Medical billing, compliance, and data management all rely on codes in medical, yet many healthcare professionals find them confusing or overwhelming. For clinics, practitioners, and administrators, understanding these codes in medical is essential for smooth operations, accurate reimbursements, and regulatory compliance.
This essential guide will help you unlock the fundamentals of medical coding, from the main coding systems and compliance regulations to future trends and practical strategies for optimizing your processes. Whether you oversee a busy practice or manage a healthcare organization, you will gain actionable insights to streamline workflow, reduce errors, and improve revenue cycle management.
Understanding Medical Codes: Foundations and Functions
Medical codes in medical billing and administration form the language that translates complex healthcare encounters into standardized data. These codes in medical records ensure that every diagnosis, procedure, and service is captured accurately, allowing clinics and providers to communicate efficiently with payers, auditors, and regulatory bodies.
What Are Codes in Medical?
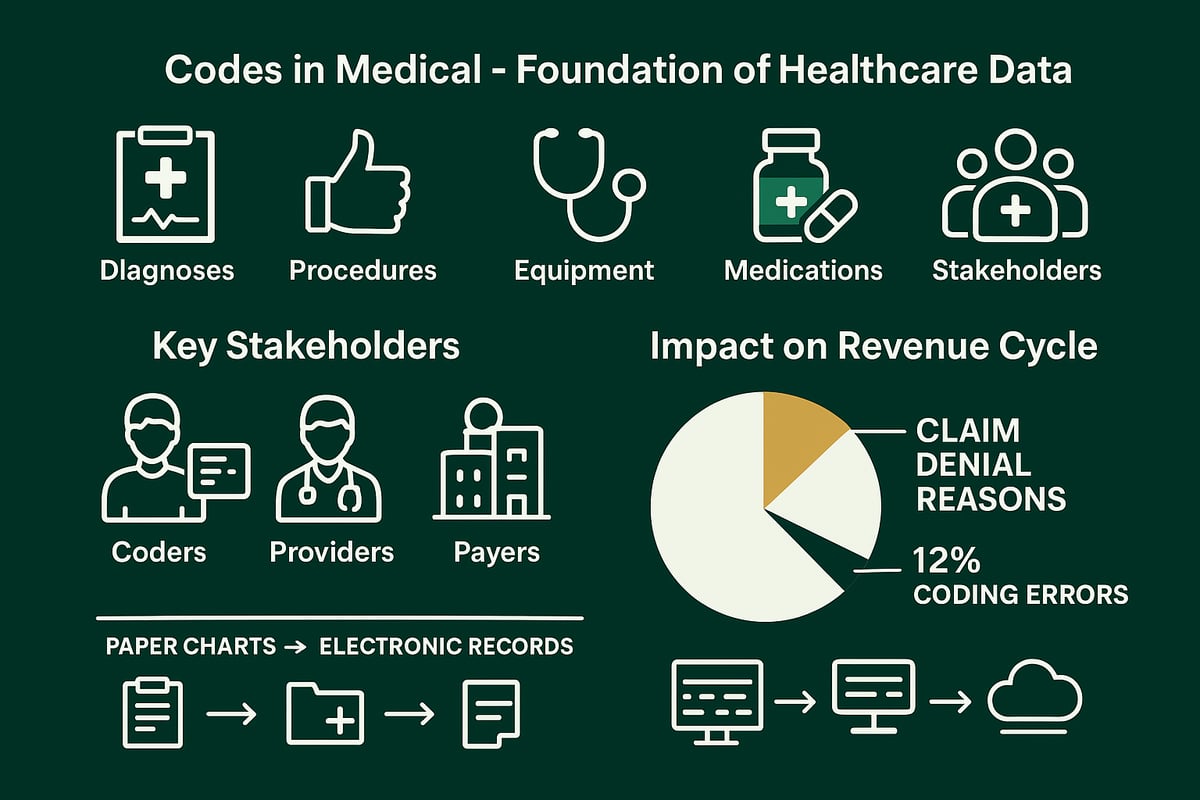
Codes in medical documentation are alphanumeric or numeric representations assigned to clinical concepts. Their core purpose is to standardize the description of diagnoses, procedures, medical equipment, and medications across the healthcare ecosystem. This standardization is vital for accurate billing, insurance claims, and regulatory compliance.
