The landscape of healthcare billing is changing rapidly, and the need to verify medical insurance is more crucial than ever for providers planning ahead for 2026. New payer requirements, evolving technology, and stricter compliance standards are reshaping daily operations for clinics and healthcare organizations.
This expert guide equips your team with actionable strategies and up-to-date insights to master every step of the verification process. You will discover the critical importance of precise insurance checks, learn efficient workflows, stay ahead of technology trends, and ensure compliance while maximizing reimbursements.
Ready to streamline your revenue cycle and stay ahead of industry changes? Dive in for expert guidance tailored to healthcare professionals and organizations.
The Critical Role of Insurance Verification in 2026
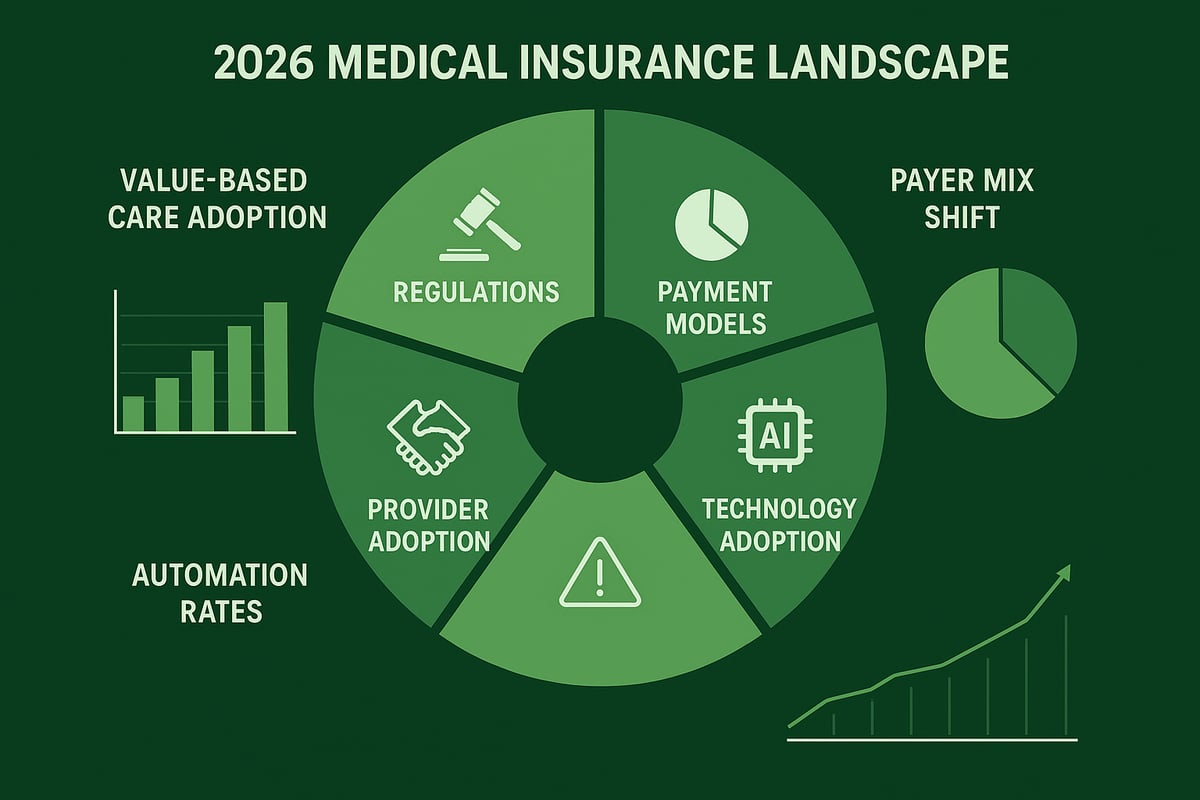
The ability to accurately verify medical insurance is more vital than ever in 2026. Healthcare providers face a rapidly shifting landscape, where payer requirements, compliance standards, technology, and patient expectations are all evolving. Understanding the critical role of verification is key to protecting revenue, managing risk, and ensuring operational excellence.
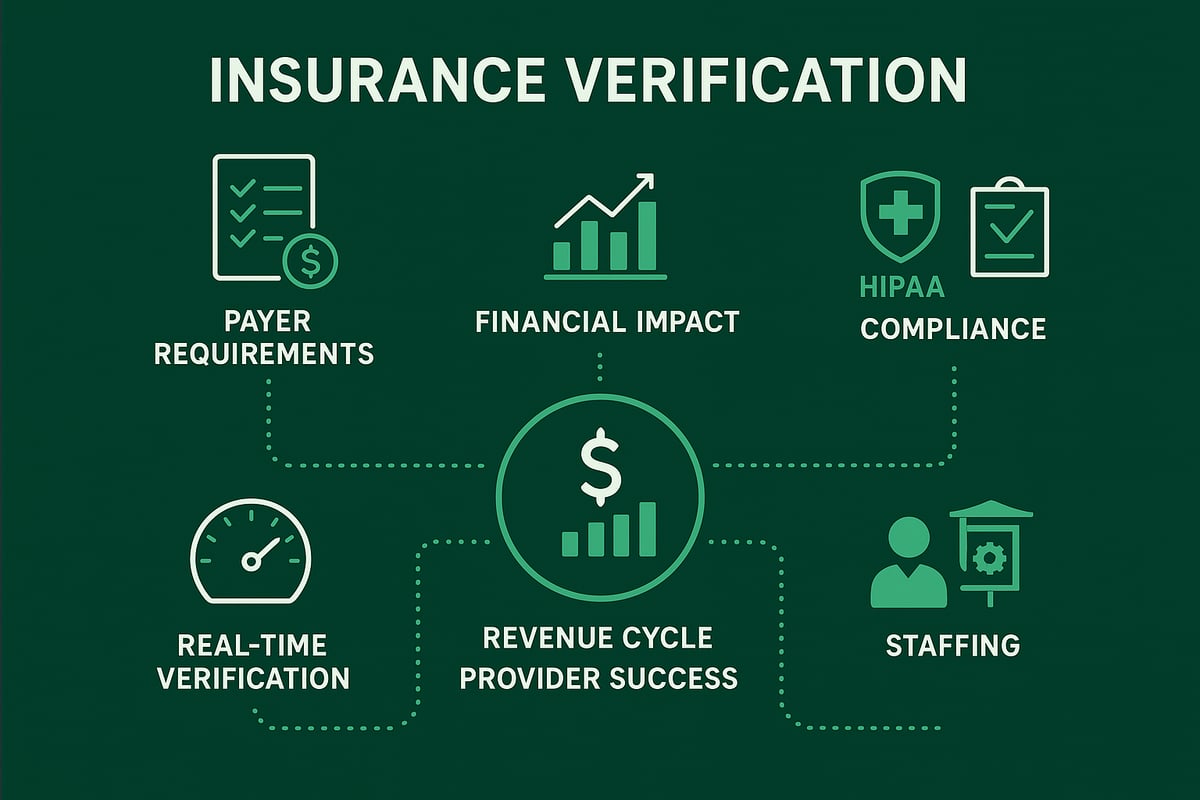
The Impact of Evolving Payer Requirements
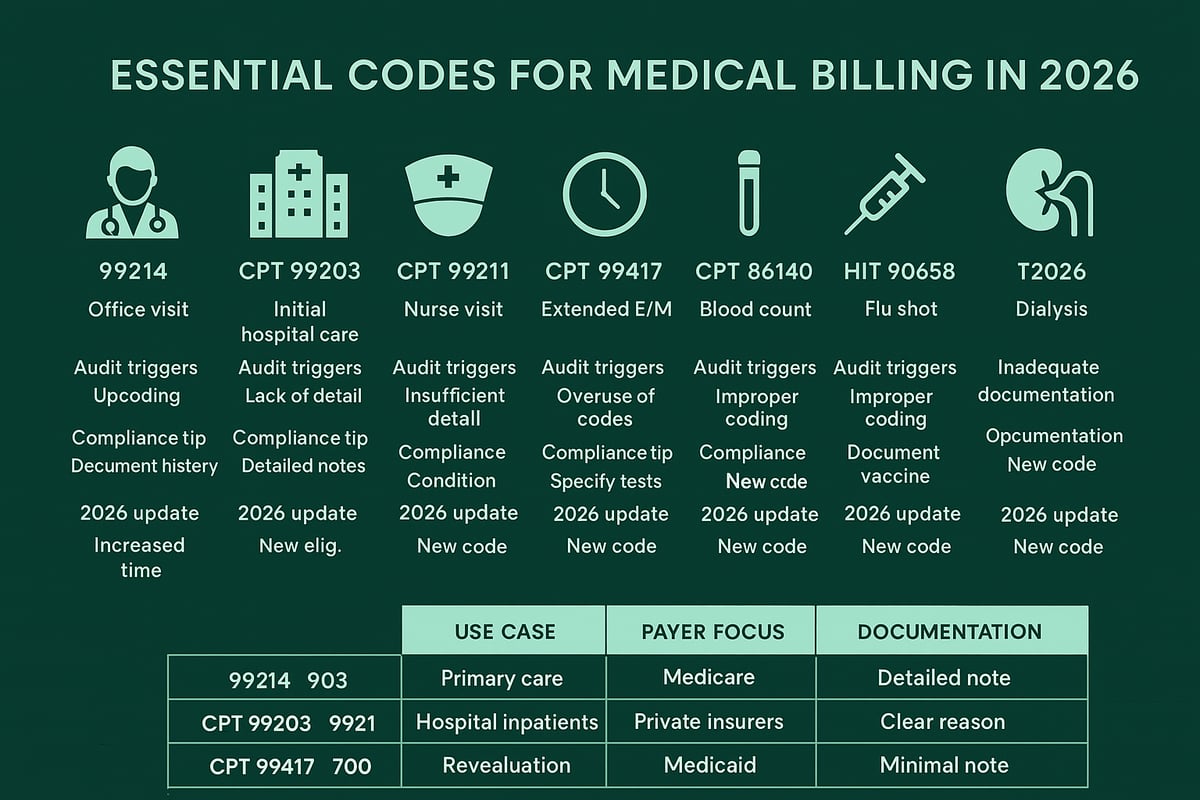
