The healthcare revenue cycle management industry is rapidly evolving as providers face increasing complexity, regulatory demands, and technological change. Effective RCM is crucial for healthcare organizations to maintain financial stability and deliver high-quality patient care. As the industry adapts to new payer models and compliance requirements, professionals must navigate these shifts with confidence and expertise. This comprehensive guide is designed for healthcare professionals and administrators seeking to optimize every aspect of their revenue cycle. We will explore key RCM components, market trends, regulatory considerations, proven best practices, and future outlook to empower your organization’s financial success.
Healthcare Revenue Cycle Management Industry Overview
The healthcare revenue cycle management industry has become a cornerstone of financial sustainability for providers and organizations across the care continuum. As the business of healthcare grows more complex, mastering the revenue cycle is essential for optimizing cash flow and supporting quality patient care.
Definition and Scope of RCM
The healthcare revenue cycle management industry focuses on overseeing the entire financial process from patient registration through final payment collection. RCM ensures accurate billing, timely claims submission, and effective collection of reimbursements. This process involves both services performed by expert teams and the use of specialized software. For a detailed breakdown of each component, see this Revenue cycle medical billing overview. The distinction between RCM services and software is crucial, as many organizations rely on service providers to manage complex workflows.
Key Market Drivers and Challenges
Several forces are shaping the healthcare revenue cycle management industry. Growing patient volumes, evolving insurance plans, and regulatory requirements drive demand for robust RCM solutions. Providers face staffing shortages and increased administrative tasks that strain internal resources. At the same time, payer mix shifts add complexity to reimbursement. Organizations must navigate these challenges while maintaining compliance and optimizing financial outcomes.
Market Size and Growth Projections
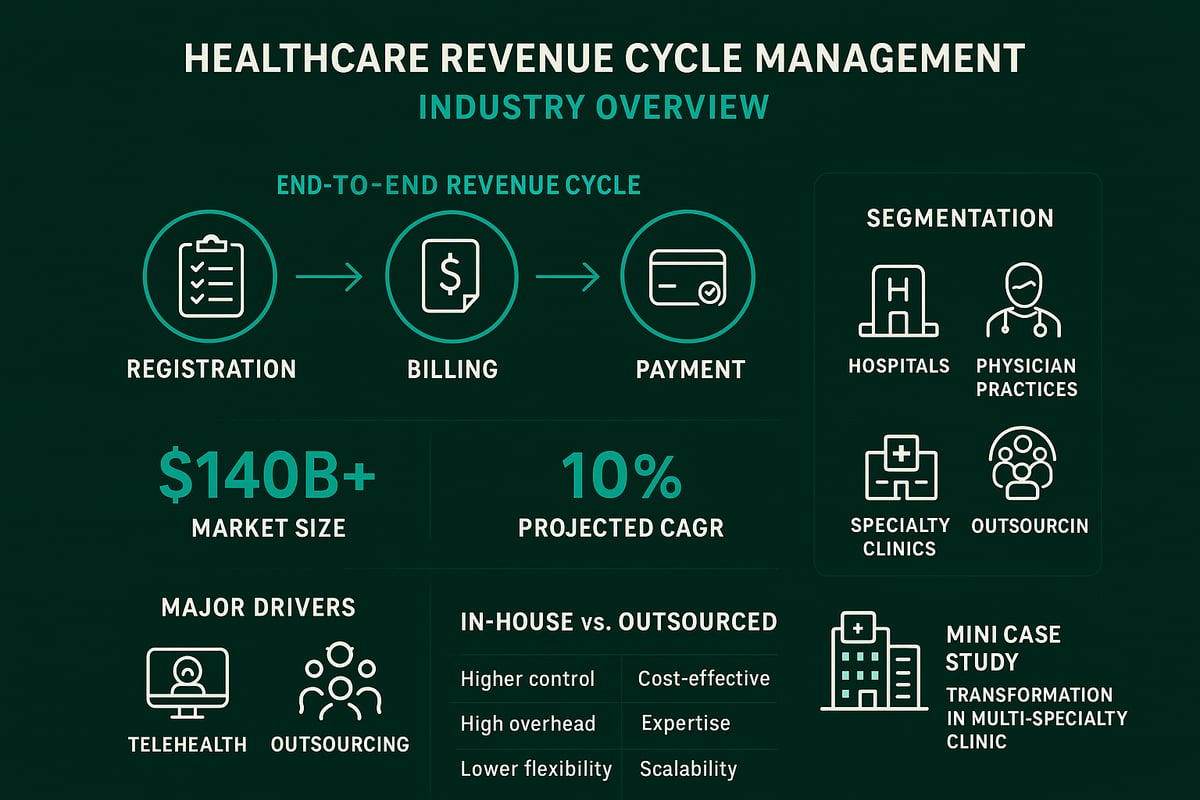
The healthcare revenue cycle management industry is experiencing rapid expansion. Recent research values the global market at more than $140 billion, with a projected compound annual growth rate exceeding 10 percent. This upward trend is fueled by the adoption of telehealth, the outsourcing of RCM functions, and the ongoing shift to value-based care. As healthcare delivery models evolve, demand for expert RCM services is expected to increase significantly.
