Accurate medical billing for behavioral health has never been more critical, as industry regulations and payer requirements continue to evolve. Behavioral health practices face unique billing challenges and higher claim denial rates, making streamlined processes essential for financial health. This comprehensive guide walks you step-by-step through mastering medical billing for behavioral health, offering actionable solutions to maximize reimbursements and ensure compliance. You will discover strategies for handling industry-specific coding, insurance verification, documentation, workflow optimization, regulatory updates, and proven best practices. Stay ahead and transform your billing operations with the insights ahead.
Understanding the Unique Challenges of Behavioral Health Billing
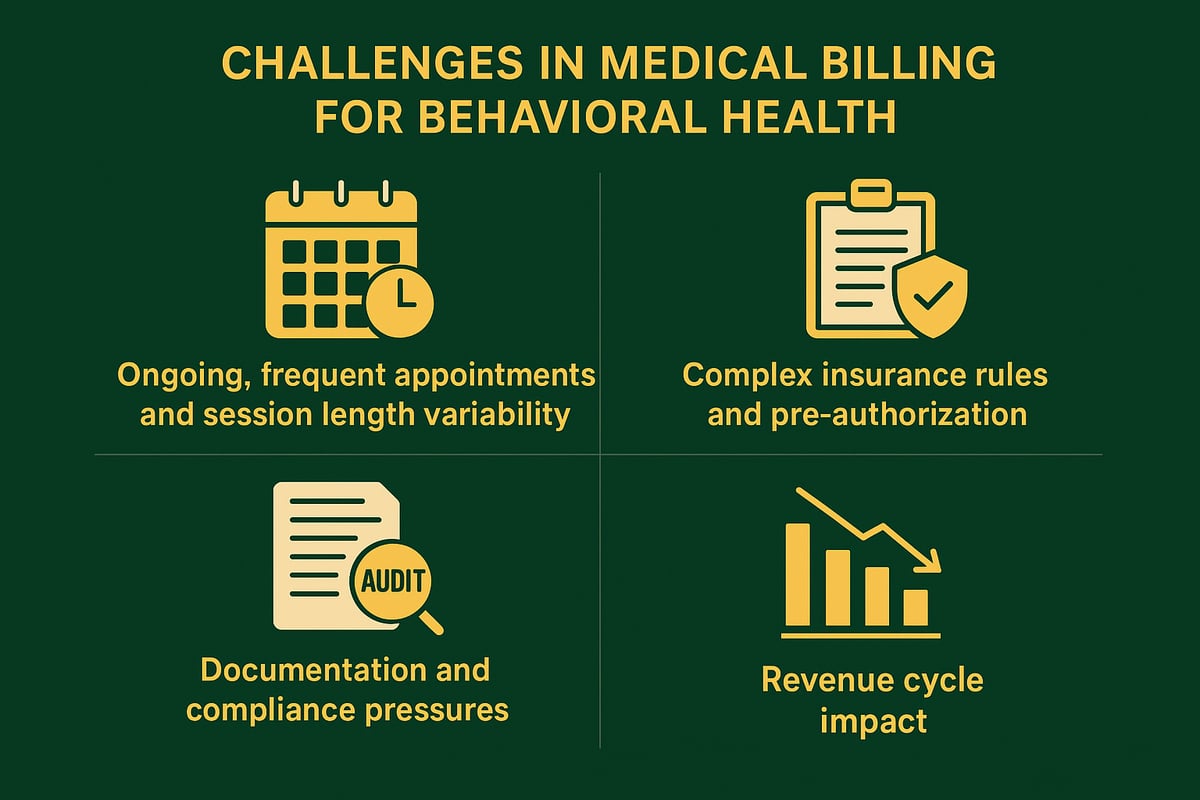
Behavioral health practices encounter a unique landscape when it comes to medical billing for behavioral health. Unlike general medical specialties, these providers must navigate complex service delivery, payer requirements, and documentation standards. Understanding these challenges is essential for optimizing revenue and maintaining compliance.