Payer policies are shifting in 2026, requiring providers to adapt quickly. Insurers are introducing new benefit structures, more granular eligibility rules, and stricter documentation standards. For example, some plans now require multi-tiered authorizations or dynamic copay calculations based on procedure codes.
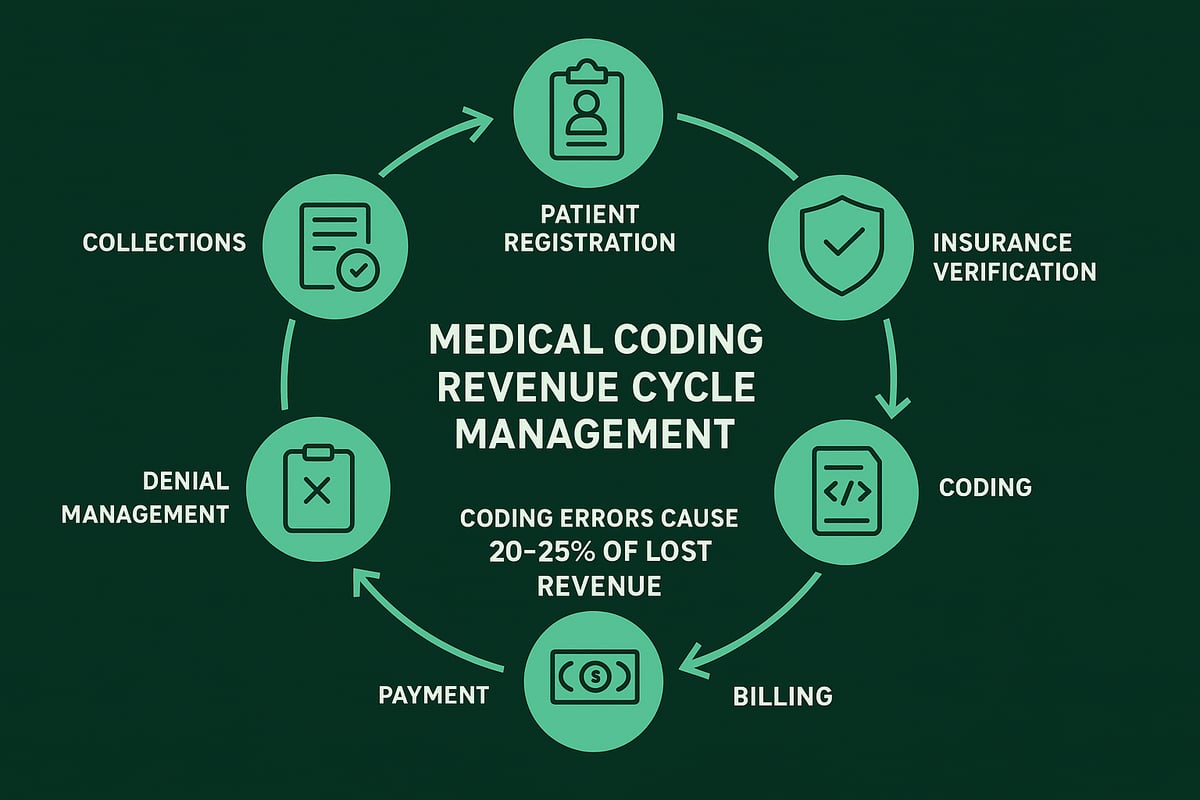
A 2024 industry survey revealed that over 60% of claim denials stem from eligibility errors. To effectively verify medical insurance, healthcare organizations must stay current with changing payer bulletins and leverage robust verification protocols. Missing a small detail can cascade into major revenue disruption.
Financial and Operational Implications
Incomplete or inaccurate attempts to verify medical insurance can result in significant lost revenue. Denials due to eligibility issues not only delay payments but also increase the administrative workload and reduce patient satisfaction.
| Impact Area | Consequence | Example |
|---|---|---|
| Revenue Loss | Unpaid or delayed claims | $500K annual loss reported |
| Cash Flow | Increased AR days | 30% slower collections |
| Admin Burden | Rework and appeals | 2x staff time per denial |
A multi-specialty group recently faced a 15% drop in collections due to verification gaps. For additional insights into how proper verification reduces denials, see Denial Management in Medical Billing. The bottom line: every step to verify medical insurance directly affects your financial health.
