In 2026, healthcare organizations are navigating unprecedented financial pressures, new regulations, and increasingly complex payer relationships. Staying ahead in this environment demands a proactive, data-driven approach to every aspect of your revenue cycle.
Healthcare revenue cycle analytics has become the cornerstone for making informed financial decisions. By mastering analytics, healthcare leaders can unlock greater efficiency, reduce costly denials, and set the stage for sustainable growth.
This comprehensive guide is designed to provide a step-by-step blueprint for success in healthcare revenue cycle analytics. We will cover core concepts, essential metrics, technology trends, best practices, and actionable strategies to help your organization optimize revenue cycle performance in the year ahead.
Understanding Healthcare Revenue Cycle Analytics in 2026
Defining Revenue Cycle Analytics
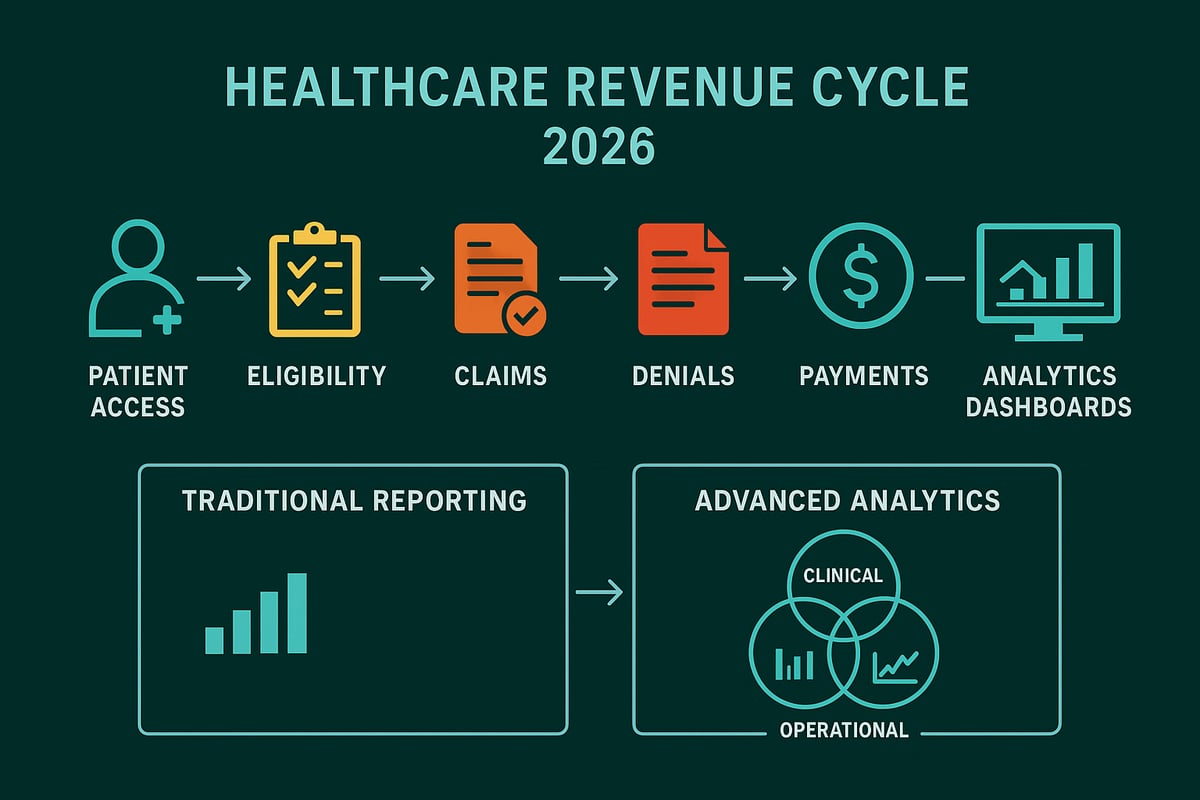
Healthcare revenue cycle analytics is the systematic process of collecting, integrating, and interpreting data across the full revenue cycle. This includes patient access, eligibility verification, charge capture, billing, collections, and final payment reconciliation. Unlike static or retrospective reporting, healthcare revenue cycle analytics leverages advanced tools to provide real-time insights and predictive trends.