The Distinct Nature of Behavioral Health Services
The landscape of medical billing for behavioral health is defined by ongoing, subjective, and time-intensive care. Providers often see patients for recurring therapy sessions, which might be weekly, bi-weekly, or monthly, and session lengths can vary from 30 to 60 minutes or more. Each encounter increases claim volume per patient, requiring robust tracking.
Unlike many other specialties, behavioral health services demand more detailed clinical documentation to justify medical necessity. Insurers frequently rely on third-party administrators who impose their own billing and reporting requirements, further complicating the process for providers.
Insurance Complexity and Payer Rules
Insurance coverage for behavioral health is often managed separately from general medical benefits, making medical billing for behavioral health a more intricate process. Practices must verify behavioral health benefits, as session limits, co-pays, and pre-authorization requirements can differ widely between payers.
Some insurers only approve a fixed number of sessions per year or require ongoing medical necessity reviews. Failure to comply with payer-specific rules often results in higher denial rates. Staying current on each payer’s policies is critical to ensure claims are processed efficiently and accurately.
Documentation and Compliance Pressures
Medical billing for behavioral health faces intense scrutiny around documentation. Insurers demand that every billed code is supported by thorough clinical notes, directly tied to the patient’s progress and treatment plan. Any mismatch between documentation and codes can trigger claim denials or post-payment audits.
For example, billing for an extended 60-minute session requires explicit justification in the clinical record. Inadequate documentation is a leading cause of denied claims, putting practices at risk for revenue loss and compliance violations.
Impact on Revenue Cycle and Practice Operations
The unique demands of medical billing for behavioral health directly affect the revenue cycle and day-to-day operations. Inefficient billing can lead to delayed payments, increased accounts receivable days, and a heavier administrative workload for staff.
Practices must find a balance between delivering high-quality care and adhering to evolving billing requirements. According to industry reports and Behavioral Health Medical Billing Best Practices, behavioral health practices consistently report higher denial rates than other specialties, highlighting the need for continuous process improvement and staff education.
Step-by-Step Guide to Behavioral Health Medical Billing
Navigating medical billing for behavioral health requires a structured, detail-oriented approach. By following a proven workflow, practices can reduce errors, speed up reimbursement, and stay compliant. Here is a step-by-step guide to streamline your billing process and maximize revenue.
![]()
Step 1: Patient Intake and Insurance Verification
The first step in medical billing for behavioral health is collecting thorough patient demographics and insurance information. This ensures every claim starts on solid ground.
- Use a standardized intake checklist to gather details.
- Verify behavioral health benefits, session limits, co-pays, deductibles, and network status.
- Confirm pre-authorization requirements before the first appointment.
For a detailed guide on optimizing this process, see insurance verification in billing. Accurate verification reduces eligibility denials and prevents unexpected patient balances. Practices that prioritize this step set the foundation for clean claims and faster payments.
Step 2: Accurate and Compliant Documentation
Compliant documentation is the backbone of medical billing for behavioral health. Insurers demand progress notes that justify the billed code, session length, and therapeutic interventions.
- Link notes to treatment plans and diagnosis codes.
- Reference SAMHSA or industry guidelines to meet standards.
- Document the clinical necessity for extended sessions.
For example, a 60-minute session requires detailed rationale for the time billed. Thorough documentation not only supports reimbursement but also prepares your practice for audits and compliance reviews.
Step 3: Proper Coding and Charge Capture
Selecting the correct CPT and ICD-10 codes is vital in medical billing for behavioral health. Codes must accurately reflect services rendered and diagnoses documented.
- Use common codes such as 90791, 90832, 90834, 90837, and 90853.
- Avoid mismatches between codes and documentation.
- Regularly update code lists to prevent outdated submissions.
A common pitfall is coding errors, which are a leading cause of claim denials. Ensure your billing team stays current with coding changes and conducts periodic audits to maintain accuracy.
Step 4: Claims Submission and Tracking
Submitting claims promptly and tracking them is essential for efficient medical billing for behavioral health. Delays or errors can cause payment lags and increased A/R days.
- Submit claims electronically or manually as required by payers.
- Use clearinghouses or RCM partners to streamline the process.
- Set automated reminders for timely filing and follow-ups.
Monitor claim status and address pending or denied claims quickly. Consistent tracking helps practices identify bottlenecks and maintain a healthy revenue cycle.