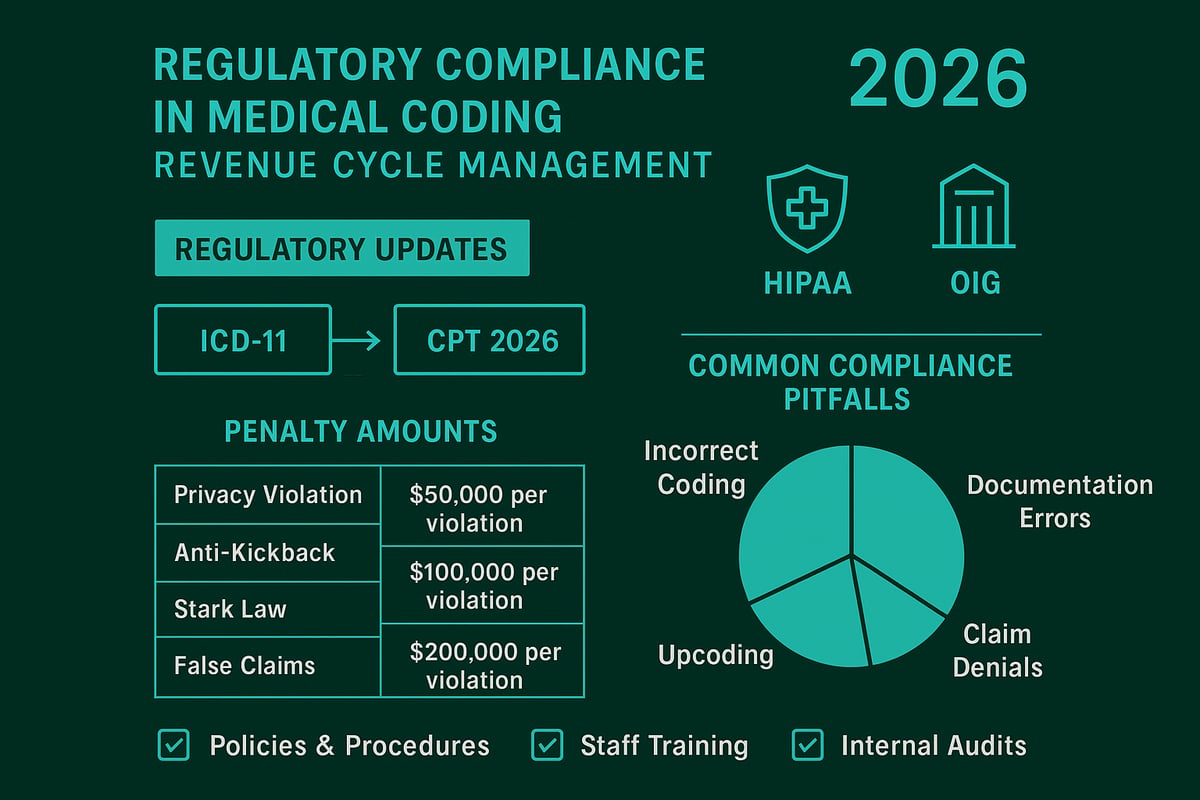
Regulatory and Compliance Considerations
Regulatory demands are increasing, with HIPAA updates and new payer mandates governing how providers verify medical insurance. In 2026, documentation standards are more stringent, requiring detailed audit trails for every verification.
Non-compliance can result in penalties, and payer audits are more frequent. Providers must ensure that their verification processes meet the latest requirements to avoid fines and reputational damage. Documentation is now a frontline defense in regulatory audits.
The Shift Toward Real-Time Verification
Real-time eligibility checks have become the industry benchmark in 2026. These tools offer immediate confirmation of coverage, reducing wait times and minimizing errors when you verify medical insurance.
Average turnaround times have dropped to under two minutes for most payers. Real-time verification not only improves efficiency but also helps staff resolve discrepancies before the patient encounter, strengthening the revenue cycle.
Patient Experience and Practice Reputation
Verification errors can erode patient trust and damage a provider’s reputation. Patients who receive unexpected bills or encounter coverage confusion are more likely to leave negative online reviews and seek care elsewhere.
Proactively verify medical insurance and communicate coverage details clearly to patients. This approach enhances satisfaction, supports retention, and builds a positive brand image for your organization.
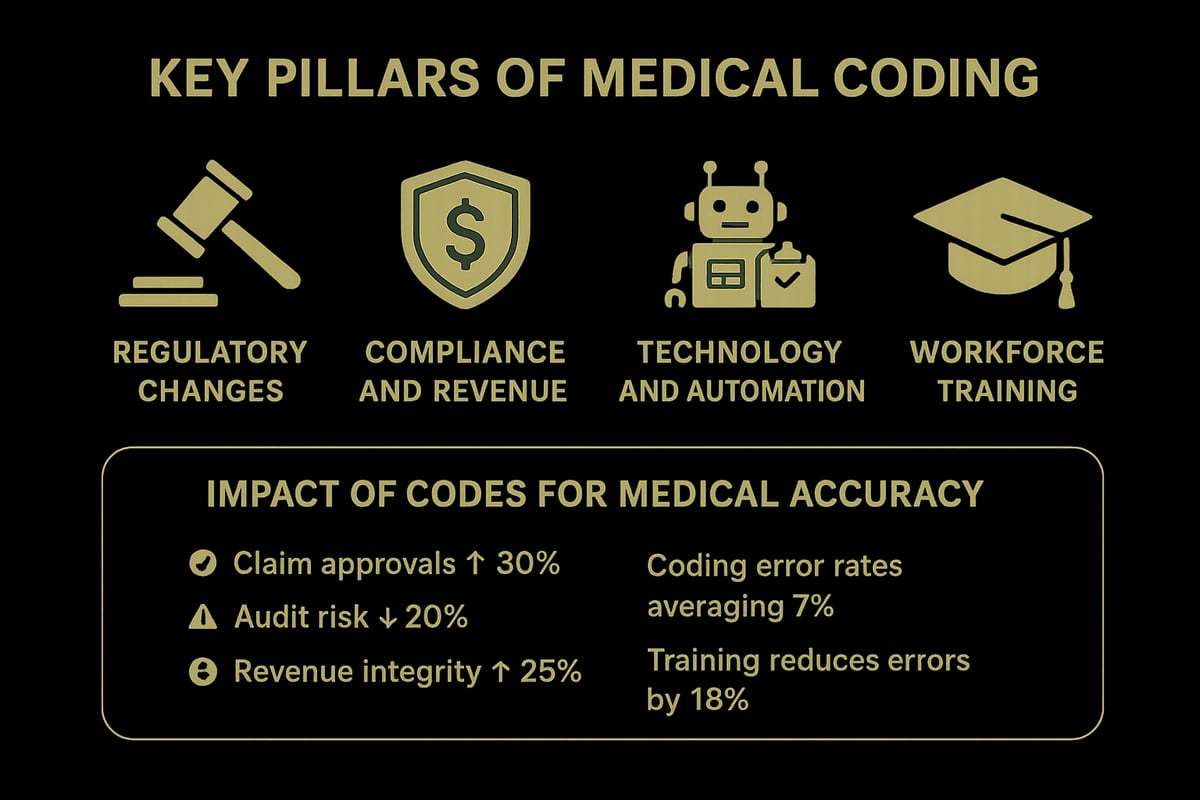
Staffing and Training Challenges
The complexity of insurance verification in 2026 requires specialized training. Staff must understand new protocols, navigate payer portals, and handle exceptions efficiently.
High turnover can jeopardize verification accuracy. Investing in ongoing training and clear workflows ensures your team is equipped to verify medical insurance correctly, supporting both compliance and financial objectives.
Step-by-Step Process to Verify Medical Insurance in 2026
Navigating the process to verify medical insurance in 2026 requires precision, up-to-date knowledge, and a systematic approach. Healthcare organizations must implement robust workflows to minimize denials and optimize reimbursements. Below, we break down each essential step for B2B healthcare teams.