Major Industry Segments
Within the healthcare revenue cycle management industry, key segments include hospitals, physician practices, and specialty clinics. Organizations can choose between outsourced RCM service models or maintaining in-house teams. Outsourcing is increasingly popular among smaller practices seeking efficiency, while larger health systems often leverage hybrid approaches. The choice depends on factors such as size, specialty, and available resources.
Competitive Landscape and Leading Players
Competition in the healthcare revenue cycle management industry is intense, with numerous established service providers offering tailored solutions. Top firms specialize in areas like hospital RCM, physician billing, or specialty clinic support. Recent trends include industry consolidation and strategic partnerships, enabling providers to offer broader expertise and innovative solutions to clients.
Case Example: RCM Transformation in a Multi-Specialty Clinic
A multi-specialty clinic partnered with a dedicated RCM service provider to streamline its billing and collections. By optimizing workflows and leveraging best practices, the clinic reduced days in accounts receivable and improved its net collection rate. This real-world example highlights how the healthcare revenue cycle management industry drives measurable financial and operational improvements for healthcare organizations.
The Revenue Cycle Management Process: Step-by-Step Breakdown
Understanding the revenue cycle is fundamental for any organization operating in the healthcare revenue cycle management industry. Each stage in the process is critical for maximizing revenue, minimizing denials, and ensuring regulatory compliance. Here is a step-by-step breakdown of the essential components of RCM, tailored for healthcare providers, clinics, and administrators.
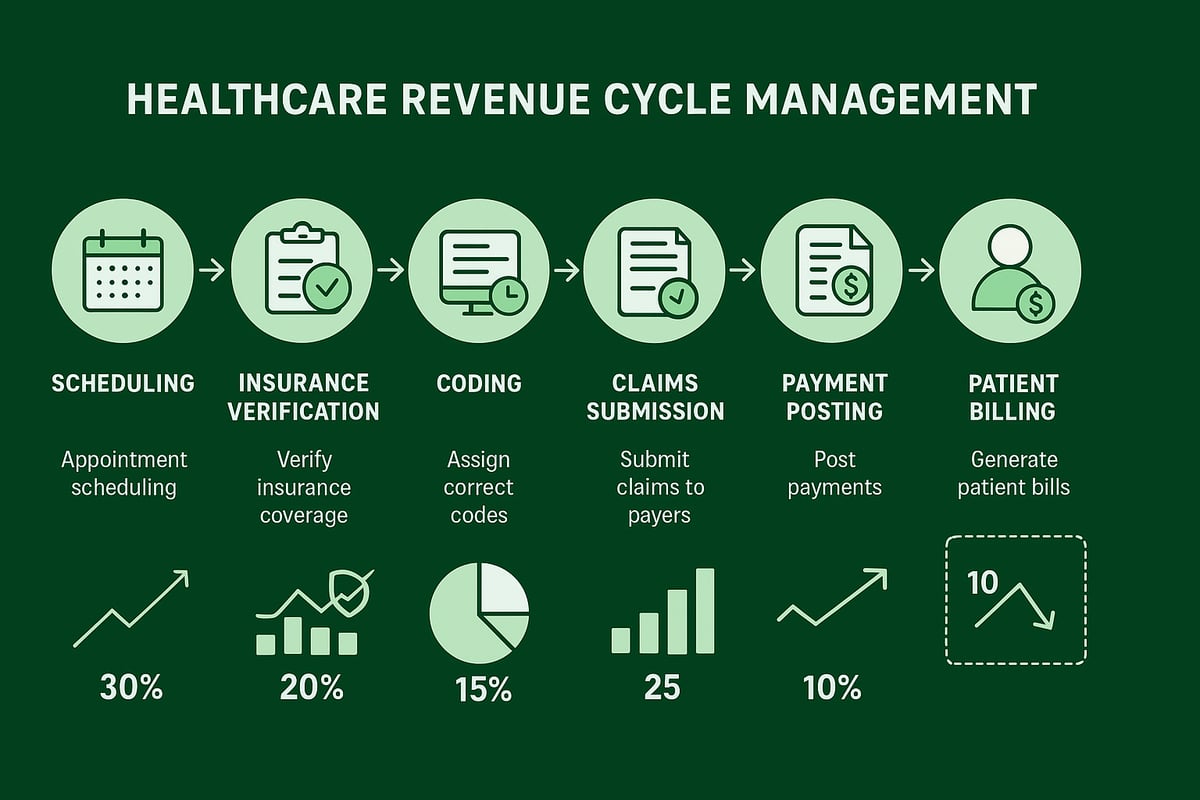
Step 1: Patient Scheduling and Pre-Registration
Accurate patient data collection is the foundation of the healthcare revenue cycle management industry process. During scheduling and pre-registration, front-desk staff gather demographic and insurance details to set up the patient account.