Essential Roles in Healthcare Operations
The functions of codes in medical settings are multifaceted. They drive billing accuracy, streamline insurance claim submissions, and ensure that patient care is documented consistently. Codes in medical workflows also support analytics, enabling practices to track outcomes, measure performance, and identify trends for quality improvement.
Stakeholders in the Coding Ecosystem
A variety of professionals depend on codes in medical processes. Certified coders translate clinical documentation into standardized codes. Billers use these codes to prepare and submit claims. Healthcare providers rely on coding for proper reimbursement and compliance. Payers, such as insurance companies and government programs, use codes to adjudicate claims, while regulators set and enforce coding standards.
Table: Key Stakeholders and Their Roles
| Stakeholder | Role in Medical Coding |
|---|---|
| Coders | Assign and review medical codes |
| Billers | Prepare claims using assigned codes |
| Providers | Document clinical encounters |
| Payers | Process claims, determine coverage |
| Regulators | Set standards, audit for compliance |
The Importance of Accuracy
Accurate codes in medical records have a direct impact on the revenue cycle. Proper coding ensures timely reimbursement, reduces claim denials, and supports compliance with payer and government regulations. Inaccurate coding can lead to underpayment, delays, or even penalties for noncompliance.
Common Coding Errors and Their Impact
Coding errors are a significant concern for healthcare organizations. According to the American Medical Association, up to 12% of claims are denied due to coding errors. Mistakes such as incorrect codes, missing modifiers, or insufficient documentation can cause claim denials or delayed payments. These issues disrupt cash flow and increase administrative workload.
- Example: Entering the wrong procedure code may result in a denied claim.
- Example: Omitting required modifiers can reduce reimbursement or trigger audits.
Types of Data Encoded
Codes in medical systems represent a broad range of information:
- Diagnoses (ICD codes)
- Procedures (CPT, HCPCS)
- Medical equipment and supplies
- Medications
For a detailed overview of the various coding systems used in healthcare, see Types of medical coding explained.
The Shift to Digital Coding
The evolution of codes in medical practice mirrors the shift in healthcare technology. Coding began as handwritten notations on patient charts, but today, most organizations use electronic health records (EHRs) and digital coding tools. This transition has improved accuracy, data accessibility, and the ability to analyze trends for business and clinical decision-making.
Major Medical Coding Systems: ICD, CPT, HCPCS, and Beyond
In healthcare administration, the landscape of codes in medical is shaped by three foundational systems: ICD, CPT, and HCPCS. Each system plays a distinct role in supporting accurate billing, clinical documentation, compliance, and analytics. For healthcare organizations and professionals, mastering these codes in medical is essential for operational efficiency and regulatory alignment.