Step 5: Payment Posting, Denial Management, and Patient Billing
The final step in medical billing for behavioral health is accurate payment posting, effective denial management, and clear patient billing practices.
- Post payments promptly and reconcile with EOBs.
- Analyze denials, identify root causes, and resubmit corrected claims.
- Communicate transparently with patients about balances and payment options.
Regular denial analysis reduces repeat errors and improves cash flow. Clear patient communication builds trust and ensures collections are handled efficiently.
Mastering Behavioral Health Billing Codes and Modifiers
Understanding the right billing codes and modifiers is central to effective medical billing for behavioral health. Accurate use not only ensures proper reimbursement but also keeps your practice compliant with payer requirements. Let’s break down the essentials for providers and billing teams.
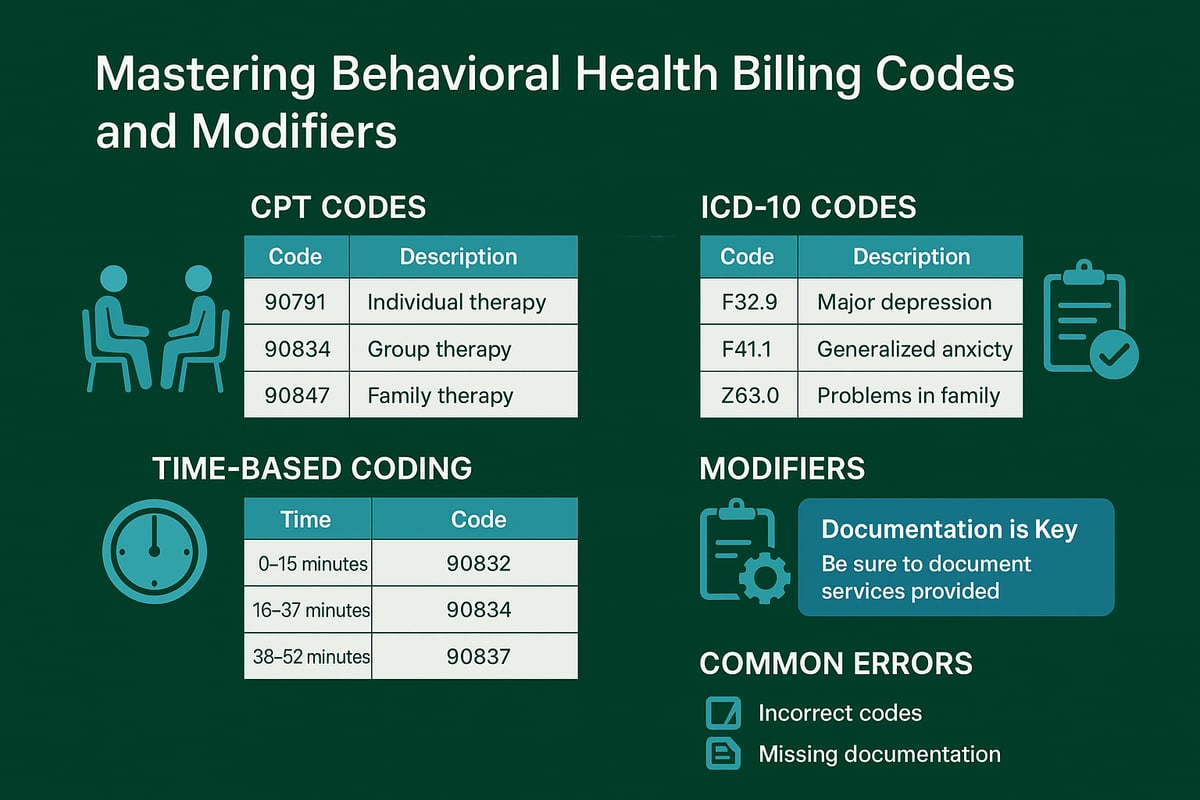
CPT and ICD-10 Codes Essential for Behavioral Health
Medical billing for behavioral health relies on precise coding to reflect each service rendered. CPT codes for psychotherapy include 90791 (diagnostic evaluation), 90832 (30 minutes), 90834 (45 minutes), and 90837 (60 minutes). Group therapy is billed under 90853, while family sessions use 90846 or 90847.
