Efficient gastroenterology revenue cycle management is essential for maintaining the financial strength of GI practices. Gastroenterology providers face unique billing and reimbursement challenges, from high-volume procedures to complex payer policies.
When managed well, practices see higher collections, fewer denials, and smoother workflows. This guide offers an actionable, step-by-step approach to gastroenterology revenue cycle management.
Explore fundamentals, optimization strategies, technology integration, best practices, and emerging trends so your GI practice can thrive today and in the future.
Understanding the Gastroenterology Revenue Cycle
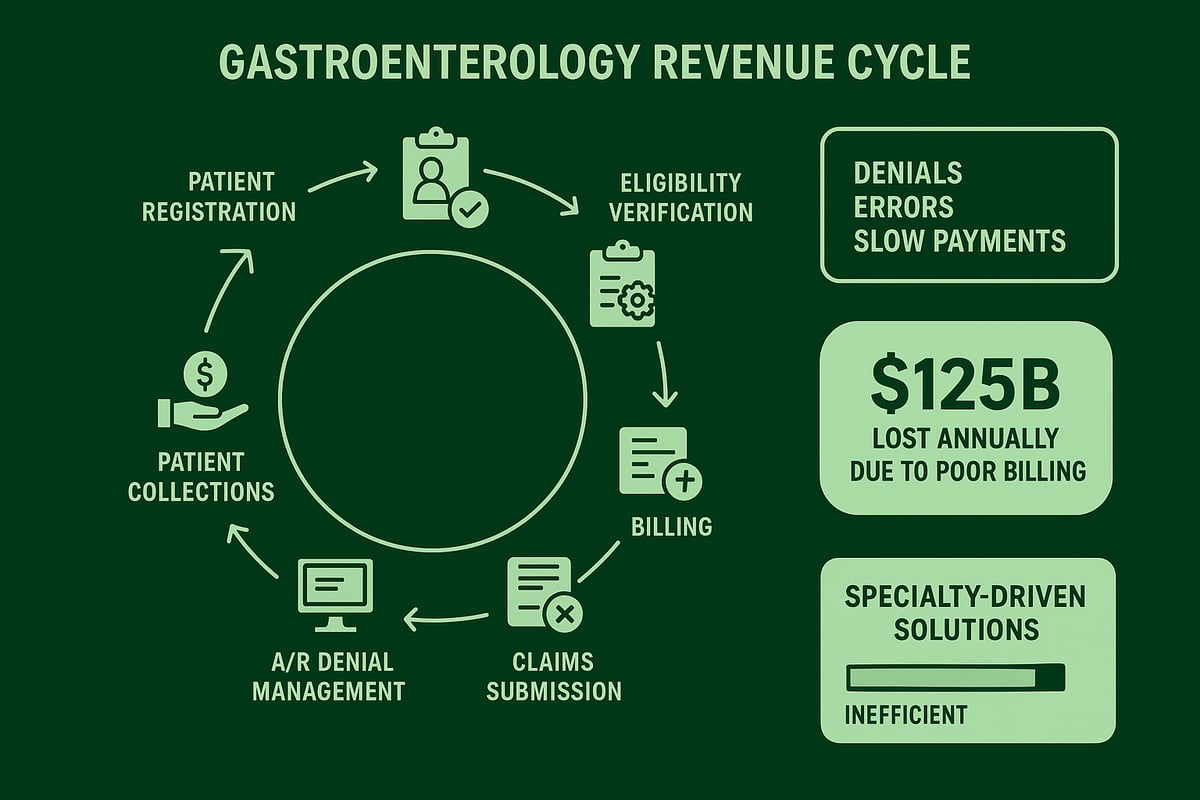
The revenue cycle in a gastroenterology practice covers every step from a patient’s first appointment to the final payment received. It is a complex process, shaped by the unique clinical and operational realities of GI care.
Gastroenterology practices manage a high volume of procedures, such as colonoscopies and endoscopies, each with their own payer rules and frequent requirements for prior authorization. These factors add layers of complexity to every billing cycle.
The main stages of the revenue cycle include patient registration, eligibility verification, detailed GI-specific coding, timely billing, claims submission, denial management, accounts receivable (A/R) follow-up, and patient collections. Each stage must be carefully managed to avoid costly errors.
