Accurate coding is the backbone of financial stability and compliance for healthcare organizations in 2026. As payer rules grow stricter and audits increase, mastering the right codes for medical billing and documentation is more critical than ever.
This article explores seven essential code sets every provider must know to optimize claims and reimbursement. We will break down how each code impacts your revenue, share actionable tips, and highlight real-world challenges. Ready to protect your bottom line and stay compliant? Start by understanding the codes for medical success.
The Importance of Medical Coding in 2026
The healthcare industry is experiencing rapid transformation, and mastering codes for medical billing is now more critical than ever. As reimbursement models evolve and payer requirements become more complex, healthcare organizations must prioritize accuracy and compliance to protect their revenue and reputation. Understanding the significance of correct coding practices is essential for every provider, clinic, and medical group striving for long-term financial health.
The Evolving Landscape of Medical Billing
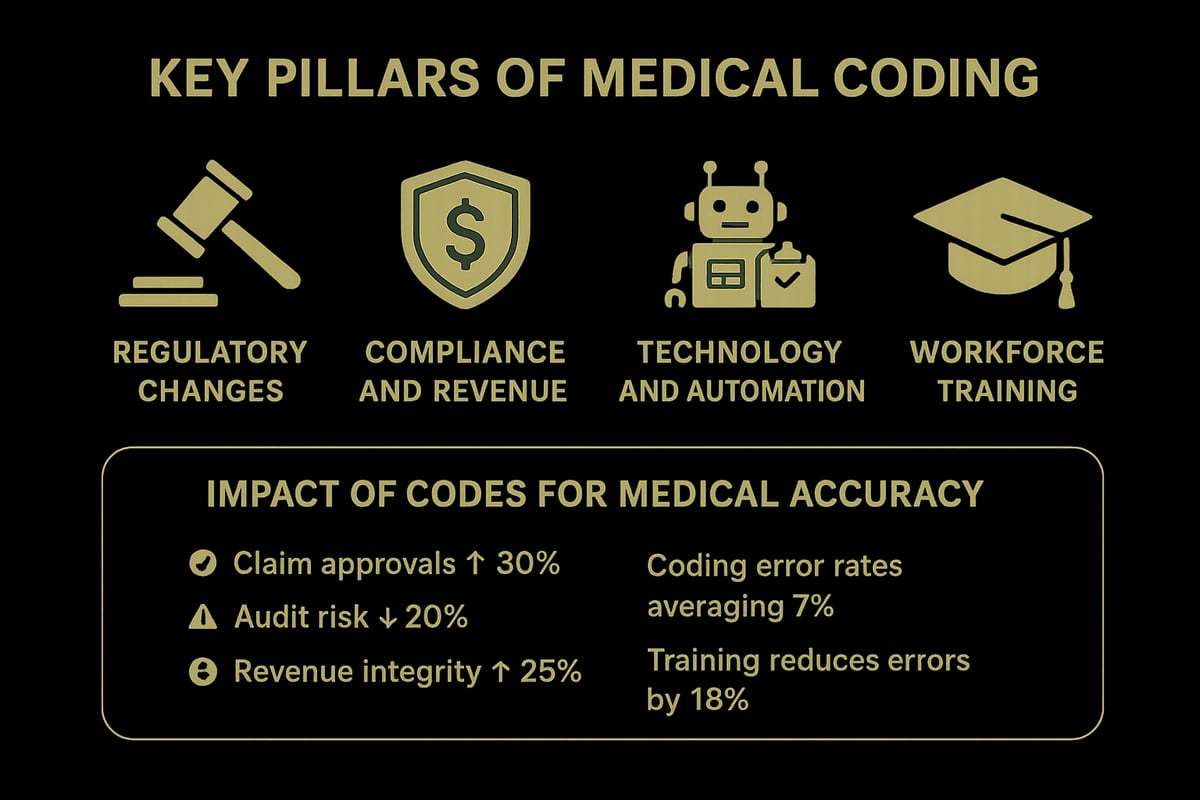
Medical billing is facing unprecedented change in 2026. Regulatory shifts, such as new CMS rules and value-based care initiatives, are reshaping the way organizations approach codes for medical reimbursement. Payers are scrutinizing claims more closely, increasing the risk of denials and audits for incomplete or inaccurate coding.