A modern approach integrates clinical, financial, and operational data for a holistic view. Examples of data analyzed include claims submissions, denial rates, accounts receivable balances, and payment posting accuracy. By adopting robust reporting and analytics in medical billing, organizations move beyond basic reporting into actionable analysis that drives improvement.
Why Revenue Cycle Analytics Matters Now More Than Ever
In 2026, healthcare organizations are under pressure from tighter reimbursement policies and evolving regulations. Fragmented data from multiple EHR and billing systems makes unified visibility a challenge. With margins shrinking and operational costs rising, the need for healthcare revenue cycle analytics is at an all-time high.
Competitors are leveraging analytics to minimize financial risk. For top hospitals, as much as $300 million is at stake due to unresolved denials. Analytics play a crucial role in supporting value-based care initiatives and maintaining compliance by making data-driven decisions possible.
Core Components of a Modern Analytics Program
A successful healthcare revenue cycle analytics program rests on several pillars. First, it requires consolidating data from disparate systems for a single source of truth. Real-time dashboards and KPI monitoring enable organizations to respond quickly to trends or issues. Predictive analytics help forecast cash flow, denial rates, and reimbursement scenarios, empowering proactive decision-making.
Benchmarking tools allow organizations to measure performance against industry standards and identify improvement opportunities. Visual dashboards, scenario planning, and contract modeling are essential examples of how analytics drive efficiency.
Challenges and Barriers to Effective Analytics
Despite the benefits, organizations face significant barriers when implementing healthcare revenue cycle analytics. Data silos and poor interoperability can limit the ability to gain comprehensive insights. The lack of standardized metrics and inconsistent data quality often undermine analytics reliability.
Change management is another hurdle, as staff may resist new tools or processes. Limited resources, whether technology, skilled personnel, or expertise, further complicate adoption. For example, relying on manual denial analysis can lead to inefficiency and missed revenue opportunities.
Essential Revenue Cycle Metrics and KPIs for Success
Identifying and tracking the right metrics is the foundation for optimizing healthcare revenue cycle analytics in 2026. With financial pressures mounting and payer complexity increasing, a focused approach to KPIs empowers organizations to make proactive, data-driven decisions. The following categories outline the essential metrics that drive revenue cycle performance and long-term sustainability.
![]()
Key Financial Metrics Every Healthcare Organization Must Track
Financial KPIs are the backbone of healthcare revenue cycle analytics, providing a clear view of organizational health. The most critical metrics to monitor include:
- Clean Claims Rate: Measures the percentage of claims accepted on the first submission. A high rate accelerates cash flow and reduces rework.
- Denial Rate and Root Cause Analysis: Tracks the frequency of denied claims, highlighting issues in eligibility, coding, or documentation.
- Days in Accounts Receivable (A/R Days) and Gross Days Receivable Outstanding (GDRO): Indicates the average time to collect payments, impacting liquidity.
- Net Patient Service Revenue (NPSR) and Operating Margins: Evaluates profitability by comparing revenue collection against operating costs.
- Cash Flow Forecasting (30/60/90-day horizons): Enables leaders to anticipate revenue trends and manage resources effectively.
For a more detailed breakdown of these KPIs and their impact on healthcare revenue cycle analytics, see the Top Revenue Cycle KPIs for 2025. Regular monitoring of these indicators ensures timely identification of issues and supports strategic decision-making.
Operational and Process Metrics
Operational KPIs help pinpoint inefficiencies and workflow challenges across the revenue cycle. Key metrics include:
- Claims Submission Timeliness and Accuracy: Tracks how quickly and correctly claims are filed, reducing delays and denials.
- Rate of Manual Intervention: Monitors the percentage of claims requiring manual processing, a signal for automation opportunities.
- Time Spent on Data Gathering and Reporting: Measures reporting efficiency, with analytics often reducing this by up to 20 percent.
- Staff Productivity Benchmarks: Compares team performance to industry standards, identifying training or resource needs.
By integrating these metrics into your healthcare revenue cycle analytics strategy, organizations can streamline operations and enhance productivity.
Denial Management and Revenue Leakage Indicators
Denials and revenue leakage are persistent threats to financial performance. Robust healthcare revenue cycle analytics should focus on:
- Frequency and Types of Denials: Analyze eligibility, coding, and authorization denials to address root causes.
- Underpayment Rates and Contract Compliance: Identify discrepancies between expected and actual payments.
- Revenue Leakage Points: Track missed charges, write-offs, and underpayments across the cycle.