Common pain points for GI providers include high denial rates, manual data entry errors, slow reimbursement, and a lack of real-time financial visibility. According to Healthcare Business & Technology, US doctors lose an estimated $125 billion annually due to poor billing practices.
A typical GI practice workflow might involve verifying insurance for a colonoscopy, ensuring correct procedure codes are captured, submitting clean claims, and actively following up on any denials. When any part of this workflow breaks down, it directly impacts cash flow and can even affect patient care.
To overcome these challenges, practices increasingly turn to specialty-driven solutions. Addressing the unique RCM challenges in gastroenterology practices is essential for improving efficiency and financial performance.
Step-by-Step Guide to Optimizing Your GI Revenue Cycle
A robust gastroenterology revenue cycle management strategy requires a systematic, stepwise approach. By addressing each stage of the revenue cycle, practices can maximize collections, minimize denials, and achieve sustainable growth. Below is a detailed, actionable guide tailored for GI practices.
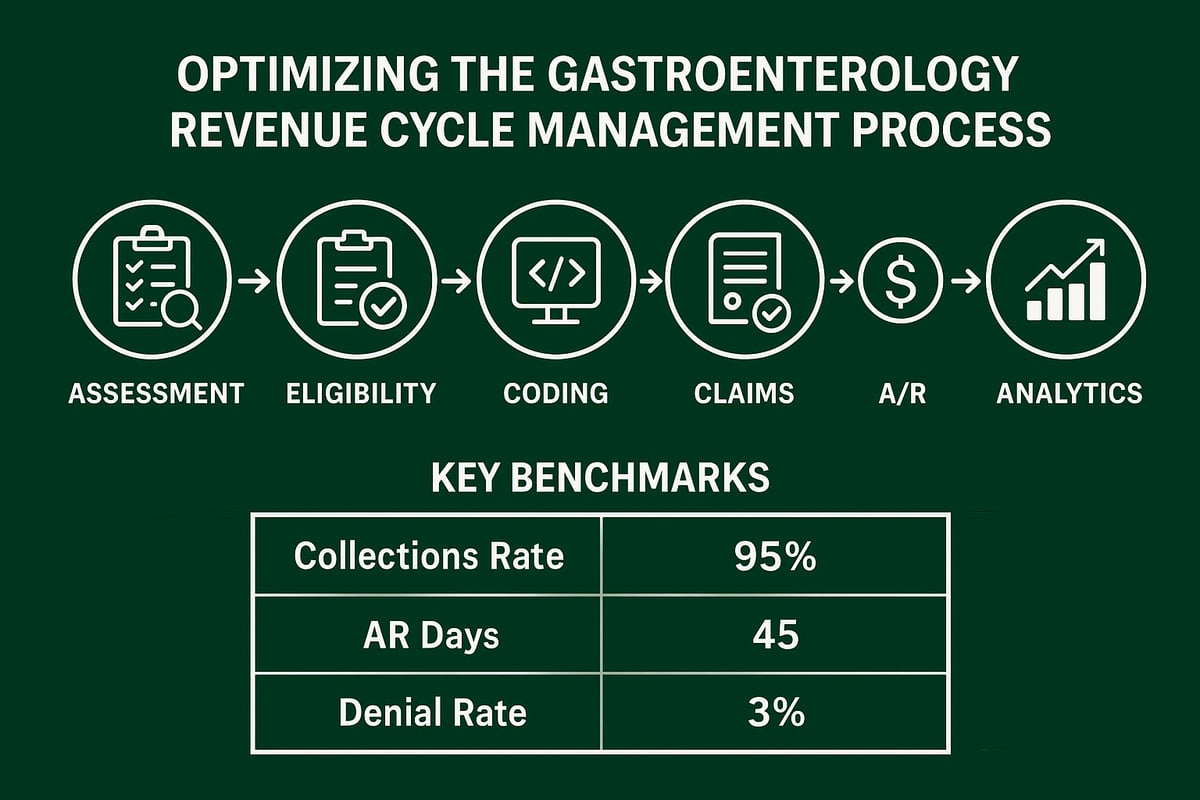
Step 1: Comprehensive Practice Assessment & Gap Analysis
Start with a thorough review of your gastroenterology revenue cycle management performance. Assess financial health by analyzing:
| Metric | Benchmark |
|---|---|
| Net Collection Ratio | ≥ 98% |
| Days in A/R | ≤ 25 |
| Write-off Percentage | < 2% |
Review clinical collections, aged receivables, and denial patterns. Many GI practices lose revenue from under-coded procedures or ignored denials. Benchmark against industry standards, then set clear, measurable improvement goals.