- Verify contact, insurance, and referral information.
- Collect required consents and authorizations.
- Input data directly into the billing system for seamless workflow.
Proper pre-registration reduces claim delays and errors, streamlining downstream revenue cycle tasks for all stakeholders.
Step 2: Insurance Verification and Prior Authorization
Verifying insurance eligibility and securing prior authorizations are vital steps in the healthcare revenue cycle management industry. These actions prevent claim rejections and ensure the provider receives payment for services rendered.
- Confirm benefits and coverage before the visit.
- Identify copays, deductibles, and out-of-pocket costs.
- Obtain authorization for high-value or specialty procedures.
Automated tools can speed up this process, but expert oversight is essential for accuracy, especially when payer policies frequently change.
Step 3: Medical Coding and Charge Capture
Certified medical coders translate clinical documentation into standardized codes for billing. In the healthcare revenue cycle management industry, accurate coding ensures correct reimbursement and compliance with payer rules.
- Assign CPT, ICD-10, and HCPCS codes.
- Capture all billable services and supplies.
- Audit for common coding errors that lead to denials.
A focus on documentation quality and coder education helps reduce costly mistakes and supports optimal revenue capture.
Step 4: Claims Submission and Processing
Timely and accurate claims submission drives cash flow for the healthcare revenue cycle management industry. Most organizations use electronic data interchange (EDI) to transmit claims to payers via clearinghouses.
- Submit claims promptly after charge capture.
- Address payer-specific requirements and edits.
- Track claim status and resolve rejections quickly.
Clearinghouses act as intermediaries, checking for formatting errors and routing claims to the correct insurance payers.
Step 5: Payment Posting and Reconciliation
After payers remit payments, the next task in the healthcare revenue cycle management industry is to post payments and reconcile accounts. This step ensures that all payments are correctly matched to the appropriate claims.
- Apply payments, adjustments, and write-offs.
- Identify and resolve payment discrepancies.
- Use automation to speed up reconciliation and reporting.
Efficient payment posting supports accurate financial reporting and helps identify underpayments or missed revenue opportunities.
Step 6: Denial Management and Appeals
Denials can significantly impact cash flow in the healthcare revenue cycle management industry. Proactive denial management includes root cause analysis and aggressive appeals when justified. For a deeper dive, explore Denial management strategies in billing.
- Categorize denials by type and frequency.
- Implement corrective actions to prevent future denials.
- Submit timely and well-documented appeals.
Successful denial management improves net collections and supports long-term financial health.
Step 7: Patient Billing and Collections
The final phase in the healthcare revenue cycle management industry process is patient billing and collections. Transparent communication and flexible payment options are key to maintaining strong patient relationships.
- Provide clear, itemized statements.
- Offer payment plans and digital payment portals.
- Follow up with reminders and support for financial questions.
Patient satisfaction rises when billing processes are straightforward and responsive to individual needs.
The Role of Technology and Outsourcing in Modern RCM
Technology is fundamentally reshaping the healthcare revenue cycle management industry. Providers are adopting advanced tools and outsourcing strategies to streamline operations, cut costs, and drive better financial outcomes. Below, we explore the major trends and best practices transforming RCM for healthcare organizations.