ICD-10 codes must match the clinical diagnosis, such as F32.0 for major depressive disorder. Using detailed and specific codes increases approval rates. Avoid unspecified codes, as payers may flag these for audit or deny reimbursement. Proper coding forms the foundation of every successful claim.
Time-Based Coding and Documentation Alignment
Time-based codes are a unique feature of medical billing for behavioral health. For example, 90832, 90834, and 90837 represent sessions of 30, 45, and 60 minutes, respectively. Documentation must clearly indicate session length and clinical necessity for the time billed.
If using add-on codes like +90836 for interactive complexity, include extra documentation to justify the complexity. Billing 90837 without detailed notes explaining the need for a full hour can result in denials. Always align session documentation with the codes submitted to maintain compliance and avoid payment delays.
Modifiers and Place-of-Service Codes
Modifiers play a critical role in medical billing for behavioral health, especially with the rise of telehealth. Use modifier 95 or GT to indicate telehealth delivery, ensuring the payer recognizes the service format. Place-of-service codes, such as 11 for office, 02 for telehealth, and 12 for home visits, specify where care occurs.
Incorrect or missing modifiers can cause claim rejections. Always verify payer requirements for each modifier and place-of-service code, as rules may vary. Integrate modifier checks into your workflow to streamline approvals and minimize rework.
Common Coding Errors and How to Avoid Them
Common errors in medical billing for behavioral health include mismatched codes and documentation, outdated codes, and omission of required modifiers. These mistakes lead to higher denial rates and lost revenue. Regular staff training and coding audits are essential preventive measures.
For a deeper dive into typical pitfalls and how to address them, see this resource on common medical billing coding errors. Staying proactive with education and process reviews ensures your team keeps pace with annual updates and payer changes. This commitment results in cleaner claims and stronger financial outcomes.
Insurance Verification, Prior Authorization, and Payer Requirements
Accurate insurance processes are critical for successful medical billing for behavioral health providers. The landscape is increasingly complex, with unique requirements that directly impact reimbursement and patient satisfaction. Understanding each step, from benefit verification to payer communication, helps practices avoid denials and optimize revenue.
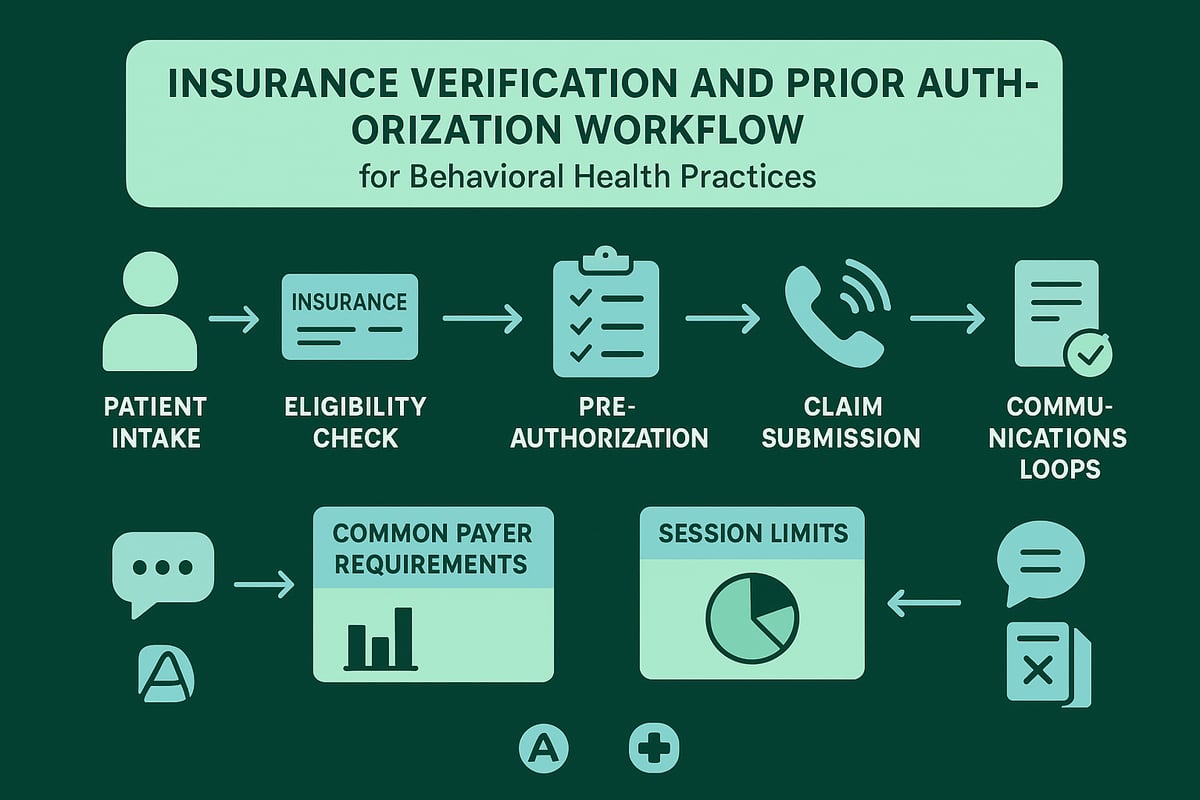
The Importance of Thorough Insurance Verification
Thorough insurance verification is the foundation of effective medical billing for behavioral health. Behavioral health benefits are often distinct from general medical coverage, requiring a specialized approach. Verifying patient eligibility, coverage levels, and benefit limitations before the first session prevents costly claim denials and unexpected patient balances.