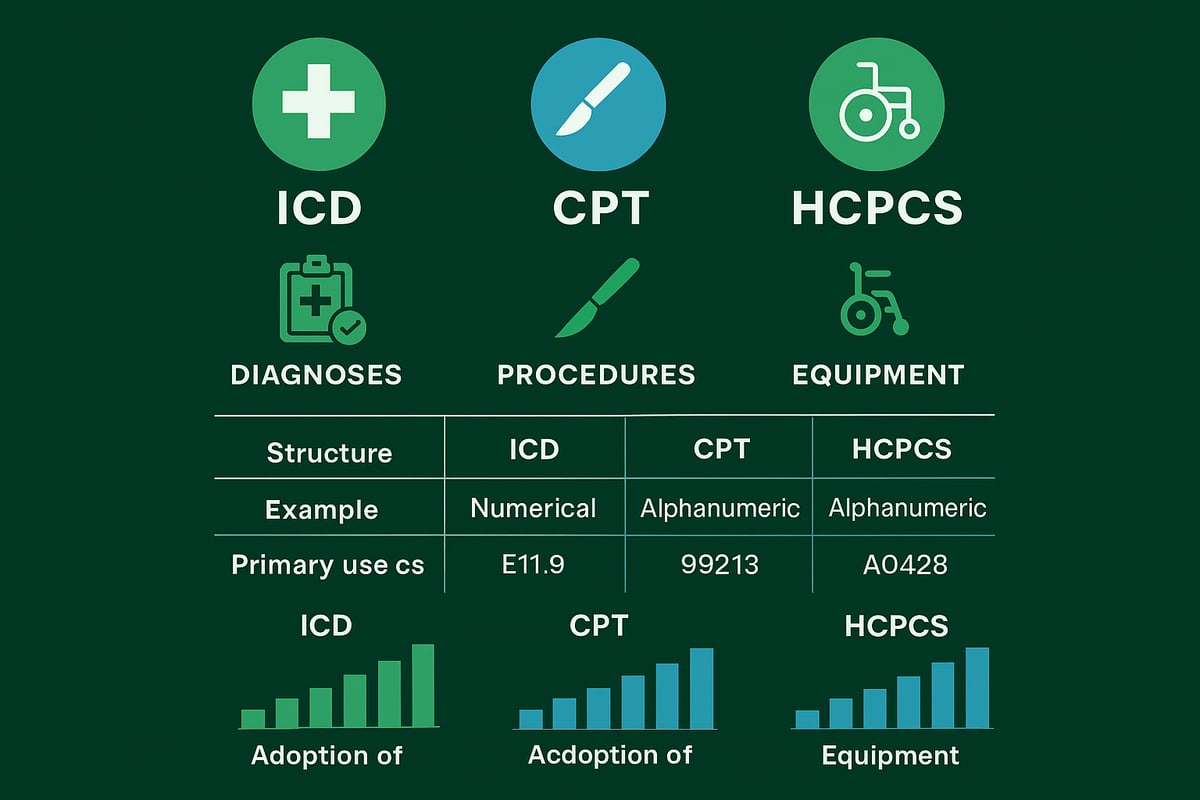
International Classification of Diseases (ICD)
The International Classification of Diseases, known as ICD, is the global standard for coding diagnoses and health conditions. Developed by the World Health Organization, ICD enables consistent tracking and reporting of diseases across countries and care settings. Its structure uses alphanumeric codes to represent specific diagnoses, such as E11.9 for Type 2 diabetes without complications.
ICD is the backbone of codes in medical documentation for hospitals, clinics, and payers. Its applications extend beyond reimbursement, playing a critical role in epidemiology, population health research, and quality measurement. For example, public health agencies use aggregated ICD data to monitor disease trends and allocate resources.
The current widely adopted version in the United States is ICD-10-CM, with updates released annually to reflect new medical knowledge and emerging conditions. Other regions may use localized adaptations to meet unique regulatory or clinical requirements. As healthcare evolves, ICD remains central to codes in medical processes, supporting everything from patient care to global health initiatives.
A simplified table for ICD code structure:
| Code Example | Description | Use Case |
|---|---|---|
| E11.9 | Type 2 diabetes, no complications | Claims, analytics |
| J45.909 | Unspecified asthma, uncomplicated | Population tracking |
ICD continues to adapt, ensuring that codes in medical always reflect the latest clinical realities.
Current Procedural Terminology (CPT)
Current Procedural Terminology, or CPT, is the primary coding system for documenting medical procedures and services in the United States. Developed by the American Medical Association, CPT codes in medical billing capture everything from office visits to complex surgeries. Each code is five digits, often supplemented by modifiers to indicate specific circumstances.
CPT is divided into three categories: Category I for standard procedures, Category II for performance measurement, and Category III for emerging technologies. For instance, the CPT code 99213 represents a standard office visit for an established patient with moderate complexity.