Step 2: Insurance Eligibility Verification & Prior Authorization Management
Verify insurance coverage before every patient visit to prevent claim denials. Efficient prior authorization management is critical for high-volume GI procedures such as colonoscopies and endoscopies. Track changes in payer rules and adapt quickly.
Leverage real-time eligibility verification tools or experienced staff to ensure all approvals are secured before services are rendered. This proactive step reduces delays and increases your clean claim rate.
Step 3: Accurate GI-Specific Coding & Documentation
Certified coders with GI expertise are essential for capturing the full value of your services. Focus on CPT, ICD-10, and modifier accuracy for common services like colonoscopies, biopsies, and E/M visits. Ensure documentation meets payer requirements.
Minimize denials by addressing common errors. For deeper insights, explore medical coding revenue cycle management strategies tailored to GI practices. Plutus Health, for example, maintains a 98% coding accuracy rate in this specialty.
Step 4: Claims Submission, Scrubbing, and Denial Prevention
Submit claims within 48 hours of service to accelerate reimbursement. Utilize intelligent claim scrubbing technology to catch errors and meet payer-specific requirements. Strive for a clean claim rate of at least 95 percent.
Monitoring denials and flagging potential mismatches before submission can further reduce revenue loss. Prompt, accurate claims submission directly supports financial stability.
Step 5: Aggressive A/R Management and Collections
Track every claim until resolved to optimize gastroenterology revenue cycle management. A dedicated GI-trained A/R team should:
- Follow up on denials immediately
- Rework and resubmit rejected claims quickly
- Reduce A/R days to 25 or less
- Implement clear, patient-friendly collections processes
Proactive collections and timely appeals prevent revenue from slipping through the cracks.
Step 6: Financial Reporting, Analytics, and Continuous Improvement
Leverage analytics dashboards to monitor KPIs like days in A/R, denial trends, and revenue per procedure. Regularly analyze root causes of denials and adjust workflows based on data insights.
Provide leadership with performance reviews and drive ongoing process optimization. Continuous improvement is essential for long-term practice success.