Key steps for successful insurance verification include:
- Collecting complete insurance information at intake
- Verifying behavioral health network status and benefits
- Confirming session limits, co-pays, and deductibles
- Identifying if third-party administrators manage behavioral health coverage
Some insurance plans subcontract behavioral health benefits, so extra diligence is needed. A comprehensive verification process ensures that every claim submitted is aligned with the patient’s policy, minimizing financial risks for your practice.
Navigating Pre-Authorization and Session Limits
Navigating pre-authorization requirements is a crucial part of medical billing for behavioral health. Many payers demand prior approval for initial visits, ongoing therapy, or session extensions. Failing to obtain or renew authorizations is a top reason for claim denials in behavioral health.
To streamline this process:
- Track authorization numbers and expiration dates in a centralized system
- Verify if extended sessions or specific CPT codes require additional approval
- Re-verify authorizations when treatment plans change or as session limits approach
For example, some insurers limit the number of covered visits per year, necessitating regular review of patient benefits. Establishing a proactive workflow for pre-authorizations helps ensure uninterrupted care and maximizes reimbursement.
Managing Payer-Specific Rules and Timely Filing
Each insurance payer has unique documentation, coding, and timely filing requirements that directly affect medical billing for behavioral health. Missing a submission deadline or misunderstanding payer rules can result in denied or underpaid claims. Staying current with these requirements is essential for minimizing revenue loss.
Consider using a table to track payer-specific rules:
| Payer Name | Timely Filing Limit | Pre-Auth Needed | Session Cap |
|---|---|---|---|
| Payer A | 90 days | Yes | 20/year |
| Payer B | 120 days | No | 30/year |
Given the increasing complexity, practices should regularly communicate updates and changes to their billing team. For further insights on evolving payer challenges, see Why Behavioral Health Billing Is Getting Harder in 2026. Staying organized and informed reduces the risk of missed opportunities and supports compliance.
Proactive Communication with Patients and Payers
Effective communication is a cornerstone of medical billing for behavioral health. Educating patients about their coverage, out-of-pocket costs, and authorization requirements helps set expectations and minimizes confusion. Providing clear coverage summaries and regular updates fosters trust and reduces disputes.
Maintain open lines with payers to quickly resolve claim issues or clarify policy details. Timely follow-ups on pending authorizations or denials are vital. By prioritizing transparency and responsiveness, your practice can support both patient satisfaction and financial health.