Accurate use of CPT codes in medical claims is vital for proper reimbursement and compliance. Payers rely on these codes to determine coverage and payment rates. Annual updates ensure CPT remains current with evolving medical practice, and professional organizations provide guidance on correct usage.
For more detailed information on how CPT codes are used in healthcare claims, see CPT code usage in healthcare claims.
Sample CPT code in code block:
99213 - Office or other outpatient visit for the evaluation and management of an established patient, moderate complexity
CPT codes in medical workflows help standardize reporting, minimize ambiguity, and support data-driven decision-making.
Healthcare Common Procedure Coding System (HCPCS)
The Healthcare Common Procedure Coding System, or HCPCS, complements ICD and CPT by coding medical supplies, equipment, and non-physician services. HCPCS is structured in two levels: Level I mirrors CPT codes for procedures, while Level II covers products like wheelchairs, medications, and ambulance services. For example, E0114 is the HCPCS code for a standard four-legged walker.
HCPCS codes in medical billing are particularly important for Medicare and Medicaid claims, as they ensure precise tracking and reimbursement for services not covered by CPT. The system is updated regularly to reflect new technologies and healthcare delivery models.
A quick comparison of HCPCS code levels:
| Level | Description | Example |
|---|---|---|
| Level I | CPT-based procedures | 99213 |
| Level II | Supplies, equipment, services | E0114 |
By incorporating HCPCS, organizations can ensure that all aspects of codes in medical are addressed, from high-level diagnoses to the granular details of supply usage. This comprehensive approach supports compliance, transparency, and optimal financial performance.
HCPCS, alongside ICD and CPT, provides the complete toolkit for effective management of codes in medical, ensuring healthcare practices are prepared for regulatory demands and future innovation.
The Role of Medical Coding in Revenue Cycle Management
Medical coding is a vital component of revenue cycle management for healthcare organizations. Codes in medical are more than just data points—they drive the financial health and operational efficiency of every practice. Accurate coding ensures that healthcare providers receive timely, appropriate reimbursement while maintaining compliance with industry regulations.
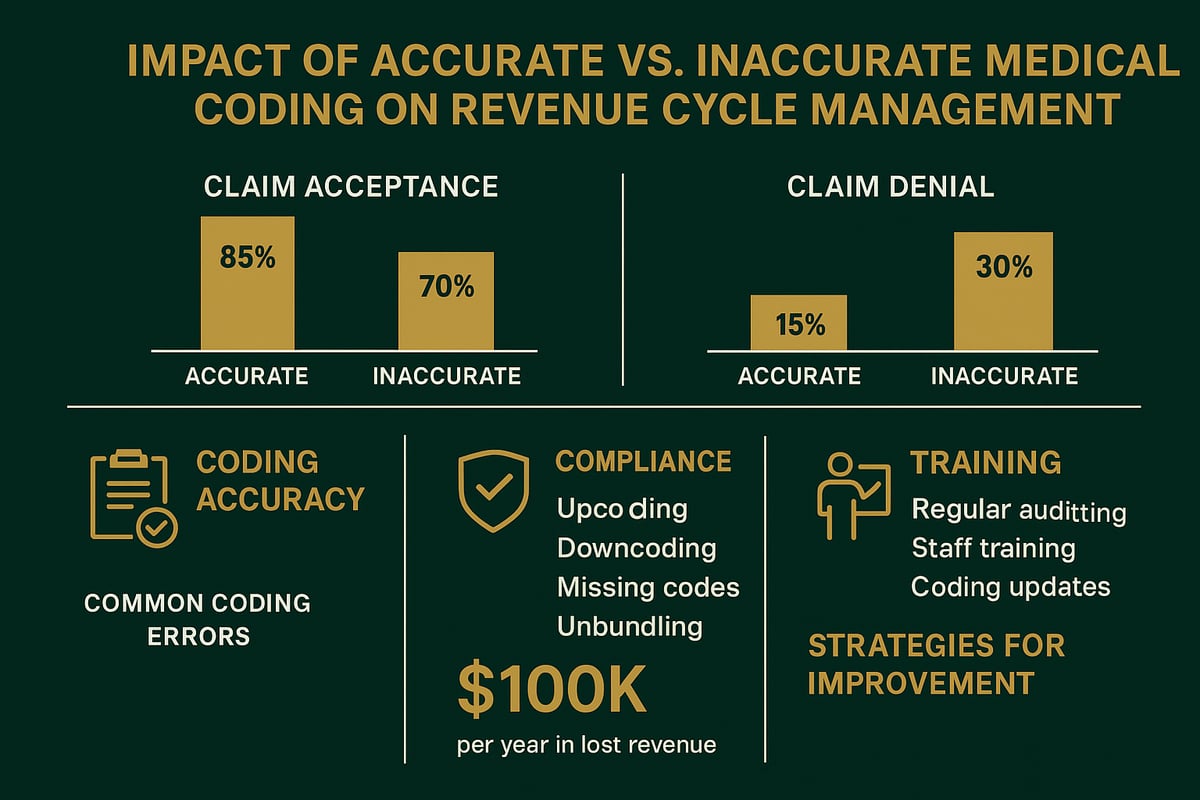
Coding Accuracy and Financial Performance
The precision of codes in medical directly affects your bottom line. Accurate coding streamlines claim processing, improves reimbursement rates, and minimizes costly delays. When codes in medical are entered incorrectly, payers may deny claims, resulting in lost revenue and increased administrative work.
Common coding mistakes include undercoding (failing to report all services), upcoding (reporting services at a higher level than performed), and bundling errors (combining services incorrectly). Each of these can disrupt cash flow and lead to compliance concerns. For example, using the wrong modifier can cause an otherwise valid claim to be denied, costing a practice thousands over time.