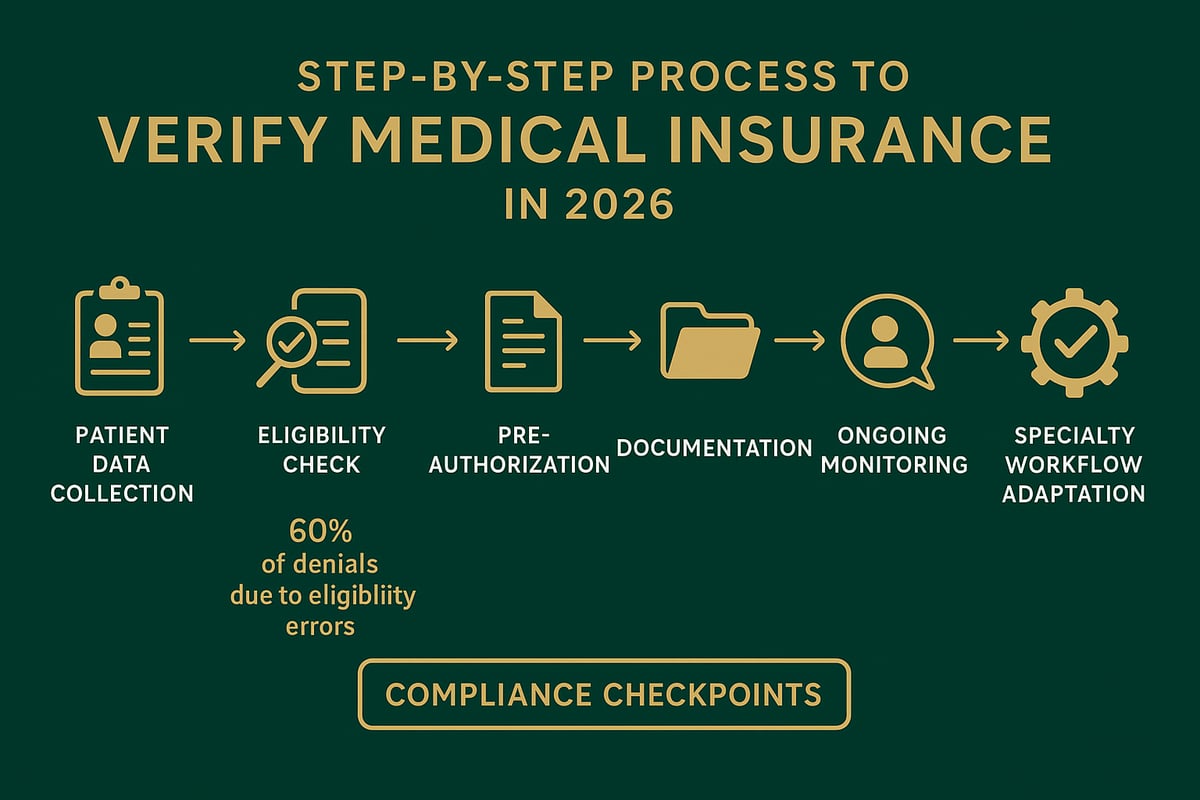
Step 1: Collect and Validate Patient Information
The foundation to verify medical insurance begins with accurate patient data collection. Ensure front desk or intake teams gather complete demographic details and insurance information at every encounter. Double-check data such as name, date of birth, policy number, and payer group.
Common data entry errors can derail the process. These include transposed digits, misspelled names, or outdated coverage details. To reduce mistakes, implement digital forms with validation fields and train staff on common pitfalls.
| Common Data Entry Errors | Prevention Strategy |
|---|---|
| Wrong policy number | Use real-time validation |
| Misspelled patient name | Cross-check with ID |
| Expired insurance card | Request updated copy |
Accuracy at this stage ensures downstream steps to verify medical insurance are efficient and compliant.
Step 2: Check Eligibility and Benefits
Next, verify medical insurance eligibility and benefit details directly with payers. Use payer portals, clearinghouses, or professional RCM services for real-time checks. Confirm coverage dates, co-pay amounts, deductibles, and any plan exclusions.
Missing benefit limitations can result in costly denied claims. For example, a recurring therapy visit might be denied if annual visit limits are exceeded. Always document eligibility responses and clarify any ambiguous coverage terms with the payer before service is rendered.
A standardized checklist helps ensure all critical data points are reviewed during each attempt to verify medical insurance.
Step 3: Confirm Pre-Authorizations and Referrals
In 2026, more services require payer pre-authorization or referrals before treatment. Identify which procedures need authorization by reviewing payer bulletins and plan documents. Submit requests early and track responses to avoid delays.
Document authorization numbers, approval dates, and expiration periods. Missing or expired authorizations are a leading cause of denied claims. For a deeper dive into this process, consult the Authorization in Medical Billing Guide for step-by-step instructions and best practices.
Mastering this step strengthens your ability to verify medical insurance efficiently and reduces costly interruptions in patient care.
Step 4: Document Verification Results
Documenting each verification step is crucial for audit-readiness and operational transparency. Record eligibility confirmation, pre-authorization details, and any additional payer communications in the patient's electronic health record or practice management system.
Standardized documentation protocols ensure consistency, especially when multiple staff members are involved. This approach supports compliance and simplifies payer audits. Integrate digital documentation tools to streamline the process and ensure all steps to verify medical insurance are traceable.
Step 5: Communicate with Patients and Internal Teams
Timely, clear communication is key when you verify medical insurance. Notify patients as soon as coverage issues or benefit limits are identified. Use phone calls, secure messaging, or patient portals to provide updates and clarify financial responsibility.
Internally, establish workflows to flag discrepancies before appointments. Collaboration between front office, billing, and clinical teams prevents last-minute surprises and supports a seamless patient experience. Each time you verify medical insurance, make sure communication protocols are followed.
Step 6: Ongoing Monitoring and Updates
Insurance plans and patient circumstances change frequently. To maintain accuracy, routinely verify medical insurance for recurring care or high-risk patients. Set automated reminders to recheck eligibility at appropriate intervals, such as every visit or before scheduled procedures.
Industry benchmarks suggest re-verification is essential for chronic care management, infusion therapies, or behavioral health. Consistent monitoring reduces the risk of denied claims and keeps your revenue cycle healthy.
Example Workflow for Specialty Practices
Specialty and high-volume clinics may need tailored steps to verify medical insurance. For example, laboratory services often require rapid eligibility checks and payer-specific documentation. Behavioral health providers must navigate unique benefit structures and frequent prior authorization rules.
Customizing workflows for specialty needs improves efficiency and reduces errors. Continuous staff training and periodic workflow reviews help specialty practices maintain best-in-class verification outcomes.