Recent CMS updates have introduced new requirements for documentation and code selection, directly impacting how providers capture essential data. The transition towards value-based care also means that coding must reflect quality and outcomes, not just services rendered. For a deeper look at the evolving code sets and their impact, Types of Medical Coding Explained provides a helpful overview.
Providers must stay alert to these changes, as even minor missteps can have significant financial and compliance consequences.
Compliance, Accuracy, and Financial Performance
Precise codes for medical billing are the cornerstone of strong financial performance. Accurate coding ensures that organizations receive full reimbursement for services provided, while errors can lead to claim denials, delays, or even penalties under HIPAA and OIG regulations.
Common mistakes, such as upcoding or downcoding, not only risk lost revenue but may also trigger payer audits and reputational damage. For example, a clinic that consistently undercodes chronic care visits might see thousands lost in annual reimbursement, while upcoding could invite costly penalties.
By investing in robust compliance programs and regular chart audits, healthcare organizations can safeguard their financial health and build trust with payers.
The Impact of Technology and Automation
The integration of EHRs and billing automation tools has transformed the management of codes for medical billing. AI-driven solutions now assist with code selection and claim edits, reducing manual errors and increasing efficiency. However, technology is not a replacement for skilled oversight.
Professional review remains essential to catch nuances that automation might miss, such as complex modifier use or documentation gaps. For instance, large clinics implementing automated coding have reported a measurable drop in claim errors, but only when paired with routine audits by certified professionals.
Leveraging both advanced tools and expert review is key to achieving optimal billing outcomes.
Skills and Training for 2026
As coding requirements grow more complex, ongoing education is vital for anyone handling codes for medical claims. Certifications such as CPC and CCS are now standard, reflecting the need for up-to-date knowledge and expertise.
Partnering with experienced RCM service providers can further enhance billing accuracy and efficiency. These experts stay current on code updates and payer rules, helping clients avoid common pitfalls. For example, clinics investing in regular staff training have seen significant improvements in first-pass claim acceptance rates.
Continuous training, certification, and collaboration are essential strategies for staying competitive and compliant in 2026.
Overview of Medical Code Sets
Understanding the main code sets is fundamental for effective billing and documentation in every healthcare organization. These codes for medical claims define the language of reimbursement, compliance, and care tracking. Mastery of these systems is essential for clinics and providers aiming to optimize revenue and avoid costly errors.
![]()
ICD-10-CM: Diagnosis Coding
ICD-10-CM codes for medical diagnoses are the foundation of clinical documentation and billing. This system classifies diseases, symptoms, and external causes with high specificity, supporting accurate claim submission. Each year, updates reflect emerging diseases and revised definitions, impacting payer requirements.
For example, the ICD-10-CM code U07.1 for COVID-19 was rapidly adopted, affecting billing and tracking throughout the industry. Keeping current with these codes for medical ensures compliance and enables providers to capture risk adjustment data for value-based contracts. Annual updates in 2026 will further refine codes for chronic and emerging conditions.
CPT: Current Procedural Terminology
CPT codes for medical services are maintained by the AMA and represent procedures, tests, and outpatient encounters. These codes are central to outpatient billing, forming the basis for most physician and clinic claims. The CPT code set is revised annually to reflect new technologies and care delivery models.
Understanding What is a CPT Code in Healthcare helps organizations select and apply the correct codes for medical procedures, reducing denials and supporting compliance. For instance, telemedicine visits have dedicated CPT codes, which evolve with regulatory changes and payer policies.