According to the Medical Group Management Association, coding errors can result in 20 to 30 percent revenue loss for some providers. The following table summarizes typical coding errors and their financial impact:
| Coding Error Type | Description | Potential Impact |
|---|---|---|
| Undercoding | Missing codes for services provided | Revenue loss, compliance risk |
| Upcoding | Reporting higher-level services | Audit risk, penalties |
| Bundling Errors | Incorrectly combining codes | Claim denials, lost revenue |
To understand how coding precision supports financial success, review this medical coding and revenue cycle management guide for deeper insights.
Compliance, Audits, and Risk Management
Codes in medical also serve as a critical compliance tool for healthcare organizations. Regulatory bodies such as HIPAA, the Office of Inspector General, and private payers require strict adherence to coding standards. Consistency in codes in medical helps ensure that claims meet all necessary requirements and reduces the likelihood of audits or penalties.
Audits can be internal, where your own team reviews documentation and coding practices, or external, conducted by payers or government agencies. Failing to maintain compliance can lead to substantial financial penalties and reputational damage. High-profile cases have shown that fraudulent or negligent coding practices can result in millions in fines.
To manage risk, organizations should:
- Conduct regular internal audits
- Implement clear documentation standards
- Train staff on emerging regulations
- Establish rapid response plans for audit findings
These strategies create a culture of accountability and help practices remain audit-ready.
Training, Certification, and Professional Development
Investing in professional development is essential for maintaining excellence in codes in medical. Certified coders, such as those with CPC or CCS credentials, bring specialized expertise that reduces error rates and improves claim outcomes. Ongoing education ensures that staff stay current with frequent code updates and evolving payer requirements.
Professional organizations like AAPC and AHIMA offer resources, webinars, and certifications that support continued learning. Providing regular training sessions for your coding team can lead to measurable improvements in efficiency and accuracy.
For example, practices that prioritize coder education report fewer denials, faster payments, and greater staff satisfaction. By making professional development a core part of your revenue cycle strategy, you help your organization adapt to industry changes and optimize the use of codes in medical.
Medical Coding Compliance and Regulatory Updates
Navigating codes in medical billing and documentation is a complex process, shaped by evolving regulations and strict oversight. Achieving compliance is not just about accuracy, it is essential for operational integrity, reimbursement, and risk management. Understanding the regulatory landscape, staying current on code changes, and embedding best practices are critical steps for any healthcare organization aiming for long-term success.