Optimizing the Behavioral Health Billing Workflow
Optimizing the workflow in medical billing for behavioral health is essential for practices aiming to boost efficiency, reduce errors, and maximize reimbursement. A well-structured billing process not only streamlines administrative tasks but also supports compliance and financial stability. By focusing on standardization, leveraging professional services, ongoing staff training, and diligent metric monitoring, organizations can successfully navigate the unique challenges of medical billing for behavioral health.
Standardizing Front-Desk and Billing Procedures
Consistency is the foundation of effective medical billing for behavioral health. Standardizing front-desk and billing protocols ensures all patient data, insurance details, and authorizations are accurately captured from the start. Use checklists and templates for recurring tasks, such as eligibility verification and claims submission. This reduces administrative errors and avoids missed steps that could delay reimbursement.
Typical standardized steps include:
- Collecting patient demographics and insurance cards
- Verifying benefits and pre-authorization requirements
- Utilizing a structured intake form for every new patient
By building these routines into daily operations, practices can ensure smoother medical billing for behavioral health and minimize costly mistakes.
Leveraging Technology and Professional Services
Adopting technology and partnering with experienced professionals can dramatically enhance medical billing for behavioral health. Electronic health record (EHR) systems and billing platforms tailored to behavioral health streamline documentation and claims processes. However, many practices benefit from outsourcing to revenue cycle management specialists who work with your existing systems, providing expertise without requiring a software switch.
Key benefits include:
- Seamless integration with your current EHR
- Access to skilled professionals who adapt to your workflow
- Reduced denials and improved claim turnaround times
This approach allows providers to focus on patient care, with the assurance that their medical billing for behavioral health is managed efficiently and compliantly.
Staff Training and Compliance Monitoring
Continuous education in medical billing for behavioral health is vital. Regular staff training ensures everyone stays current on coding changes, payer updates, and documentation requirements. Quarterly or monthly training sessions can address common errors, reinforce best practices, and adapt to evolving regulations.
Effective compliance monitoring includes:
- Internal audits of billing and documentation
- Scheduled reviews of payer policy changes
- Immediate feedback and correction on identified issues
Investing in staff competency helps maintain high accuracy in medical billing for behavioral health while reducing compliance risks and supporting smooth operations.
Monitoring Claims, Denials, and Revenue Metrics
Diligent tracking of claims, denials, and revenue cycle KPIs is crucial for optimizing medical billing for behavioral health. Practices should monitor clean claim rates, denial rates, and days in accounts receivable to spot trends and identify process gaps. Analyzing denial patterns enables targeted interventions that improve cash flow and reduce recurring errors.
For actionable strategies, consider this Denial management strategies resource, which outlines proven methods to enhance denial resolution and overall financial performance.
By leveraging robust data analytics and proactive denial management, organizations can continually refine their medical billing for behavioral health and achieve stronger financial outcomes.
Regulatory Compliance, Audits, and Industry Updates
Maintaining regulatory compliance is essential for any organization involved in medical billing for behavioral health. With evolving requirements and frequent audits, practices must stay ahead to protect their revenue and reputation. This section explores the pillars of compliance, audit readiness, and strategies for keeping up with industry shifts in medical billing for behavioral health.
HIPAA, Privacy, and Data Security
Protecting sensitive patient information is at the core of medical billing for behavioral health. HIPAA and state privacy laws impose strict rules on data storage, access, and transmission. Every billing team must ensure all data is encrypted, whether at rest or in transit.
Regular security audits help identify vulnerabilities. Staff should receive ongoing training on privacy protocols and breach response. For example, restricting access to only necessary personnel and using secure communication channels are best practices. Proactive monitoring and prompt responses to incidents build trust and minimize legal risks.
Documentation Standards and Audit Readiness
Accurate, timely, and comprehensive documentation is the foundation of compliant medical billing for behavioral health. Insurers and auditors require clear records supporting every billed service, including session length, clinical necessity, and alignment with treatment plans.
To prepare for audits, practices should:
- Maintain organized and up-to-date records
- Use standardized templates for progress notes
- Conduct regular internal documentation reviews
Inadequate documentation often leads to recoupments or denied claims. Consistent audit preparation not only reduces financial risk but also streamlines the workflow for billing teams.
