyone is aligned on revenue goals and progress.
As you’ve seen throughout this guide, optimizing every step of your oncology revenue cycle—from accurate patient intake and coding to denial management and compliance—can make a measurable difference in your practice’s financial health. If you’re ready to identify missed opportunities or want expert advice tailored to your unique workflows, you don’t have to navigate these complexities alone. We’re here to help you boost efficiency, maximize reimbursements, and reduce administrative headaches. \
Take the next step: Get Your Free Audit and see how your oncology practice can thrive in 2026 and beyond.