- Denial Trend Analysis Tools: Leverage data to reduce manual processes by up to 90 percent and recapture lost revenue.
Continuous analysis in these areas leads to measurable improvements in collections and reduces preventable losses.
Benchmarking and Performance Comparison
Benchmarking is essential for setting realistic goals and driving continuous improvement in healthcare revenue cycle analytics. Organizations should:
- Conduct Internal Benchmarking: Compare performance across departments or locations to highlight best practices and outliers.
- Use External Benchmarking: Evaluate metrics against national and regional peers to identify competitive gaps.
- Scenario Planning: Assess contract scenarios before payer negotiations to optimize reimbursement terms.
Effective benchmarking uncovers improvement opportunities and fosters a culture of accountability.
Turning Metrics into Actionable Insights
Collecting data is only the first step. Transforming metrics into actionable insights is key to unlocking the full value of healthcare revenue cycle analytics.
For example, leveraging payer performance data can help prioritize negotiation strategies, moving organizations from reactive to proactive revenue cycle management. This approach ensures every metric drives tangible business outcomes.
Step-by-Step Guide to Implementing Revenue Cycle Analytics in 2026
Implementing healthcare revenue cycle analytics is a multi-phase process that demands strategic planning, collaboration, and continual refinement. This step-by-step guide outlines how healthcare organizations can build a robust analytics program, unlock actionable insights, and drive measurable financial improvements in 2026.
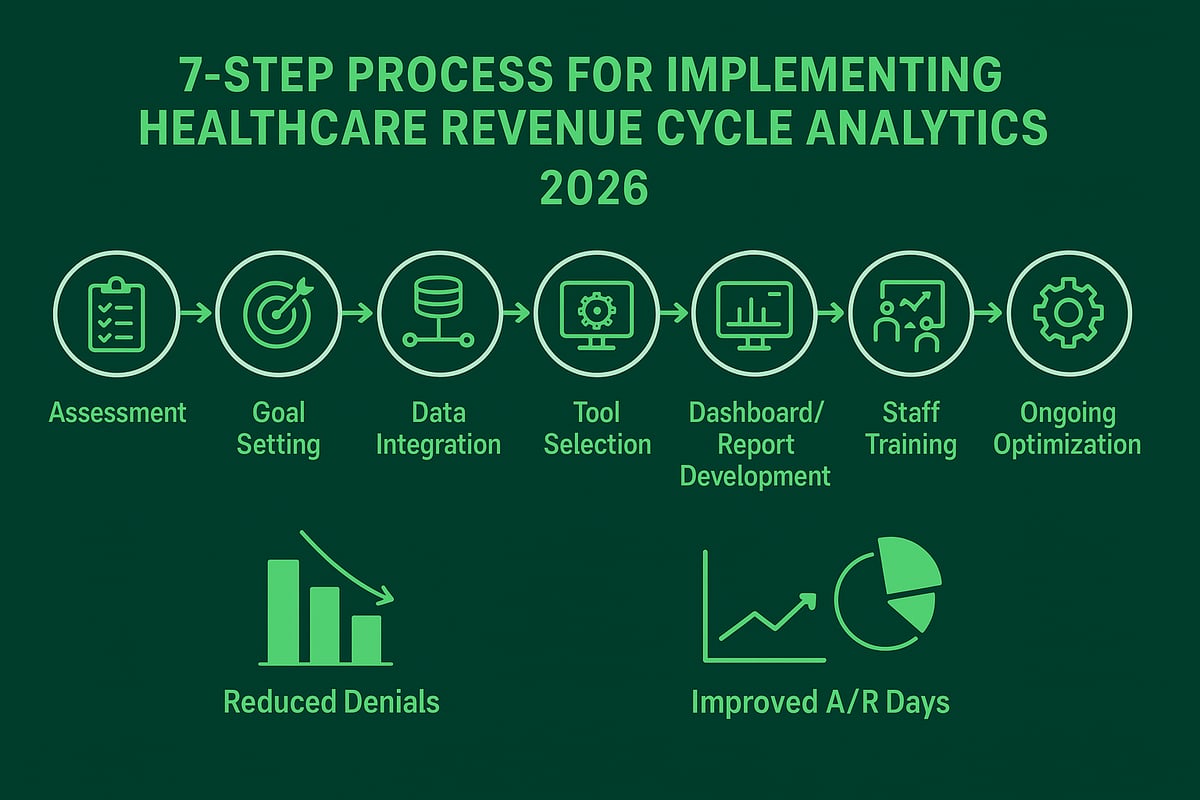
Step 1: Assess Current Analytics Capabilities
Begin by thoroughly evaluating your organization’s current state in healthcare revenue cycle analytics. Inventory all data sources, including EHR, billing, scheduling, and financial systems.