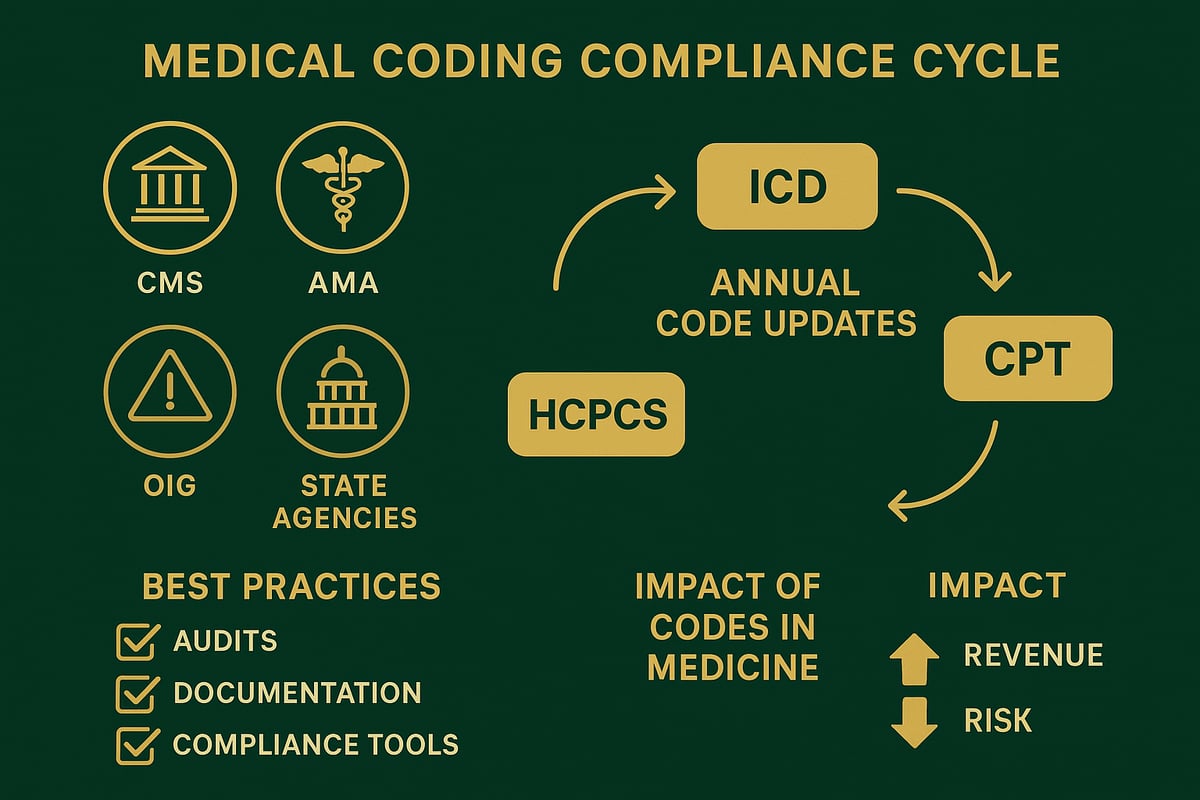
Key Regulatory Bodies and Guidelines
Several regulatory bodies set the standards for codes in medical documentation and billing. The Centers for Medicare and Medicaid Services (CMS) oversees federal compliance, including the implementation of coding edits and payment policies. The American Medical Association (AMA) is responsible for maintaining CPT codes, while the Office of Inspector General (OIG) enforces fraud prevention and risk management.
State agencies may also impose their own rules, adding another layer of complexity for practices operating in multiple jurisdictions. Compliance with codes in medical billing is not optional, it is a legal and financial necessity. For example, the CMS National Correct Coding Initiative (NCCI) establishes edits that prevent improper code combinations, reducing the risk of overpayments or denials.