Leveraging Technology and Outsourcing for Efficient Verification
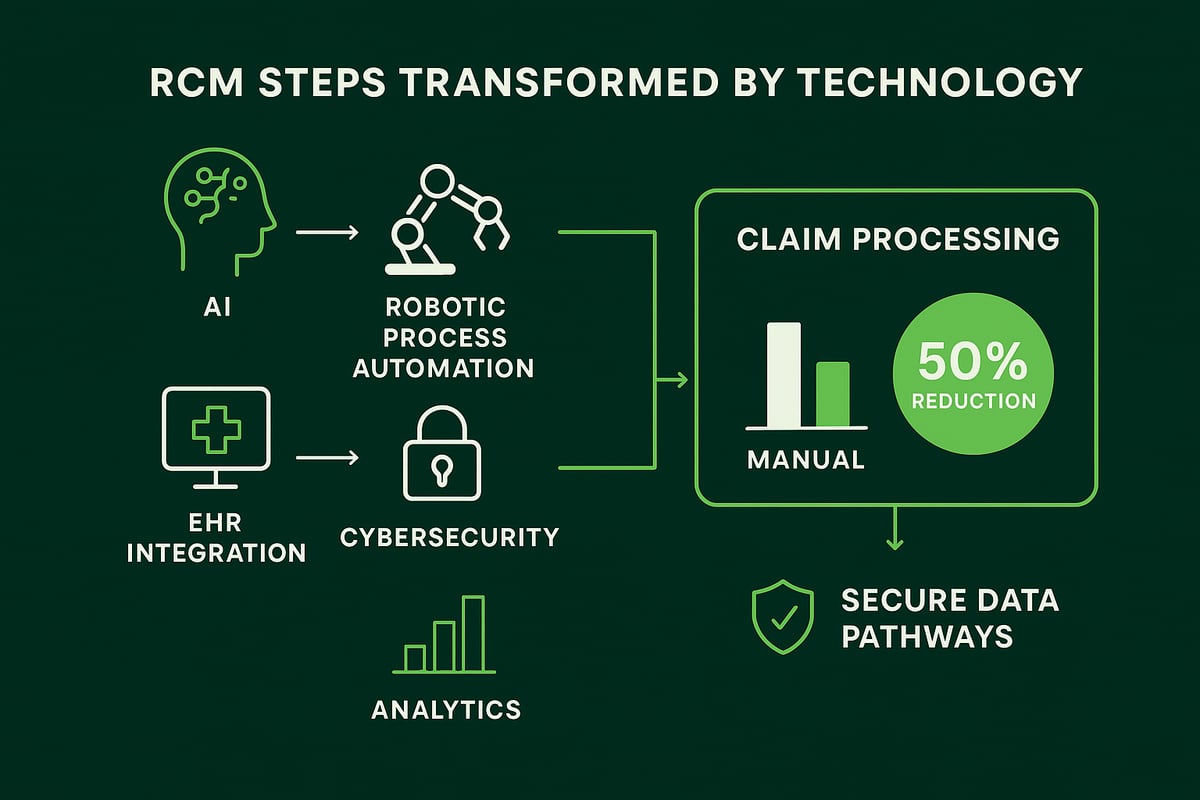
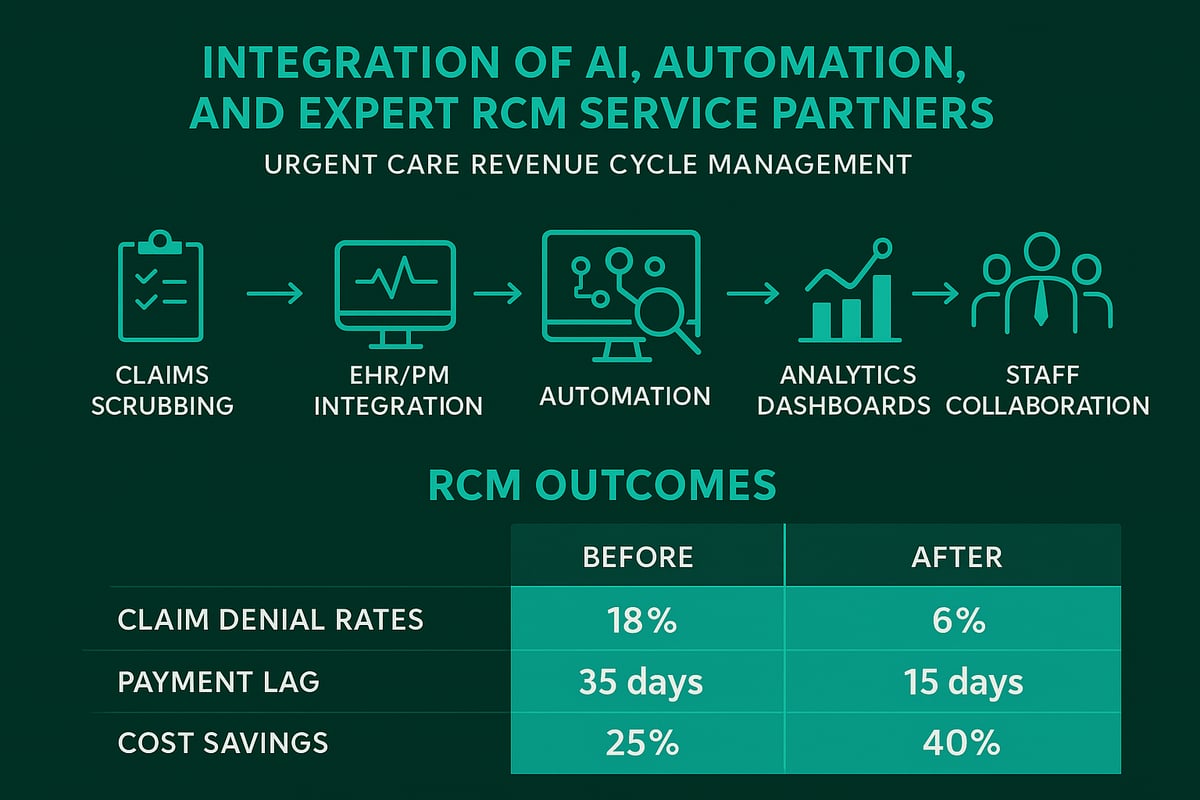
Technological advancements have transformed how healthcare organizations verify medical insurance. In 2026, automation, AI, and specialized outsourcing are crucial for streamlining verification processes, minimizing errors, and driving revenue cycle performance.
Automation and AI in Insurance Verification
To verify medical insurance efficiently in 2026, automation and AI-driven tools are now industry standards. These technologies instantly extract and validate eligibility data from multiple payer sources, reducing manual effort and mistakes.
AI systems can flag inconsistencies, predict claim risks, and even auto-populate verification forms. Practices using AI report faster turnaround, higher accuracy, and fewer denied claims. A recent survey found that over 70% of U.S. providers now use some form of automation to verify medical insurance, demonstrating the shift toward tech-enabled workflows.
Automation lets your team focus on complex cases rather than repetitive data entry. As payer rules grow more intricate, AI’s ability to adapt quickly is a major advantage.
Integration with EHR and Practice Management Systems
Seamless integration between verification tools and your EHR or practice management system is essential. When you verify medical insurance, results must sync automatically with patient records to avoid errors and ensure audit readiness.
However, integration brings challenges. Compatibility issues, data mapping, and user training can create hurdles. Practices should vet solutions for interoperability and data security before implementation.
Best practices include standardized data fields, regular system updates, and close collaboration between IT and billing teams. This approach keeps verification workflows smooth and reduces rework.
Outsourcing Verification: When and Why
Many organizations choose to outsource insurance verification to specialized RCM partners. Outsourcing is particularly valuable for high-volume clinics, multi-location groups, or practices with frequent staff turnover.
Compare in-house and outsourced verification:
| Factor | In-House | Outsourced RCM Partner |
|---|---|---|
| Staffing | Requires training | Experienced verification team |
| Cost | Fixed payroll | Scalable, per-transaction |
| Accuracy | Varies by staff | Industry benchmarks |
| Turnaround Time | Dependent on volume | Faster, 24/7 coverage |
Outsourcing helps verify medical insurance consistently while freeing up internal resources for patient care. Case studies show clinics reducing denials and increasing collections by partnering with experts.