Map out your existing analytics workflows, identifying strengths and gaps. Are data collection and reporting processes manual or automated? Review staff expertise, available technology, and workflow integration.
Establish baseline metrics for key performance indicators, such as denial rates and A/R days. Visualize the entire patient-to-payment journey to highlight inefficiencies and opportunities for data capture. This initial assessment sets the foundation for targeted improvements and informs future investments in healthcare revenue cycle analytics.
Step 2: Set Clear Goals and Success Criteria
Define specific, measurable objectives for your healthcare revenue cycle analytics initiative. Examples include reducing denial rates by 15 percent or cutting A/R days by 10 percent over the next year.
Align these goals with your broader organizational strategy to ensure analytics efforts support business priorities. Engage stakeholders from finance, IT, clinical, and operations teams to gain buy-in and diverse perspectives.
Use the SMART framework (Specific, Measurable, Achievable, Relevant, Time-bound) to clarify targets and success criteria. Prioritize analytics projects with the highest potential impact, ensuring resources are focused where they matter most in healthcare revenue cycle analytics.
Step 3: Integrate and Standardize Data
Consolidating data from disparate systems is crucial for effective healthcare revenue cycle analytics. Integrate EHR, billing, scheduling, and financial information into a unified platform, addressing data quality and consistency issues.
Implement robust data governance policies to ensure accuracy, completeness, and compliance. Overcome interoperability challenges by adopting industry-standard formats and APIs.
Centralize claims, payments, and denial data for holistic analysis. Standardization enables real-time visibility and supports advanced analytics, enhancing your ability to spot trends and optimize processes across the entire revenue cycle.
Step 4: Select Tools, Platforms, and Partners
Choose analytics tools and platforms that align with your organization’s needs and existing infrastructure. Evaluate options such as cloud-based dashboards, visualization tools, and reporting solutions that support healthcare revenue cycle analytics.
Assess vendor capabilities, ensuring they offer healthcare-specific features, scalability, and robust security (including HIPAA compliance). Consider how partners can support your analytics journey, especially if your organization relies on external expertise for RCM.
Ensure seamless integration with current systems, focusing on flexibility and adaptability. This approach allows your analytics program to grow alongside your organization and evolving industry demands.
Step 5: Develop Analytics Dashboards and Reports
Design intuitive dashboards for real-time monitoring of KPIs relevant to healthcare revenue cycle analytics. Customize reports for various user roles, from executives to billing staff, ensuring each stakeholder has access to actionable insights.
Visualize trends, identify outliers, and highlight opportunities for intervention. Automate recurring reports to minimize manual work and accelerate data-driven decisions. For insights on optimizing denial tracking and report automation, see Denial management best practices.
Incorporate predictive models for forecasting denial trends and reimbursement scenarios. Well-crafted dashboards empower teams to act quickly, address issues proactively, and drive continuous improvement.
Step 6: Train Staff and Foster Data-Driven Culture
Empowering your team is essential for successful healthcare revenue cycle analytics adoption. Provide comprehensive training on analytics tools, data interpretation, and reporting best practices.
Encourage cross-functional collaboration among finance, billing, clinical, and IT teams. Assign clear ownership of key metrics to foster accountability and transparency.
Promote a culture where data informs decision-making at every level. Regularly communicate results, celebrate wins, and address challenges openly. When staff are engaged and data-literate, analytics initiatives gain momentum and deliver stronger outcomes.
Step 7: Monitor, Iterate, and Optimize
Continuous monitoring is the final pillar of effective healthcare revenue cycle analytics. Track KPIs regularly, using benchmarking and feedback loops to identify areas for refinement.
Adapt strategies based on real-world results and evolving organizational needs. Hold periodic reviews to celebrate successes, document lessons learned, and set new improvement targets.
Organizations that embrace a cycle of monitoring, iteration, and optimization consistently outperform peers, achieving lasting gains in revenue, efficiency, and compliance through healthcare revenue cycle analytics.