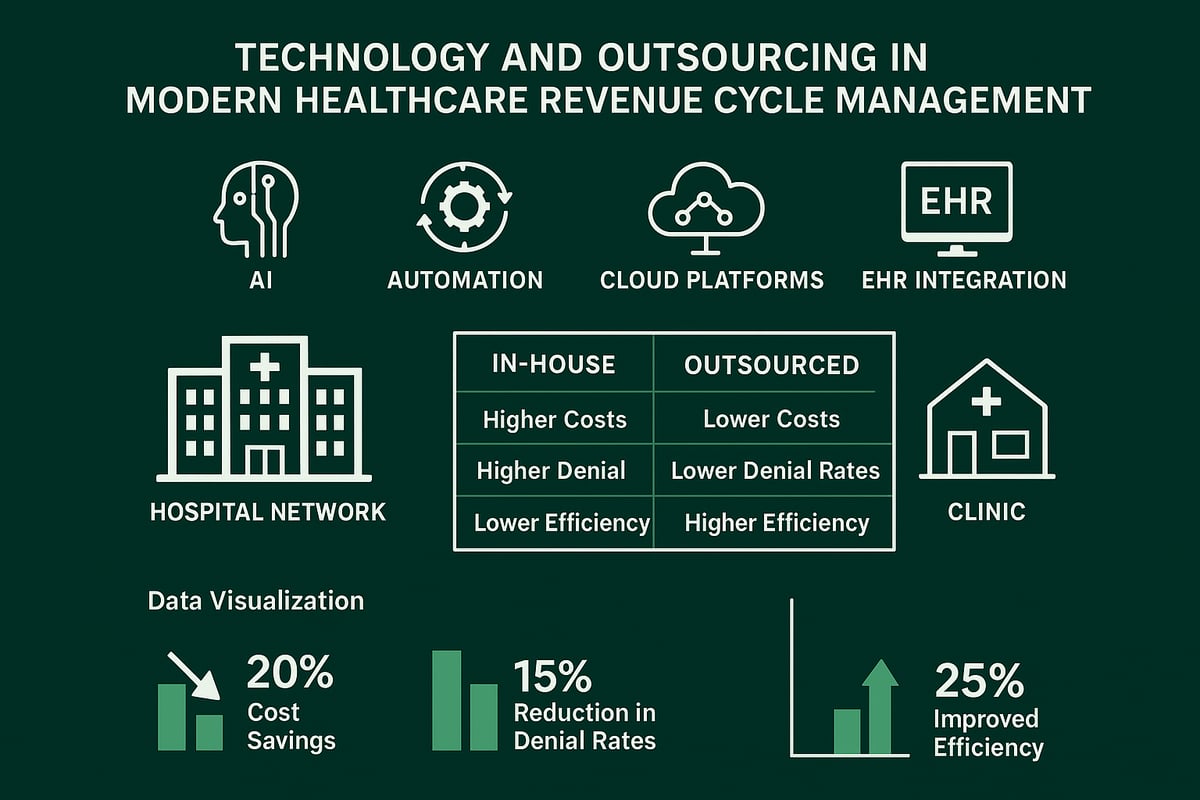
Impact of Automation and AI
Automation and artificial intelligence are revolutionizing the healthcare revenue cycle management industry. AI-powered tools now handle coding, claim scrubbing, and predictive analytics with greater accuracy and speed. These technologies reduce manual errors, lower administrative workload, and help providers prevent costly claim denials. For more details on how AI is transforming RCM, see this AI integration in RCM workflows report.
Organizations leveraging automation experience faster reimbursements and improved compliance. Implementing these solutions allows healthcare teams to focus on higher-value tasks, enhancing overall performance.
EHR Integration and Data Interoperability
Seamless integration between EHR systems and billing platforms is essential for the healthcare revenue cycle management industry. When clinical and financial data flow smoothly, providers benefit from fewer data entry errors and faster claims processing.
However, integrating multiple EHR platforms remains challenging, especially in organizations with varied specialties. Overcoming interoperability issues requires skilled professionals who can adapt RCM processes to diverse technology environments.
Outsourcing RCM Services: Benefits and Considerations
Outsourcing is a growing trend in the healthcare revenue cycle management industry. Many healthcare organizations choose external RCM partners to gain access to specialized expertise, reduce costs, and scale operations quickly.