HCPCS Level II Codes
HCPCS Level II codes for medical supplies, durable equipment, and non-physician services are essential for billing items not covered by CPT. Governed by CMS, these alphanumeric codes identify products like wheelchairs, medications, and ambulance services.
Correct use of HCPCS Level II codes for medical billing is critical for Medicare and Medicaid reimbursement. Annual updates accommodate new therapies and technologies, requiring providers to review code changes each year. Staying informed on these codes for medical equipment and services prevents claim rejections and compliance issues.
Modifiers and Their Function
Modifiers enhance the specificity of codes for medical billing by indicating variations in procedures or circumstances. Common examples include Modifier 25 for significant, separately identifiable E/M services and Modifier 59 for distinct procedural services.
Applying the right modifiers to codes for medical claims ensures accurate reimbursement and reduces audit risk. However, incorrect modifier use can trigger denials or penalties. Providers must stay updated on modifier guidelines and train staff to document appropriately, as modifier rules often change with each code set update.
7 Essential Codes for Medical Billing and Documentation 2026
Navigating the landscape of codes for medical billing and documentation is more complex and crucial than ever in 2026. Healthcare organizations must master key code sets to secure reimbursement, ensure compliance, and optimize revenue cycle performance. Below, we break down seven essential codes for medical billing, highlighting their significance, correct application, and the latest updates impacting clinical and financial outcomes.
1. ICD-10-CM Code Z00.00: General Adult Medical Examination
ICD-10-CM code Z00.00 is foundational among codes for medical billing, representing a general adult medical examination without abnormal findings. It is primarily used for routine check-ups and preventive care visits, a critical focus under value-based care models in 2026.
To bill this code correctly, providers must document the absence of abnormal findings and detail the scope of the examination. Compliance requires clear evidence in the clinical note that the visit was preventive, not problem-oriented. Payers often scrutinize claims for Z00.00, especially when combined with additional services or tests, making precise documentation essential.
Audit triggers include upcoding preventive visits as problem-focused or missing required elements in the history and exam. Recent guideline changes emphasize specificity, requiring separation of preventive and diagnostic services if performed together. For annual wellness visits, Z00.00 helps drive quality metrics, impacting risk adjustment and reimbursement.
Common payer rules now demand explicit statements regarding the patient’s preventive status and the absence of symptoms. Failure to meet these criteria can result in claim denials or recoupments, directly affecting revenue. In 2026, updates clarify documentation standards and reinforce the importance of using codes for medical billing with accuracy.