Leveraging Analytics to Optimize Denials Management and Collections
Healthcare revenue cycle analytics is transforming how organizations tackle denials, collections, and revenue leakage. By leveraging advanced analytics, providers can proactively identify bottlenecks, improve financial performance, and ensure compliance in a rapidly evolving landscape.
Identifying and Addressing Denial Root Causes
Healthcare revenue cycle analytics empowers organizations to uncover the true drivers behind claim denials. By systematically tracking denial rates by payer, provider, and service line, B2B teams can pinpoint persistent issues such as eligibility errors, coding mistakes, or missing documentation.
For example, analytics platforms enable users to drill down into specific claims, revealing patterns that manual reviews often overlook. Most denials are preventable, so using data-driven insights to implement corrective actions is essential.
- Track denial reasons and frequency by payer
- Analyze trends over time to identify systemic problems
- Prioritize interventions based on financial impact
With healthcare revenue cycle analytics, organizations can move from reactive denial management to proactive prevention, improving cash flow and reducing administrative burden.
Streamlining Collections and Reducing A/R Days
Timely collections are vital for maintaining financial stability. Healthcare revenue cycle analytics allows providers to monitor aging accounts, payment patterns, and collection effectiveness in real time.
By forecasting cash flow and prioritizing follow-up efforts, analytics help B2B teams automate reminders and streamline collection processes. This reduces A/R days and accelerates revenue realization.
Consider these approaches:
- Segment accounts by age and payer for targeted follow-up
- Use predictive analytics to identify accounts at risk of delay
- Automate outreach for outstanding balances
With accurate, actionable insights from healthcare revenue cycle analytics, organizations can optimize workflows, boost staff productivity, and ensure a steady cash flow.
Enhancing Clean Claims Rate and First-Pass Yield
A high clean claims rate reduces costly rework and speeds up reimbursements. Healthcare revenue cycle analytics uncovers rejection patterns, enabling teams to address root causes before submission.
Implementing pre-submission validation checks, eligibility verification, and automated edits ensures claims are accurate and complete. By reducing manual touchpoints, organizations benefit from faster payments and fewer denials.
For more on the metrics and best practices that drive clean claims and coding accuracy, explore medical billing and coding metrics.
- Monitor rejection trends by service line or location
- Automate eligibility and coding checks
- Measure first-pass yield to benchmark process improvements
Healthcare revenue cycle analytics enables providers to achieve industry-leading clean claim rates and maximize reimbursement.
Proactive Revenue Leakage Prevention
Revenue leakage can occur at multiple points in the revenue cycle, from missed charges to underpayments. Healthcare revenue cycle analytics helps B2B teams identify and close these gaps by tracking contract compliance, payment variances, and write-off trends.
Routine audits, reconciliation processes, and contract analysis are essential in quantifying and recovering lost revenue. Analytics-driven reporting makes it possible to visualize leakage points and prioritize recovery strategies.
- Identify underpayments and missed charges
- Benchmark contract terms against actual payments
- Use dashboards to monitor recurring leakage issues
By leveraging healthcare revenue cycle analytics, organizations can capture more revenue and strengthen their financial foundation.
Supporting Value-Based Care and Compliance
Regulatory requirements and value-based care models demand robust analytics and transparent reporting. Healthcare revenue cycle analytics aligns financial performance with clinical quality, ensuring organizations meet payer and compliance standards.
Tracking performance on value-based contracts, monitoring regulatory changes, and adapting documentation practices are all streamlined through advanced analytics. This supports both short-term revenue goals and long-term organizational growth.
- Align analytics with quality and compliance measures
- Track incentive payments and penalties
- Adapt to changing regulations with flexible analytics tools
Healthcare revenue cycle analytics positions B2B providers for sustained success in an increasingly complex regulatory environment.
Technology Trends and Future Directions in Revenue Cycle Analytics
Staying ahead in healthcare revenue cycle analytics requires a keen understanding of emerging technologies and best practices. As the industry evolves, strategic leaders must harness innovation to drive efficiency, accuracy, and compliance. Let us explore the most impactful trends shaping the future of analytics in healthcare revenue management.
The Rise of Predictive and Prescriptive Analytics
Healthcare revenue cycle analytics now goes far beyond traditional reporting. Organizations increasingly use predictive analytics and machine learning to anticipate denials, forecast reimbursement, and model cash flow scenarios. These advanced techniques enable proactive decision-making and optimize resource allocation.