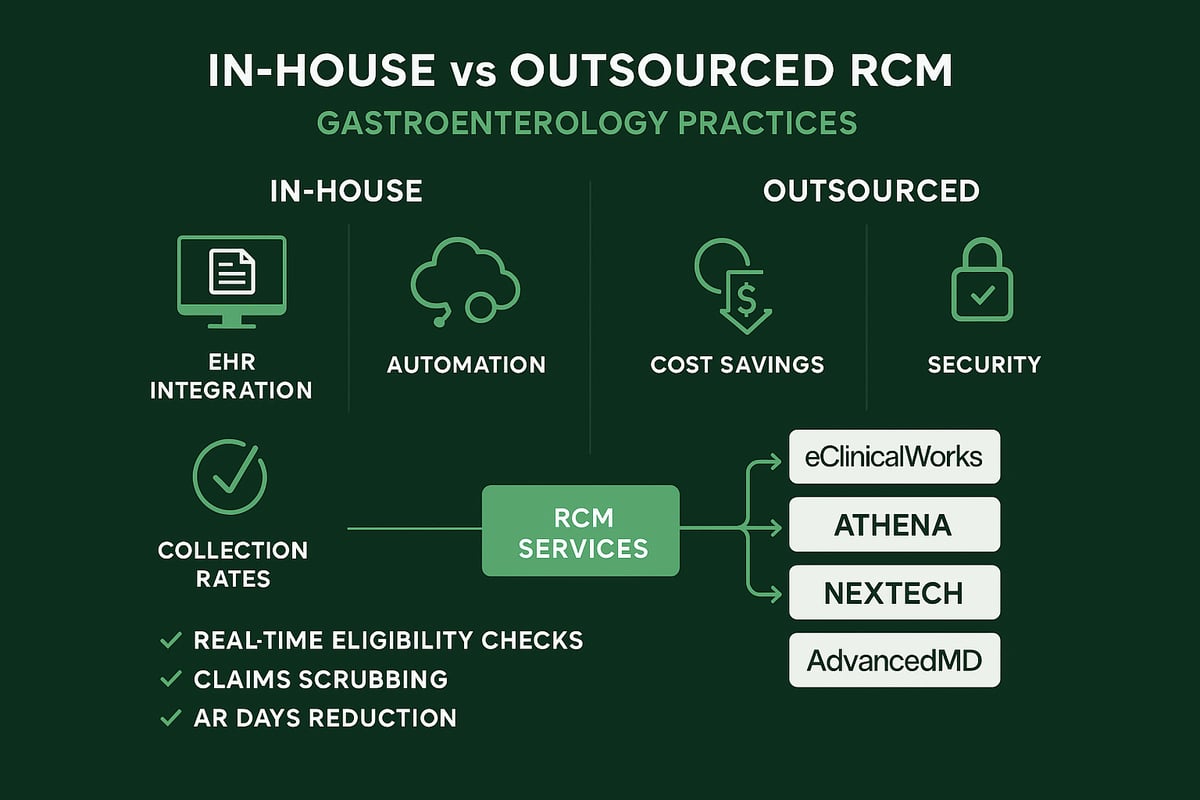
Integrating Technology and Outsourced RCM Services
Modern gastroenterology revenue cycle management demands seamless integration between RCM services and existing EHR or practice management systems. When workflows are connected, practices benefit from real-time data exchange for scheduling, billing, and analytics.
Leading platforms such as eClinicalWorks, Athena, Nextech, and AdvancedMD support direct integration, enabling automated eligibility checks, smart claims scrubbing, and instant reporting. This automation reduces manual errors and accelerates reimbursement.
Outsourcing RCM functions provides significant advantages over in-house teams. Practices gain access to specialized expertise, dedicated compliance monitoring, and scalable resources. According to case study data, outsourced solutions often achieve collection rates above 98% and reduce AR days to under 25.
| Feature | In-House RCM | Outsourced RCM |
|---|---|---|
| Cost Efficiency | Moderate to High | Lower, scalable |
| Expertise | Varies | High, GI-focused |
| Compliance Monitoring | Internal audits | Continuous, external |
| Technology Integration | Limited by staff | Industry best tools |
| Results | Inconsistent | >98% collection |
Outsourced partners also stay current with payer rules, coding updates, and regulatory changes, protecting your practice from compliance risks. Data security and HIPAA compliance are prioritized, with robust protocols for information handling.
Curious about how outsourcing could benefit your practice? Explore the advantages in this revenue cycle management outsourcing resource.
By leveraging integrated technology and expert RCM services, GI practices can streamline operations and boost financial performance.
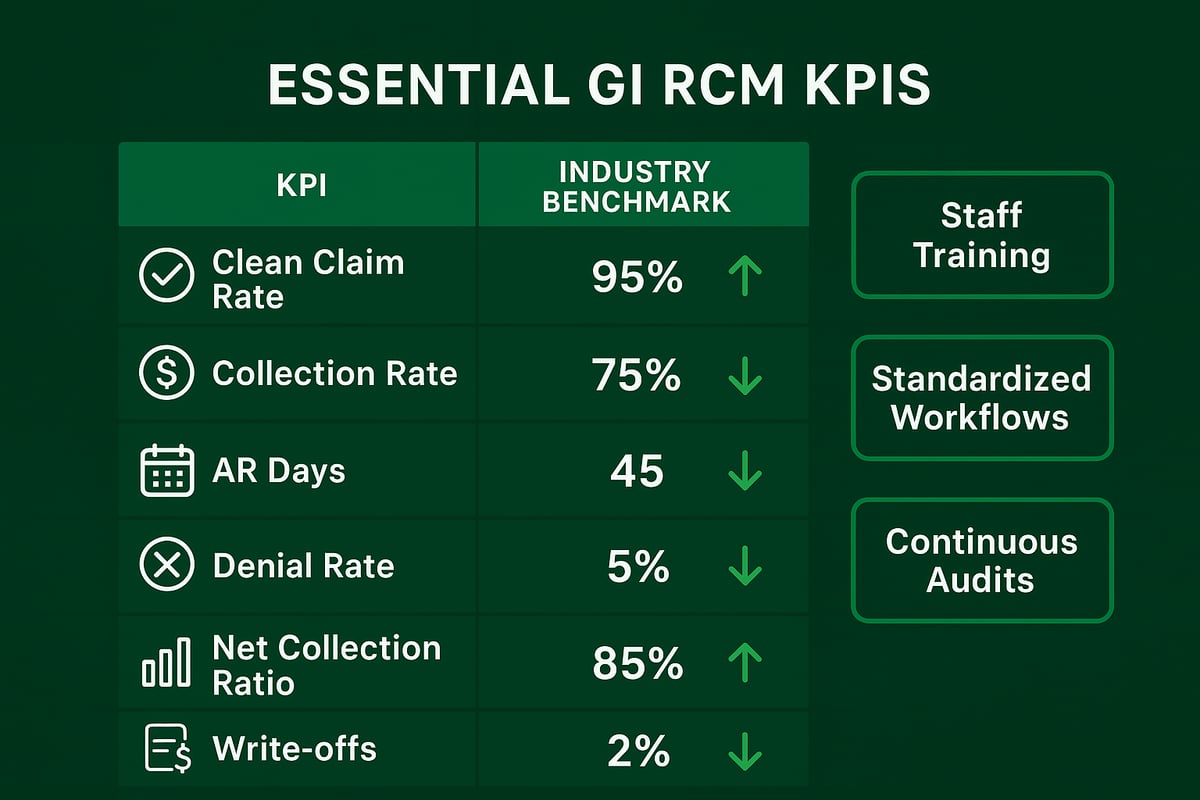
Best Practices and Key Metrics for GI RCM Success
Achieving optimal gastroenterology revenue cycle management requires clear best practices and a sharp focus on performance metrics. Successful GI practices track key indicators to identify strengths and close revenue gaps.
| KPI | Benchmark |
|---|---|
| Clean Claim Rate | ≥95% |
| Collection Rate | ≥98% |
| AR Days | ≤25 |
| Denial Rate | <5% |
| Net Collection Ratio | ≥96% |
| Write-offs | <2% |