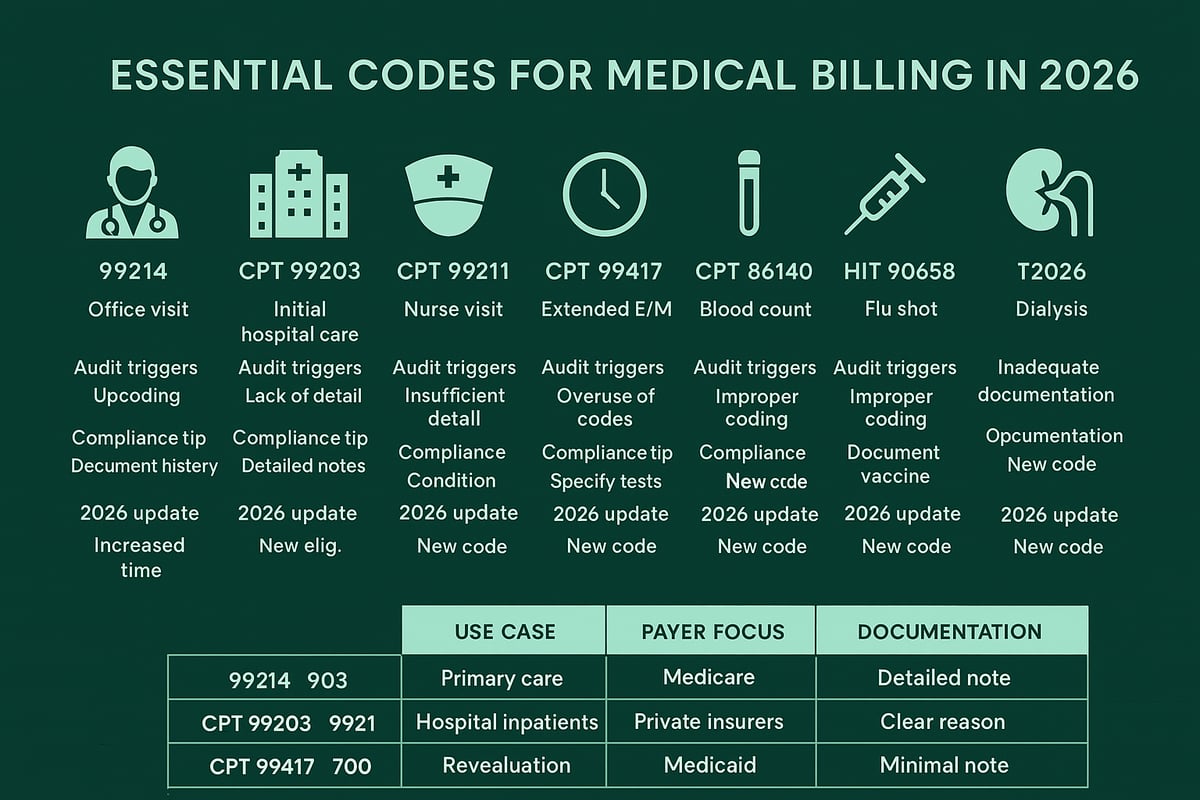
2. CPT Code 99214: Established Patient Office Visit, Level 4
CPT code 99214 is one of the most frequently used codes for medical office visits, denoting a Level 4 encounter for established patients. This code reflects moderate complexity in history, examination, and medical decision-making, often seen in chronic disease management.
Proper use of 99214 requires detailed documentation covering all three key components. Providers must specify the conditions managed, the complexity of decisions, and the time spent. With higher reimbursement comes increased payer scrutiny and a greater risk of audits, especially if documentation does not fully support the service level.
Payers may deny claims for 99214 due to insufficient detail, vague clinical notes, or mismatched diagnoses. Common pitfalls include under-documenting the decision-making process or omitting relevant exam findings. An example is billing 99214 for a diabetes follow-up where medication adjustments and risk factor counseling are thoroughly documented.
For 2026, the AMA releases CPT 2026 code set introduces updated E/M guidelines, emphasizing time-based coding and clarifying requirements for moderate complexity. Healthcare organizations need to align their codes for medical billing with these changes to maintain compliance and maximize reimbursement.
3. HCPCS Code G0463: Hospital Outpatient Clinic Visit
Among essential codes for medical billing in facility settings, HCPCS code G0463 is used for hospital outpatient clinic visits. This code is specific to facility billing and differs from physician E/M codes, making correct application vital for compliance.
G0463 covers evaluation and management services provided in a hospital outpatient department. Documentation must include the patient’s presenting problem, assessment, and the scope of care delivered by hospital staff. Accurate charge capture is necessary, as payers closely monitor claims for duplication or overlap with physician services.
Common errors include billing G0463 for services that do not meet outpatient criteria or failing to distinguish between facility and professional components. Compliance pitfalls involve incomplete documentation or billing the code in conjunction with unrelated procedures.
An example scenario is a patient visiting a hospital-based clinic for hypertension management, where the clinical team provides assessment and care coordination. In 2026, CMS payment policy changes refine the requirements for outpatient billing, reinforcing the need for healthcare organizations to apply codes for medical services correctly and ensure audit readiness.
4. CPT Code 99457: Remote Physiologic Monitoring Treatment Management
CPT code 99457 is a pivotal code for medical practices embracing digital health in 2026. It reimburses for remote physiologic monitoring (RPM) treatment management, supporting the shift toward telehealth and chronic care management.