Staying Current with Industry Changes
Medical billing for behavioral health is shaped by frequent updates to CPT codes, ICD-10 classifications, and payer policies. Staying informed is critical to avoid costly errors and compliance gaps. Engaging with professional associations, subscribing to newsletters, and attending webinars are practical ways to keep teams updated.
For deeper insights into industry shifts and revenue cycle management, consider reviewing resources like the Behavioral Health Revenue Cycle Management Guide. Adapting quickly to new requirements ensures your billing processes remain efficient and compliant.
Risk Management and Proactive Compliance Strategies
Implementing robust risk management protocols is vital in medical billing for behavioral health. Internal controls, such as segregation of duties and regular compliance training, help prevent errors and detect fraud. Running mock audits prepares your organization for real payer reviews and uncovers areas needing improvement.
Key strategies include:
- Quarterly staff education on fraud, waste, and abuse
- Periodic review of billing policies and procedures
- Immediate corrective action on compliance violations
Proactive compliance reduces audit anxiety and safeguards your practice’s financial health.
Best Practices and Tips for Maximizing Behavioral Health Billing Success
Success with medical billing for behavioral health depends on a proactive, strategic approach. To maximize reimbursements and reduce errors, behavioral health practices need to implement proven best practices across their entire revenue cycle. The following actionable tips will help you build a foundation for sustainable growth and compliance.
Building an Efficient Billing Team or Partner Network
The backbone of successful medical billing for behavioral health is a skilled, specialized billing team. Whether you hire in-house staff or partner with an experienced RCM provider, prioritize professionals with behavioral health expertise and certification.
Collaboration between clinicians and billing staff is essential. Schedule regular meetings to review documentation requirements, clarify coding questions, and address workflow concerns. This fosters accurate charge capture and minimizes costly errors.
Consider the following when building your team:
- Hire certified billing and coding professionals
- Ensure ongoing training in behavioral health regulations
- Encourage open communication between clinical and billing teams
A dedicated team directly impacts your bottom line by increasing clean claim rates and reducing denials.
Continuous Process Improvement and Error Reduction
Continuous improvement is crucial for effective medical billing for behavioral health. Regularly evaluate your billing workflows to identify bottlenecks and recurring mistakes. Use denial analysis to uncover root causes and implement corrective actions.
Monthly review meetings are an excellent way to address trends and share updates. Stay informed about industry changes and payer requirements. For more in-depth strategies, explore this comprehensive guide to behavioral health billing strategies for maximizing reimbursement.
Proactive process improvement not only reduces errors but also leads to faster payments and improved staff confidence.
Enhancing Patient Communication and Financial Transparency
Clear communication with patients is a cornerstone of medical billing for behavioral health. Explain insurance benefits, out-of-pocket costs, and payment options before services begin. Use simple language and provide written summaries to reduce confusion.
Offering flexible payment plans and online payment solutions can boost collections while supporting patient satisfaction. Address billing questions promptly and provide staff with scripts for common scenarios.
Key tips include:
- Educate patients about their responsibilities upfront
- Make payment policies easily accessible
- Offer multiple payment methods
Transparent billing practices build trust and reduce disputes.
Leveraging Data and Analytics for Revenue Optimization
Data-driven decision-making is a game-changer in medical billing for behavioral health. Use reporting tools to track key performance indicators such as clean claim rates, denial trends, and days in accounts receivable.
Regularly review these metrics to identify areas for improvement. Implement targeted interventions, such as additional training or workflow adjustments, based on your findings.
A simple table can help summarize important KPIs:
| KPI | Target Benchmark |
|---|---|
| Clean Claim Rate | >95% |
| Denial Rate | <5% |
| Days in A/R | <30 days |
Leveraging analytics helps practices increase revenue, improve efficiency, and make informed business decisions.
As you work toward mastering behavioral health billing, it’s clear that navigating evolving codes, payer rules, and compliance can feel overwhelming. Whether you’re aiming to improve your workflow, reduce denials, or simply gain peace of mind knowing your practice is financially healthy, you don’t have to do it alone. At Greenhive Billing Solutions, we’re committed to helping you optimize every step of your revenue cycle so you can focus on providing exceptional care. If you’d like expert insights tailored to your practice, why not Book Your Free Consultation? We’re here to support your success.