Regular staff training in GI coding and payer rules ensures accurate claims. Standardized workflows and checklists minimize manual errors. Monthly analytics reviews reveal trends, while peer feedback highlights improvements in collections and workflow.
Continuous audits, process updates, and a proactive stance on denial management in medical billing further reduce risk. Data-driven decisions help GI practices adapt quickly, boost revenue, and maintain financial health.
Future Trends in Gastroenterology Revenue Cycle Management
Artificial intelligence and automation are rapidly transforming gastroenterology revenue cycle management. From smart documentation to automated coding and real-time eligibility checks, these technologies are reducing errors and accelerating reimbursements. According to 2025 Revenue Cycle Management Survey Insights, more practices are integrating AI to streamline administrative tasks and predict denials.
Payer scrutiny is intensifying, with evolving coding guidelines for GI procedures. Practices must adapt quickly to regulatory changes and the shift toward value-based care, where interoperability and real-time analytics are essential for success. The U.S. Revenue Cycle Management Market Report 2025 highlights how third-party RCM services are driving industry growth.
Patient-centric billing is also rising, with transparent statements and digital payment options improving satisfaction and collections. Practices leveraging these advancements can enhance both patient experience and financial performance.
To remain competitive, GI practices should stay agile, invest in ongoing education, and partner with RCM experts who understand specialty trends. Industry leaders like ModMed are setting the standard for specialty-specific EHRs, underscoring the value of innovation in this evolving landscape.
As we've explored, mastering gastroenterology revenue cycle management is key to strengthening your practice’s financial health and improving patient care. From optimizing insurance verification to leveraging data-driven analytics, every step you take can make a measurable impact. If you’re ready to pinpoint hidden revenue opportunities, reduce denials, and streamline your workflows, why not get expert insight tailored to your needs? Greenhive Billing Solutions is here to help you navigate the unique challenges of GI billing with proven strategies and transparent support.
Get Your Free Audit
Let’s work together to unlock new financial potential for your practice.