To bill 99457, providers must document at least 20 minutes of clinical staff or physician/qualified healthcare professional time in a calendar month, overseeing patient data and making treatment decisions. Eligible devices include blood pressure monitors, glucose meters, and wearable cardiac devices. Patient criteria typically require a chronic condition benefiting from ongoing monitoring.
Documentation should detail the data reviewed, clinical actions taken, and patient communication. RPM opens new revenue streams for practices managing high-risk populations, such as cardiology or endocrinology groups. A typical use case: a cardiology clinic monitors a patient’s blood pressure remotely, reviews data trends, and adjusts therapy as needed, all documented under codes for medical billing.
Regulatory updates in 2026 expand coverage for RPM services, with payers clarifying allowable devices and patient populations. Staying current with these changes is crucial for optimizing reimbursement and maintaining compliance.
5. ICD-10-CM Code E11.9: Type 2 Diabetes Mellitus Without Complications
ICD-10-CM code E11.9 is one of the most widely used codes for medical billing, representing type 2 diabetes mellitus without complications. Its prevalence reflects the high burden of diabetes in the patient population and the importance of chronic disease management.
Accurate use of E11.9 requires documentation confirming the diagnosis and absence of complications such as nephropathy or retinopathy. Providers should specify glucose control, treatment regimens, and any coexisting conditions. Supporting evidence in the medical record is essential for risk adjustment and quality reporting.
Payers frequently request documentation to verify the absence of complications, as incorrect coding can distort risk scores or impact value-based payments. An example: a primary care provider sees a patient for routine diabetes management, with stable labs and no evidence of complications, appropriately using E11.9 in codes for medical billing.
2026 coding guidance emphasizes granularity, urging providers to update codes if new complications arise or if the patient transitions to insulin dependence. Staying vigilant with updates ensures accurate reporting and supports optimal reimbursement.
6. CPT Code 99406: Smoking and Tobacco Use Cessation Counseling
CPT code 99406 is increasingly important among preventive care codes for medical billing. It covers intermediate smoking and tobacco use cessation counseling, typically for sessions lasting 3 to 10 minutes.
To bill 99406, providers must document the time spent, topics discussed, and specific counseling interventions. Payer policies often set limits on frequency and total sessions covered per year, so tracking utilization is critical for compliance.
Clinical scenarios include counseling patients during annual wellness visits or addressing tobacco use in chronic disease management. For example, a family medicine provider documents a 7-minute session discussing cessation strategies and resources, correctly applying 99406 in their codes for medical billing.
Public health initiatives in 2026 further incentivize tobacco cessation, with payers offering quality bonuses for documented counseling. CPT updates this year clarify documentation requirements and may adjust time thresholds, making it essential for healthcare organizations to review and adapt workflows accordingly.
7. Modifier 25: Significant, Separately Identifiable E/M Service
Modifier 25 is one of the most scrutinized modifiers in codes for medical billing, applied to indicate a significant, separately identifiable evaluation and management (E/M) service performed on the same day as another procedure.
Proper use of Modifier 25 requires that the E/M service is distinct from the procedure or service performed. Documentation must support the medical necessity and demonstrate that the additional work was above and beyond the usual pre- and post-procedure care.
Common misuse includes applying Modifier 25 when the E/M service is not clearly separate or when documentation is insufficient, leading to payer audits and denials. For example, a provider evaluates a patient for a new problem and also performs a minor procedure, with both services thoroughly documented and Modifier 25 appropriately appended.
Denial trends in 2026 show increased payer education and audit focus on Modifier 25 usage. Best practices for compliance include regular staff training, internal audits, and clear documentation linking services. Using Modifier 25 accurately in codes for medical billing safeguards revenue and ensures regulatory adherence.