Greenhive Billing Solutions: Expert Insurance Verification Services
Greenhive delivers end-to-end insurance eligibility verification services for healthcare providers. Our professionals verify medical insurance using your existing software and adapt to all payer requirements, ensuring a smooth fit with your current systems.
Clients benefit from improved claim approval rates, fewer administrative delays, and tailored support from our team. By leveraging Greenhive’s expertise, practices experience measurable gains in cash flow and compliance, with less time spent on manual verification.
For organizations seeking a seamless and scalable solution, Greenhive’s approach blends advanced tools with human expertise to verify medical insurance accurately, every time.
Data Security and Compliance in Tech-Enabled Verification
Data security and HIPAA compliance are foundational when you verify medical insurance using technology or outsourcing. Digital workflows must protect PHI at every step.
Best practices include encryption, role-based access, and regular audits of both software and service providers. Always verify that partners meet regulatory standards and provide clear documentation trails.
By prioritizing security and compliance, healthcare organizations can confidently adopt tech-enabled solutions for insurance verification—reducing risk while enhancing efficiency.
Navigating Complex Insurance Scenarios in 2026
Navigating the complexities involved when you verify medical insurance in 2026 requires deep industry knowledge, adaptable workflows, and expert resources. Healthcare providers face a rapidly changing landscape with new plan types, stricter documentation, and sophisticated payer requirements. Mastering these challenges is essential for accurate reimbursement and sustained practice growth.
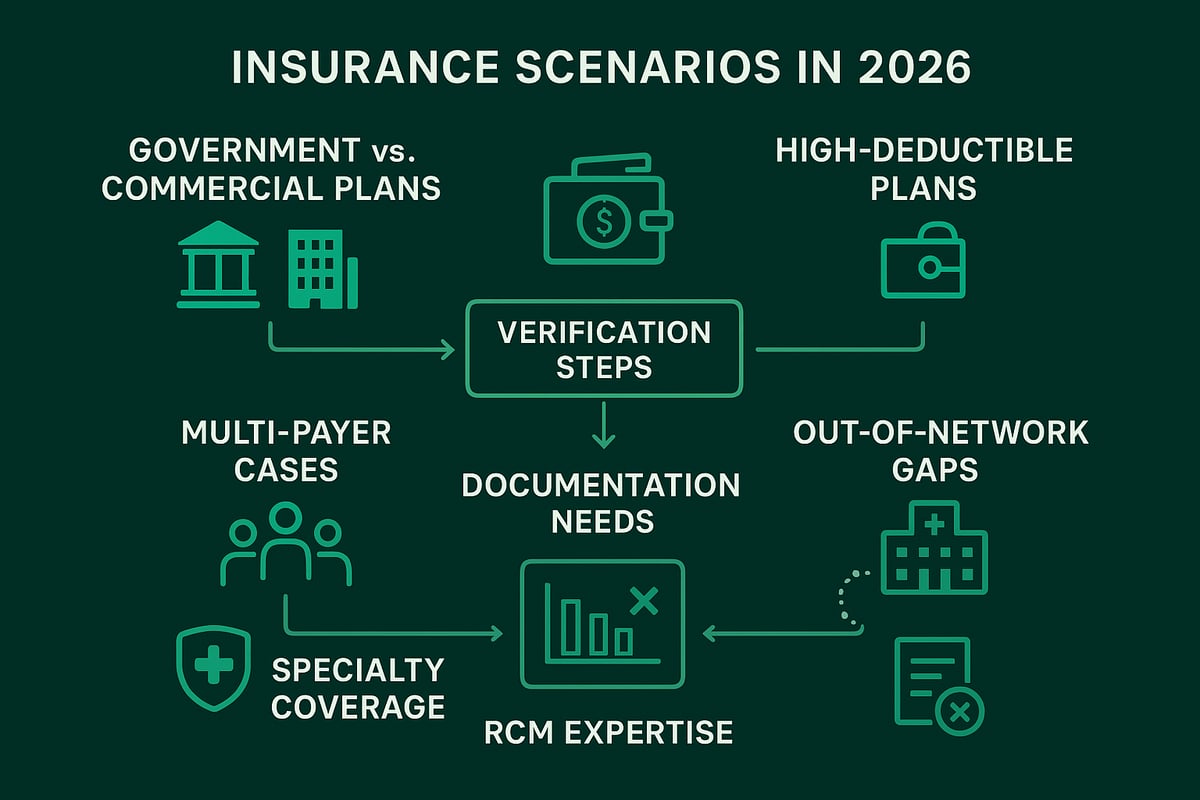
Verifying Government vs. Commercial Plans
To verify medical insurance when dealing with government plans like Medicare or Medicaid, providers must account for unique eligibility requirements and frequent regulatory updates. Commercial insurers, in contrast, often have additional documentation layers and variable network rules.
Dual-eligible patients, who qualify for both Medicare and Medicaid, present extra verification hurdles. Practices must confirm primary and secondary coverage, ensure benefits coordination, and monitor state-specific Medicaid rules. Missing a detail can result in claim denials or payment delays, so diligence is critical.
Handling High-Deductible and Marketplace Plans
High-deductible health plans and marketplace coverage have surged in popularity, adding new complexity when you verify medical insurance. These plans often shift more financial responsibility to patients, requiring practices to check deductible status and out-of-pocket maximums for every encounter.
Verifiers must clarify patient financial responsibility upfront, communicate coverage limitations, and flag services that may not be covered until deductibles are met. This proactive approach helps prevent billing confusion and maintains patient trust in your organization.
Specialty and Ancillary Coverage Verification
When you verify medical insurance for specialty services—such as laboratory, behavioral health, or physical therapy—payers may require additional pre-authorizations or impose unique benefit restrictions. Each specialty comes with its own documentation standards and payer-specific rules.
Successful verification depends on staying current with these requirements, maintaining detailed records, and following up with payers for confirmation. Failing to address specialty nuances can lead to denials and lost revenue, especially in high-volume practices.
Multi-Payer and COB (Coordination of Benefits) Cases
Multi-payer situations are increasingly common, especially as patients hold multiple insurance policies. To verify medical insurance in these cases, practices must determine which plan is primary and which is secondary, then follow each payer's coordination of benefits rules.
Common pitfalls include incorrect sequencing, missing COB documentation, or failing to update coverage changes. Establishing clear internal workflows and training staff to handle COB scenarios can reduce errors and support timely reimbursement for all services rendered.
Out-of-Network and Prior Coverage Gaps
Verifying coverage for out-of-network services requires additional attention to payer rules, prior authorization requirements, and patient notification. Practices must also check for any lapses or gaps in insurance history that could impact eligibility.
Proactively identifying and addressing these issues can help avoid surprise billing and ensure transparency for patients. Consistent communication with both payers and patients is essential to minimize disputes and protect your organization's reputation.
Leveraging RCM Expertise for Complex Cases
Complex scenarios demand more than just basic eligibility checks. When you partner with experienced RCM professionals, you gain access to specialized knowledge and proven processes to verify medical insurance across all plan types and situations.
RCM teams can adapt to your existing systems, manage intricate verifications, and ensure compliance with the latest payer and regulatory requirements. For organizations seeking to streamline their workflow, Insurance Eligibility Verification Services offer comprehensive support for even the most challenging cases.