Organizations must regularly consult these regulatory sources to ensure their codes in medical records meet current standards. Failure to comply can result in audits, financial penalties, and reputational harm, making a proactive approach vital for every healthcare provider.
Recent and Upcoming Changes in Coding Standards
Staying current with codes in medical is a dynamic challenge, as updates occur annually across ICD, CPT, and HCPCS code sets. Each year, regulatory bodies introduce new codes, retire outdated ones, and revise documentation requirements to reflect changes in clinical practice and technology. In recent years, the expansion of telehealth services has led to the addition of new procedure and diagnosis codes for virtual care.
Documentation standards are also evolving, with greater emphasis on specificity and supporting evidence in medical records. Practices must keep their teams informed about these changes to avoid compliance gaps. For detailed insights on the latest and upcoming ICD-10-CM code revisions, refer to the 2026 ICD-10-CM Medical Coding Updates.
Missing or incorrect codes in medical documentation can lead to claim denials or delays, directly impacting revenue and compliance. Forward-thinking organizations establish systematic processes to monitor and implement these updates, ensuring minimal disruption to operations.
Best Practices for Ensuring Compliance
Maintaining compliance with codes in medical requires a structured and proactive approach. Internal audits are essential for identifying errors, monitoring trends, and ensuring adherence to current standards. Establishing routine coding quality checks helps detect inconsistencies before they become costly issues.
Documentation improvement programs are another key strategy. By training staff to provide clear, complete, and accurate clinical notes, organizations reduce the risk of coding errors and support successful audits. Leveraging coding compliance tools, such as real-time validation and checklists, streamlines the review process and enhances accuracy.
Building a culture of accountability and continuous education ensures that compliance is not a one-time effort but an ongoing commitment. Adopting these best practices positions healthcare organizations to thrive in a landscape where codes in medical are central to both financial health and regulatory success.
Future Trends in Medical Coding: Technology, Automation, and Workforce
Medical coding continues to evolve, shaped by rapid advances in technology and shifting healthcare delivery models. For organizations seeking to future-proof their operations, understanding the next wave of trends is essential. From AI-driven solutions to the rise of telehealth, the landscape for codes in medical is transforming how providers, payers, and RCM partners collaborate.
AI and Automation in Medical Coding
Artificial intelligence is revolutionizing how codes in medical are processed and validated. Computer-assisted coding (CAC) platforms and natural language processing (NLP) tools scan clinical documentation, extract relevant data, and suggest accurate code assignments. This technology reduces manual errors, increases coding speed, and helps healthcare practices get reimbursed faster.
One notable advancement is the use of generative AI frameworks. For example, MedCodER: AI Assistant for Medical Coding demonstrates how AI can enhance both the accuracy and efficiency of codes in medical workflows. Automated coding systems support coders by flagging inconsistencies and highlighting documentation gaps, which minimizes claim denials.
Key benefits include:
- Improved accuracy and compliance
- Faster turnaround time for claims
- Reduced labor costs
As AI integration grows, skilled coders will focus more on audit, validation, and exception handling, while routine tasks become automated.
Telehealth and New Care Models
The expansion of telehealth has introduced new challenges and opportunities for codes in medical. Virtual care requires unique procedure and diagnosis codes to capture remote consultations, digital monitoring, and multi-state provider services. This shift has accelerated the adoption of new code sets that address the nuances of telemedicine.
During global health crises, telehealth claims surged and coding teams had to quickly adapt to updated guidelines. Accurate coding ensures proper reimbursement and compliance for virtual visits, remote patient monitoring, and asynchronous communication. As telemedicine becomes a permanent fixture, ongoing updates to codes in medical will be necessary to reflect evolving care models.
Healthcare organizations must:
- Stay updated on new telehealth code releases
- Educate staff on telemedicine documentation standards
- Monitor payer policies for virtual care billing
The adaptability of coding teams is now a competitive advantage in the digital health era.