Key advantages include:
- Cost savings and predictable expenses
- Improved collections and cash flow
- Access to skilled professionals
However, outsourcing also brings risks, such as concerns over data security, potential loss of direct control, and the need for robust vendor management strategies.
Greenhive Billing Solutions: Comprehensive RCM Services
Greenhive Billing Solutions offers tailored services to meet the complex needs of the healthcare revenue cycle management industry. Our team works with client-owned software and adapts to existing systems, ensuring seamless integration and minimal disruption.
We emphasize HIPAA compliance, specialty expertise, and transparent pricing. For example, a mid-size clinic saw a 20 percent reduction in collection times and measurable cost savings after transitioning to Greenhive’s services.
Cloud-Based RCM Platforms
Cloud-based platforms are increasingly popular in the healthcare revenue cycle management industry. They offer real-time access to data, streamlined updates, and significantly reduced IT maintenance.
Both small practices and large hospital networks are adopting cloud solutions for their flexibility and scalability. These platforms make it easier to manage billing remotely and respond quickly to regulatory changes.
Case Example: Successful RCM Automation in a Hospital Network
A large hospital network implemented automation in key RCM functions, resulting in a 30 percent improvement in days in accounts receivable and a substantial drop in claim denial rates.
This transformation demonstrates how technology and outsourcing can drive measurable results, making them essential strategies in the evolving healthcare revenue cycle management industry.
Regulatory Compliance and Security in RCM
Maintaining regulatory compliance and ensuring data security are nonnegotiable in the healthcare revenue cycle management industry. Every organization must adopt a proactive approach to protect patient information, meet payer requirements, and stay ahead of regulatory changes. Failing to do so can result in costly penalties, reputational harm, and business disruption.
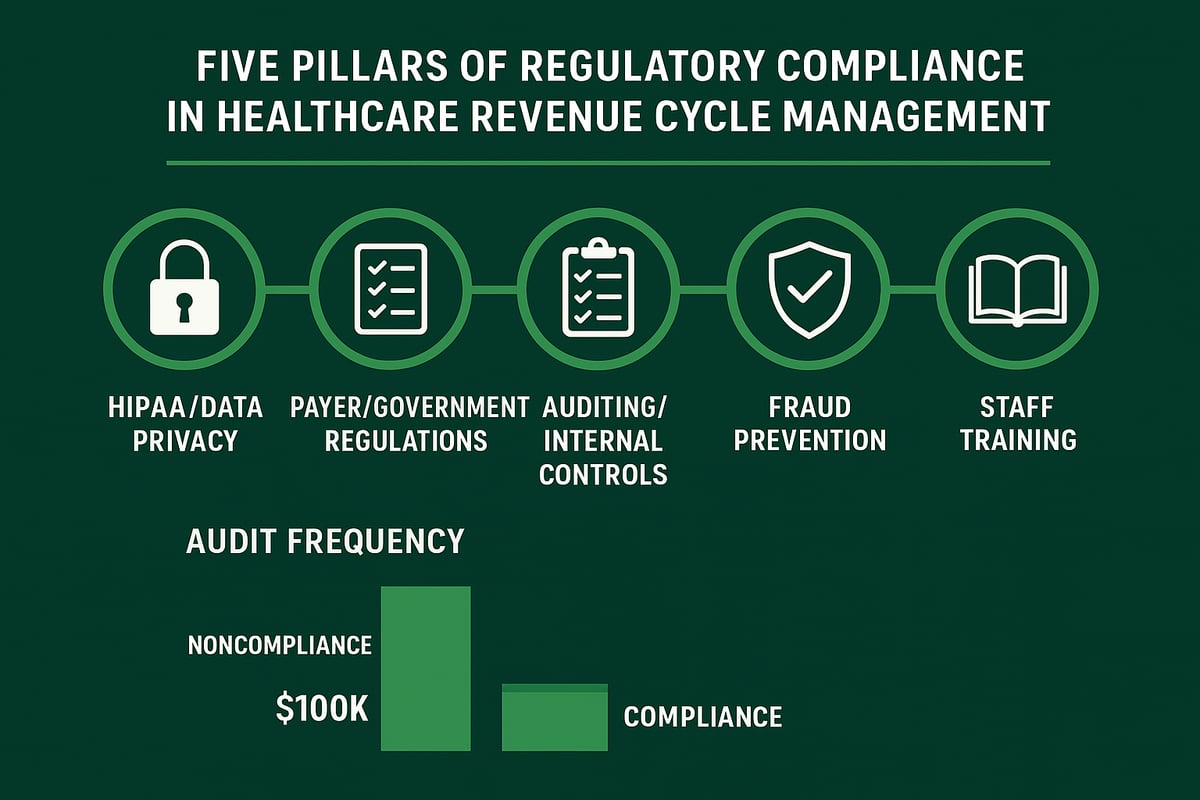
HIPAA and Data Privacy Requirements
The healthcare revenue cycle management industry is strictly governed by HIPAA, which mandates robust protection of patient health information throughout all billing and collection activities. Organizations must implement encryption, access controls, and secure communication protocols to prevent unauthorized data exposure.