Best Practices for Accurate Medical Billing and Documentation
Accurate documentation is the backbone of successful codes for medical in any healthcare organization. Precision in clinical notes, billing, and compliance processes ensures clean claims, reduces denials, and supports financial stability. By focusing on best practices, providers can maximize reimbursement and maintain regulatory confidence.
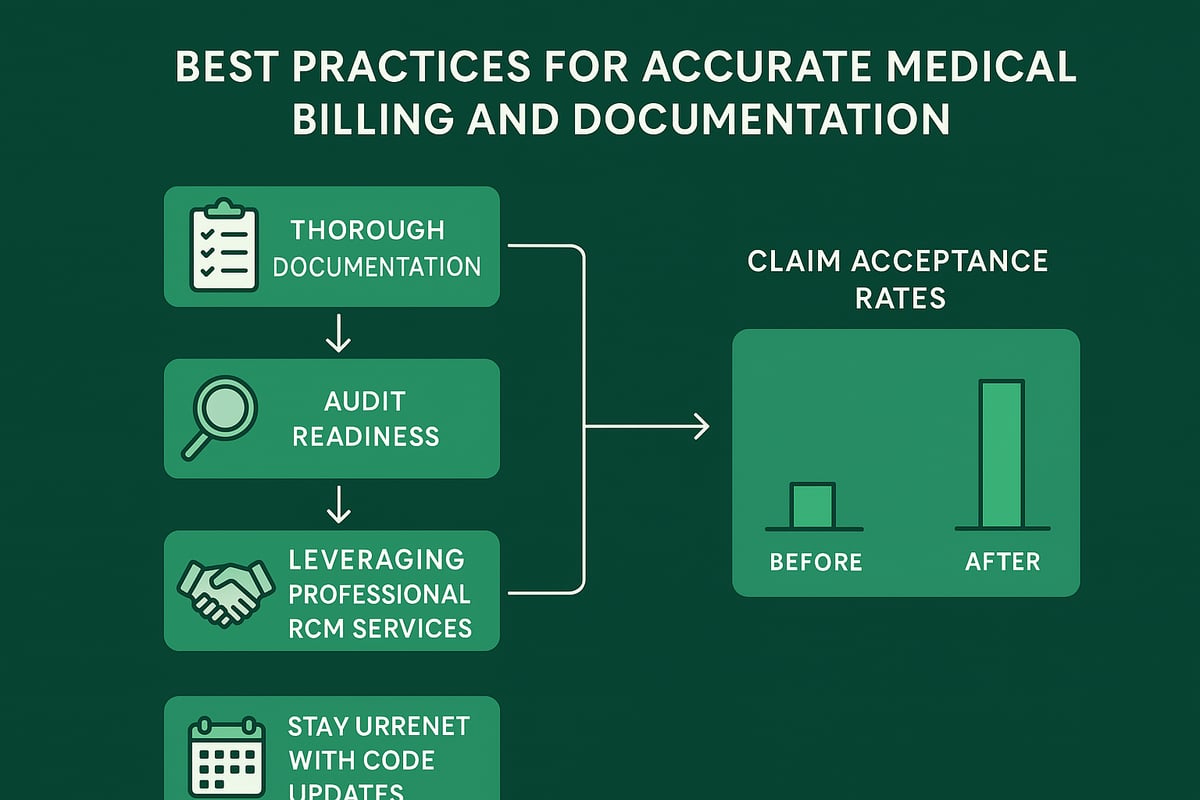
Documentation Strategies for Clean Claims
Thorough clinical notes are the foundation for selecting the right codes for medical and achieving clean claims. Every service provided should be clearly documented, linking the clinical findings directly to code selection.
Using standardized templates and checklists helps ensure consistency. For example, a checklist for E/M visits can prompt providers to record all necessary elements, supporting higher-level codes for medical when appropriate.
A well-structured note not only supports claims but also stands up under payer audits. By embedding these documentation strategies into daily workflows, practices can see fewer denials and faster payments.
Audit Readiness and Compliance
Regular chart reviews and peer audits are essential for audit readiness. Being proactive about compliance means identifying and correcting issues before they lead to costly denials or penalties.