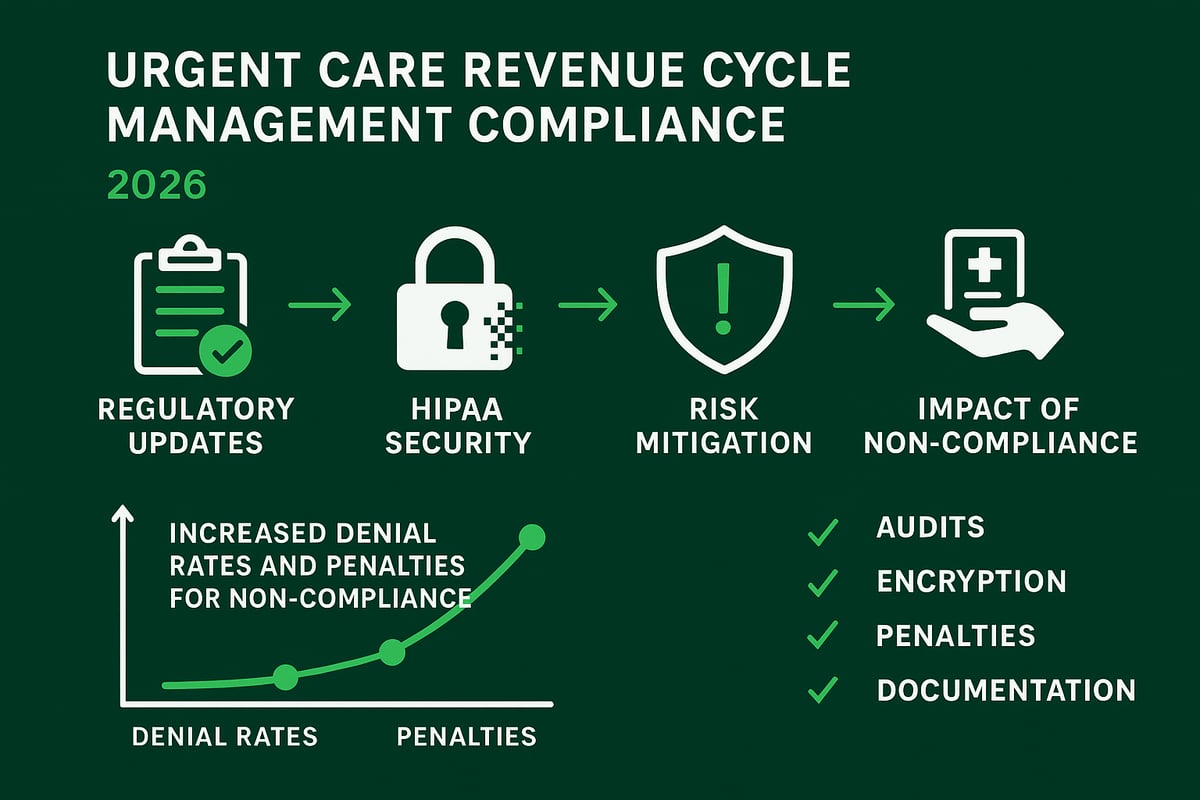
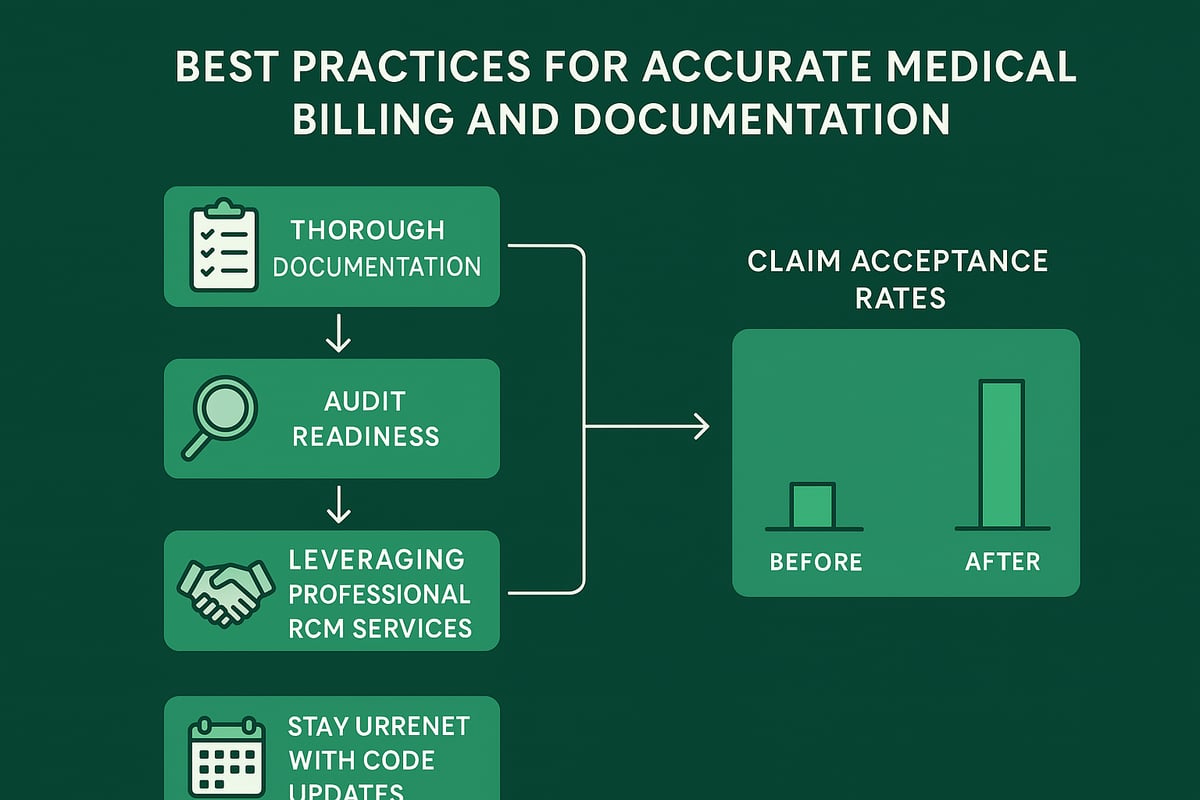
Compliance, Documentation, and Audit Readiness
Staying compliant in 2026 requires healthcare organizations to proactively verify medical insurance details and maintain meticulous documentation. As payer requirements shift and regulatory scrutiny increases, the stakes for accurate record-keeping and audit readiness have never been higher. Practices must embed compliance into every step of their revenue cycle to protect reimbursements and reputation.
Evolving Documentation Standards for 2026
To verify medical insurance effectively in 2026, healthcare providers must align with updated payer and regulatory documentation requirements. Insurers now expect detailed eligibility verification logs, pre-authorization records, and benefit explanation notes for each patient encounter.
Required documentation includes:
- Patient demographics and policy details
- Eligibility check confirmation (date/time, method)
- Pre-authorization and referral records
- Communication logs regarding coverage issues
- Copies of insurance cards and updates
These standards ensure each step to verify medical insurance is audit-ready and defensible, reducing denial risks and supporting seamless claims processing.
Preparing for Payer and Regulatory Audits
Audit readiness is a strategic priority for organizations aiming to verify medical insurance consistently and accurately. Payers and regulators have intensified their focus on documentation precision, with AI-driven audits flagging discrepancies more rapidly than ever. According to recent healthcare denial trends in 2026, incomplete verification records are a leading cause of payment delays and penalties.