Regular risk assessments and staff training are essential for compliance. In this industry, even minor data breaches can result in severe penalties, making privacy a top priority.
Payer and Government Regulations
Beyond HIPAA, the healthcare revenue cycle management industry must navigate a complex landscape of payer rules and government programs. CMS regulations, MACRA, and MIPS all affect billing procedures and documentation standards.
State-specific requirements add additional layers of complexity. Staying current with these evolving standards is crucial for accurate claims submission and timely reimbursement in this highly regulated industry.
Auditing and Internal Controls
Routine audits are critical in the healthcare revenue cycle management industry to identify compliance gaps and ensure proper billing practices. Internal controls, such as segregation of duties and automated reporting, help reduce risk.
Leveraging tools like healthcare revenue cycle analytics enables organizations to monitor compliance metrics in real time, streamline audit processes, and quickly address discrepancies.
Preventing Fraud and Abuse
Fraud and abuse in RCM can take many forms. Common schemes include upcoding, unbundling, and phantom billing. These practices can trigger audits and legal action.
| Fraud Scheme | Description | Prevention Strategy |
|---|---|---|
| Upcoding | Billing for higher value | Regular coding audits |
| Phantom Billing | Charging for no service | Verification of services |
| Unbundling | Separating bundled codes | Use of coding guidelines |
Proactive detection and staff vigilance are essential to protect your organization.
Staff Training and Certification
Ongoing staff education is vital for compliance in the healthcare revenue cycle management industry. Regulatory guidelines change frequently, so front-line teams must stay updated.
Certification programs and regular workshops reinforce best practices and build a culture of accountability. Investing in staff training ensures your organization meets industry standards and reduces the risk of costly errors.
Best Practices for Optimizing Revenue Cycle Performance
Optimizing performance in the healthcare revenue cycle management industry is essential for financial health and operational efficiency. By implementing targeted best practices, organizations can streamline workflows, reduce errors, and maximize collections. Below, we explore core strategies every healthcare provider should adopt to maintain a robust revenue cycle.
Key Performance Indicators (KPIs) to Track
Success in the healthcare revenue cycle management industry starts with tracking the right KPIs. Focus on metrics like days in accounts receivable (A/R), clean claim rate, denial rate, and net collection rate. These indicators reveal bottlenecks and highlight areas for improvement.
- Days in A/R: Measures how quickly payments are collected.
- Clean claim rate: Percentage of claims processed without errors.
- Denial rate: Portion of claims rejected by payers.
- Net collection rate: Percentage of total payments collected.
Benchmark your organization’s performance against industry standards to identify gaps. Regular KPI monitoring enables timely interventions and supports sustainable financial health.
Process Standardization and Workflow Automation
Establishing standardized processes is vital for consistency in the healthcare revenue cycle management industry. Develop detailed standard operating procedures (SOPs) for every billing step, from patient registration to payment posting. Consistent processes reduce errors and minimize revenue leakage.
Adopt workflow automation to handle repetitive tasks, such as claim submission or eligibility verification. Automation not only accelerates turnaround but also frees staff to focus on resolving exceptions and improving patient experience. This approach supports scalability as your organization grows.
Patient Engagement and Financial Transparency
Transparent financial communication is now a cornerstone of the healthcare revenue cycle management industry. Offer pre-service cost estimates and clear billing statements to build trust and minimize confusion. Encourage patients to use digital payment options for quicker transactions.
Effective engagement increases patient satisfaction and collection rates. Use patient portals, SMS reminders, and online payment platforms to make the billing process accessible and user-friendly. When patients understand their financial responsibilities, payment delays and disputes decrease.