Internal audits should focus on high-risk areas, such as documentation supporting codes for medical that drive significant revenue or are prone to payer scrutiny. Addressing common compliance risks, like upcoding or incomplete records, helps maintain trust with payers and regulators.
For instance, practices that schedule quarterly compliance reviews are better equipped to identify patterns and implement corrective action swiftly.
Leveraging Professional Billing Services
Outsourcing to certified revenue cycle management providers brings specialized expertise to your billing operations. Experienced professionals stay current on payer rules and code updates, ensuring that codes for medical are always accurate and compliant.
Partnering with an RCM firm can reduce denials and improve cash flow, as these teams are skilled in navigating complex billing environments. For example, practices leveraging external RCM services often see a significant increase in first-pass claim acceptance rates.
If you are evaluating whether to build internal expertise or seek external support, this article on Is Medical Billing and Coding Hard? provides valuable insights into the skills required for success.
Staying Current with Code Updates
Staying ahead of annual changes from CMS, AMA, and other payers is crucial for anyone working with codes for medical. Monitoring updates, attending training sessions, and utilizing industry alerts ensures your team remains compliant and efficient.
Ongoing staff education is key. Encourage team members to attend webinars or review resources such as the 2026 ICD-10-CM Medical Coding Updates to stay informed about new or revised codes for medical.
By adapting quickly to updates, healthcare organizations can avoid costly errors and capitalize on new billing opportunities.
Future Trends in Medical Coding and Documentation
As healthcare organizations plan for the future, understanding where codes for medical billing and documentation are headed is vital. The industry is shifting rapidly, with technology, regulations, and workforce needs all influencing how providers manage their revenue cycle in 2026.
Technology Integration and Automation
AI and automation are transforming how codes for medical billing are selected and validated. Many organizations now use EHR-integrated coding tools that suggest relevant codes for medical services, streamlining workflows and improving accuracy. These tools boost coder productivity, allowing professionals to focus on complex cases and exceptions.
Despite these advances, professional oversight remains crucial. Automated platforms can reduce errors but may miss crucial context or nuances in documentation. RCM service providers play a key role in bridging this gap, ensuring that technology enhances rather than replaces expert judgement. Clinics that combine automation with skilled oversight consistently achieve higher clean claim rates.
Evolving Regulatory Requirements
Regulatory changes are reshaping the landscape for codes for medical documentation. CMS and commercial payers are introducing new code sets, with a strong focus on social determinants of health, telehealth, and digital health services. Providers must adapt quickly to expanded transparency requirements and more frequent data sharing.
Staying updated is essential. For example, the ICD-10 & Other Coding Revisions to National Coverage Determinations: April 2026 Update details important changes affecting reimbursement. Proactive monitoring of these updates helps organizations avoid costly denials and maintain compliance in a rapidly evolving environment.
Workforce Development and Training
The demand for skilled professionals who understand codes for medical billing is at an all-time high. Certification programs, such as CPC and CCS, are more important than ever. Ongoing education, including webinars like the 2026 CPT® Coding Updates – AAPC Webinar, keeps staff current with new code sets and payer rules.
Partnering with experienced RCM service providers ensures organizations benefit from up-to-date expertise and best practices. Many clinics are investing in coding bootcamps and online training to build a future-ready workforce capable of handling the complexities of 2026 and beyond.
As you’ve just seen, mastering the right billing codes is key to staying ahead in today’s fast-changing healthcare landscape. Accurate documentation and code selection not only improve your financial performance—they help safeguard your practice from denials and compliance risks. If you’re ready to optimize your revenue cycle, ensure seamless operations, and keep up with evolving industry standards, let’s connect. You don’t have to navigate these complexities alone—we’re here to help you succeed.
Book Your Free Consultation
and discover how Greenhive Billing Solutions can support your practice’s growth and compliance in 2026 and beyond.