Best practices include:
- Maintaining detailed audit trails for every verification
- Retaining records per payer and HIPAA guidelines
- Conducting periodic internal compliance reviews
A single lapse, such as missing eligibility proof, can result in costly fines or lost revenue, underscoring the need for robust audit preparation.
Training and Policy Updates
Continuous staff education is crucial to verify medical insurance under evolving 2026 standards. Frequent regulatory changes demand updated internal SOPs and workflow adjustments. Practices should implement regular training sessions on new compliance mandates, documentation best practices, and payer-specific requirements.
Effective training strategies:
- Monthly compliance briefings
- Hands-on workshops for verification protocols
- Quick-reference guides for new payer rules
Consistent staff training directly impacts the accuracy and efficiency of your insurance verification process.
Leveraging Technology for Compliance
Digital tools are transforming the way practices verify medical insurance, offering automated alerts, documentation templates, and real-time compliance checks. Integration with claims processing workflows ensures that verification records are complete and accessible. More organizations are adopting automated compliance checks, streamlining audit preparation and reducing manual errors.
Partnering with an experienced RCM team ensures technology is applied strategically, supporting both compliance and operational performance. To see how documentation fits within the larger claims cycle, visit Medical Insurance Claims Processing for an overview of best practices.
Best Practices and Future Trends in Insurance Verification
In 2026, healthcare organizations must adopt forward-thinking approaches to verify medical insurance efficiently. Staying ahead means leveraging data, streamlining workflows, and building trust with patients and payers alike. This section explores the most effective strategies and emerging trends shaping insurance verification for providers and RCM partners.
Proactive Verification and Patient Communication
Proactively verify medical insurance before every patient visit to minimize delays and denials. Early eligibility checks help clarify coverage, reduce billing surprises, and improve collections. Educating patients about their insurance status and financial responsibility fosters transparency and loyalty.
Use multiple channels, such as phone, text, and secure portals, to communicate coverage details. By making insurance verification a routine part of patient intake, clinics can reduce confusion and build stronger relationships.
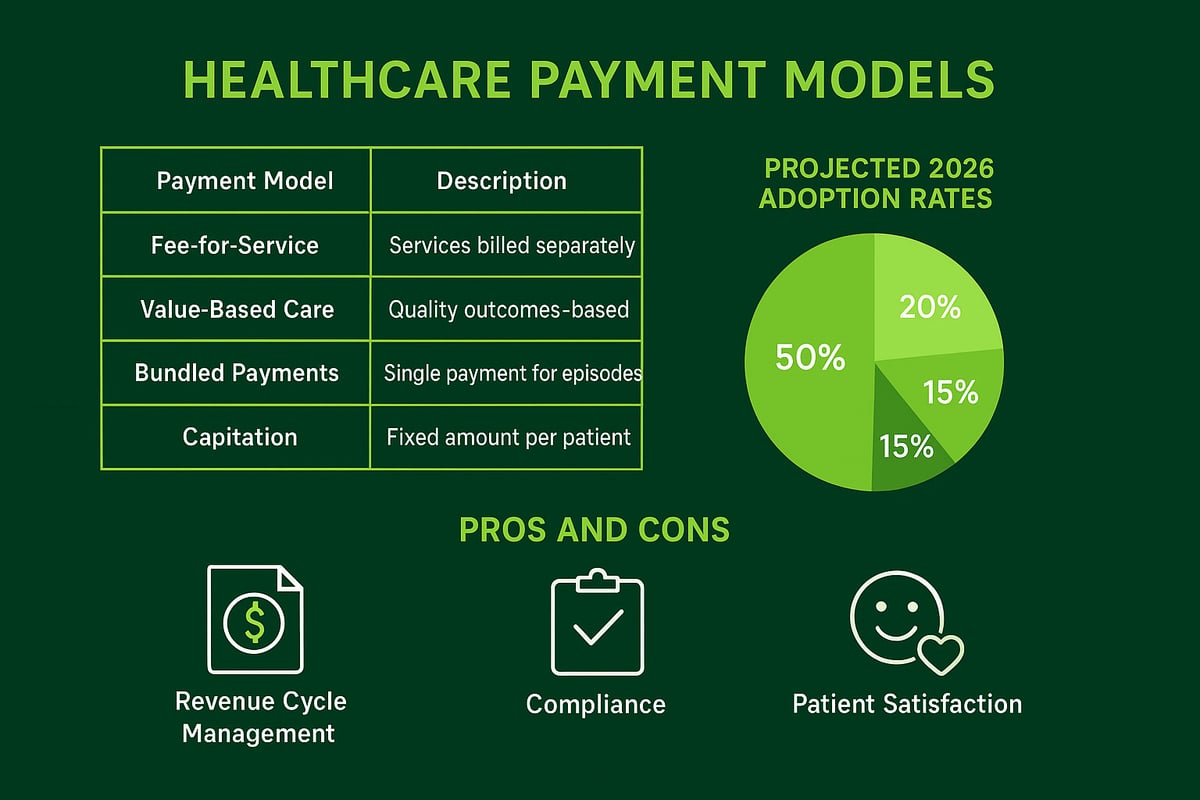
Continuous Improvement and KPI Tracking
To optimize how you verify medical insurance, establish clear KPIs and track them consistently. Focus on metrics like denial rates, verification turnaround times, and patient satisfaction scores. Regular review of these indicators uncovers process gaps and training needs.
Here is a sample KPI comparison table:
| KPI | 2026 Benchmark |
|---|---|
| Eligibility Denial Rate | < 3% |
| Verification Turnaround | < 24 hours |
| Patient Satisfaction | 90%+ |
Continuous monitoring ensures your team adapts quickly to payer changes and sustains high performance.
Adapting to Regulatory and Payer Changes
The regulatory landscape for those who verify medical insurance is becoming more complex. Legislative updates and payer bulletins frequently introduce new requirements. For instance, projected double-digit medical trend rates in 2026 are expected to impact employer-sponsored plans, as highlighted in the 2026 Health Trends report.
Stay current by subscribing to industry updates, attending webinars, and regularly reviewing payer communications. Rapid adaptation is essential for compliance and financial stability.
The Role of Professional RCM Partners
Professional RCM partners are instrumental in helping healthcare organizations verify medical insurance accurately and efficiently. Their expertise in payer policies, documentation, and audit readiness drives both compliance and revenue cycle performance.
RCM specialists work within client-owned platforms, ensuring seamless integration with existing workflows. By outsourcing verification tasks, organizations can reduce administrative burden, lower denial rates, and focus on patient care.
Anticipating Future Technology and Policy Shifts
Emerging technologies are transforming how organizations verify medical insurance. AI-driven tools, real-time data exchange, and blockchain frameworks are enhancing privacy, accuracy, and speed. Innovations such as blockchain-integrated medical insurance claim processing are poised to further secure sensitive data and streamline verification tasks.
Successful practices invest in ongoing training and system upgrades to remain competitive. By anticipating and embracing these trends, providers and RCM partners ensure long-term success in a rapidly evolving environment.
As we’ve explored, staying ahead of evolving payer requirements, regulatory updates, and new technology is critical for mastering medical insurance verification in 2026. If you want to ensure your practice is ready to reduce denials, maximize reimbursements, and maintain compliance, expert guidance can make all the difference. At Greenhive Billing Solutions, we’re here to help you navigate these changes with confidence and clarity. If you’re ready to streamline your verification process and empower your team with the latest strategies, let’s connect. Book Your Free Consultation and discover how we can support your success.