Workforce Evolution and Skills Demands
The workforce behind codes in medical is also undergoing significant change. Manual coding is giving way to roles focused on coding analysis, audit, and process optimization. Coders now need a blend of clinical knowledge, technical skills, and adaptability to thrive in increasingly automated environments.
According to U.S. Medical Coding Market Growth & Trends, demand for skilled professionals is expected to rise as compliance requirements and coding complexity increase. Remote and hybrid work models are becoming standard, and organizations must provide ongoing training to keep teams current with regulatory updates and new technologies.
Key skills for the future include:
- Proficiency in EHR and coding software
- Data analysis and quality assurance
- Flexibility for remote workflows
Investing in talent development ensures that codes in medical remain accurate, compliant, and aligned with industry best practices.
Steps to Optimize Medical Coding Processes in Your Practice
Optimizing how your organization handles codes in medical settings is crucial for financial health, compliance, and operational efficiency. These five actionable steps help healthcare businesses streamline coding workflows and minimize costly errors.
Step 1: Assess Current Coding Workflows
Begin by mapping your existing codes in medical processes from patient intake to claim submission. Engage coding staff and billing specialists to identify bottlenecks or recurring pain points. Use flowcharts or process maps to visualize each stage.
Gather feedback through brief surveys or team discussions. Look for trends such as frequent claim denials, delays, or documentation gaps. Reviewing workflow data can reveal hidden inefficiencies that impact both cash flow and compliance.
Consider leveraging insights from Revenue codes in medical billing to better understand how revenue codes fit into your process assessment.
Step 2: Invest in Training and Certification
Continuous education is essential for staff managing codes in medical billing. Encourage coders to pursue certifications such as CPC or CCS, which demonstrate expertise and commitment to best practices. Offer access to webinars, workshops, and industry publications to keep your team up to date.
Regularly review job descriptions and training materials to align with evolving regulatory standards. Staying ahead of Upcoming Regulatory Changes Affecting Medical Billing (2025-2030) ensures your staff is always prepared for new documentation and coding requirements.
Prioritize mentorship and knowledge sharing within your organization to foster a culture of continuous improvement.
Step 3: Implement Quality Assurance and Auditing
Establish routine internal audits to verify the accuracy of codes in medical documents. Set clear benchmarks and key performance indicators (KPIs) to track error rates, claim denials, and compliance issues. Use checklists and audit templates tailored to your specialty and payer mix.
Regular peer reviews and double-checks can catch mistakes before claims are submitted. Consider periodic external audits for an unbiased assessment of your coding quality. Early identification of trends, such as undercoding or improper use of modifiers, can prevent revenue loss and compliance risks.
Step 4: Leverage Technology and Automation
Utilize industry-standard tools and platforms to support codes in medical workflows. Integrate electronic health records (EHRs) and coding software to streamline data entry and reduce manual errors. Evaluate computer-assisted coding solutions that can accelerate claim processing and improve accuracy.
Encourage your team to stay informed about emerging technologies and best practices. While our service professionals adapt to client-owned systems, we ensure optimal integration and minimal disruption during transitions.
Step 5: Foster a Culture of Compliance and Continuous Improvement
Promote open communication about challenges related to codes in medical billing and documentation. Schedule regular team meetings to review regulatory updates, audit findings, and process improvements. Encourage all staff to contribute ideas for streamlining workflows and enhancing compliance.
Implement real-time coding validation tools and documentation improvement programs as part of your ongoing strategy. By prioritizing transparency and proactive problem-solving, your organization will remain agile and compliant in a rapidly changing regulatory landscape.
As we've explored, understanding medical codes is crucial for accurate billing, compliance, and the overall financial health of your practice. Even a small coding error can mean lost revenue or unnecessary headaches with claims and audits. If you want to ensure your coding processes are on track and identify areas for improvement, why not take the next step? With our comprehensive expertise in revenue cycle management and a focus on maximizing your reimbursements, we're here to help. Let us take a closer look at your billing—Get Your Free Audit and see how you can optimize your practice for 2026 and beyond.