Staff Training and Cross-Department Collaboration
Continuous staff development is essential for success in the healthcare revenue cycle management industry. Provide regular training for front office, billing, and clinical teams to keep everyone updated on regulatory changes and payer requirements.
Promote collaboration between departments to resolve billing issues quickly. Establish clear communication channels and hold cross-functional meetings. When teams work together, errors decrease and claims move smoothly through the revenue cycle.
Continuous Improvement and Analytics
Data-driven decision-making ensures ongoing improvement in the healthcare revenue cycle management industry. Leverage analytics to identify trends, monitor KPIs, and pinpoint process inefficiencies. Regularly review denial reasons and root causes to implement corrective actions.
For a comprehensive overview of proven optimization strategies, review best practices for healthcare RCM. Embracing analytics fosters a culture of accountability and adaptability, improving both financial and operational outcomes.
Outsourcing vs. In-House: Making the Right Choice
Deciding between in-house and outsourced solutions is a critical consideration in the healthcare revenue cycle management industry. Evaluate your organization’s size, specialty, available resources, and long-term goals. Outsourcing can offer access to specialized expertise and advanced technology, while in-house teams provide direct control.
Use a comparative approach to weigh costs, scalability, and compliance needs. Many physician practices benefit from tailored solutions, such as those described in physician revenue cycle management, to achieve optimal results. The right choice aligns with your strategic priorities and supports sustainable growth.
Future Outlook: Trends and Predictions in Healthcare RCM
The healthcare revenue cycle management industry is entering a transformative period marked by rapid change and new opportunities. B2B providers must stay proactive to succeed in a landscape shaped by value-based care, expanding telehealth, advanced analytics, evolving regulations, and ongoing consolidation. These trends are redefining how organizations optimize revenue cycles and deliver sustainable financial performance.
Value-Based Care and Alternative Payment Models
The healthcare revenue cycle management industry continues to shift from fee-for-service models to value-based reimbursement. Providers are adapting RCM workflows to support bundled payments, shared savings, and quality-focused incentives. These models require precise tracking of patient outcomes and alignment between clinical and financial operations.
B2B RCM service providers are helping clients navigate bundled payment contracts and implement new strategies for risk-sharing arrangements. The shift encourages collaboration between payers and providers to achieve better results for patients and organizations.
Expansion of Telehealth and Remote Services
Telehealth adoption is accelerating, bringing unique billing and compliance challenges to the healthcare revenue cycle management industry. Virtual care introduces new codes, payer policies, and requirements for accurate documentation. Providers must stay informed about changing reimbursement rules for remote visits.
Technology integration is essential for seamless telehealth billing. RCM partners are supporting clinics and practices in adapting systems, verifying insurance, and ensuring timely payment for remote services.
Advanced Analytics and Predictive Modeling
Advanced analytics are revolutionizing the healthcare revenue cycle management industry by enabling data-driven decision-making. Predictive modeling helps forecast denials, identify at-risk claims, and optimize collections. Industry leaders are leveraging real-time dashboards and AI to monitor trends, reduce errors, and improve cash flow.
The Global RCM market projected to reach $894.25 billion by 2033 highlights how analytics and automation are fueling industry growth and driving innovation in revenue cycle processes.
Evolving Regulatory Landscape
Regulatory requirements for the healthcare revenue cycle management industry continue to evolve. Federal and state agencies are introducing new billing standards, privacy rules, and reporting obligations. Providers must prepare for ongoing compliance updates and increased scrutiny.
Staying current with regulations is critical. RCM partners offer guidance, training, and audit support to help organizations mitigate risk and maintain compliance in a dynamic environment.
Industry Consolidation and Strategic Partnerships
Consolidation is reshaping the healthcare revenue cycle management industry. Mergers, acquisitions, and strategic alliances are creating larger, more integrated RCM service networks. These partnerships enable providers to access broader expertise, advanced technology, and scalable solutions.
Collaborative efforts are expected to drive innovation and deliver measurable improvements in revenue cycle performance for B2B clients.
As you’ve seen throughout this guide, staying ahead in healthcare revenue cycle management means navigating evolving regulations, leveraging technology, and continuously optimizing every step of the process. We all know how challenging it can be to spot hidden inefficiencies or compliance gaps, especially as the industry transforms. If you’re wondering where your practice stands or how you can boost financial performance, why not take the next step? You can gain valuable insights and practical recommendations tailored to your needs—simply Get Your Free Audit. It’s a smart way to move forward with confidence.