AI-driven solutions identify patterns in claims, denials, and payment data, allowing teams to intervene before issues escalate. Prescriptive analytics takes this a step further, recommending best actions based on real-time insights. According to Key Revenue Cycle Management Trends 2025, AI is transforming denial prevention and resolution, setting a new standard for analytics maturity. By leveraging these capabilities, healthcare organizations can improve financial outcomes and strengthen payer negotiations.
Data Security, Privacy, and Compliance in 2026
With the expansion of healthcare revenue cycle analytics, data security and privacy are top priorities. Practices must ensure all analytics platforms meet HIPAA standards, employ robust encryption, and maintain strict access controls. Secure cloud-based environments offer scalability and cost-effectiveness, but they require ongoing risk assessments and regular audits.
Compliance is not static. As regulations shift, analytics programs must adapt quickly to new requirements. A strong focus on security protects sensitive patient and financial data, while also supporting a cost-effective approach to revenue cycle management. Ultimately, safeguarding data is essential for trust and long-term success.
Interoperability and Unified Data Platforms
Breaking down silos is essential for effective healthcare revenue cycle analytics. Unified data platforms connect EHRs, billing systems, and financial tools, enabling a holistic view of the revenue cycle. Real-time data exchange supports faster, more informed decisions and uncovers hidden trends.
Industry standards for interoperability are improving, making seamless integration more achievable. Research on AI-Enabled Orchestration in Healthcare ERP highlights how AI can enhance workflow efficiency across disparate systems. Centralized analytics platforms empower teams to monitor performance, benchmark results, and streamline operations, resulting in greater visibility and efficiency.
The Human Element: Analytics-Driven Culture and Change Management
Technology alone does not guarantee success in healthcare revenue cycle analytics. Building an analytics-driven culture is equally important. Leadership must champion analytics initiatives, foster collaboration between IT, finance, and clinical teams, and provide ongoing training for staff.
Empowering teams with data literacy enables smarter decisions and accountability. Change management strategies, such as regular communication and celebrating wins, help drive adoption and sustain momentum. Organizations that invest in their people, as well as their technology, consistently achieve analytics maturity and measurable results.
Best Practices and Actionable Strategies for Analytics Success
Building a robust healthcare revenue cycle analytics program requires more than just technology. It calls for strategic alignment, skilled teams, and a culture that values actionable insights. Below, we outline best practices that empower healthcare organizations to excel in analytics-driven revenue cycle management.
Building a Data-Driven Revenue Cycle Team
A high-performing healthcare revenue cycle analytics team blends financial, clinical, and operational expertise. Define clear roles for analysts, revenue integrity specialists, and process owners. Cross-training staff increases flexibility and helps teams interpret data from various sources, such as claims and denials.
Regular performance reviews and feedback sessions foster accountability. Encourage continuous learning about analytics trends and data elements, including revenue codes in billing, which are essential for accurate reporting and compliance. Teams that own their metrics drive measurable improvements across the revenue cycle.
Aligning Analytics with Organizational Strategy
Healthcare revenue cycle analytics should align with the broader business vision. Integrate analytics objectives into strategic planning and resource allocation. Use analytics to support expansion decisions, service line growth, and margin improvement.
Communicate analytics outcomes to stakeholders at all levels to build buy-in and transparency. For example, when analytics reveal underperformance in a specific department, leadership can prioritize targeted interventions. Aligning financial and clinical priorities ensures analytics initiatives contribute to both profitability and quality care.
Partnering with Expert Revenue Cycle Service Providers
External service partners bring specialized knowledge and industry best practices to healthcare revenue cycle analytics. By leveraging these partnerships, organizations benefit from scalable solutions, cost efficiencies, and faster return on investment.
Expert providers support process improvement using industry-standard tools and proven methodologies. Outsourcing complex tasks, such as denial management and advanced analytics, frees internal teams to focus on higher-value work. Ensure service providers collaborate closely with internal teams and maintain compliance with all relevant standards.
Greenhive Billing Solutions: Enhancing Revenue Cycle Analytics Outcomes
Greenhive Billing Solutions elevates healthcare revenue cycle analytics through a service-based, client-focused approach. Our experienced professionals integrate seamlessly with your existing software and systems, adapting to unique workflows.
We specialize in claims processing, eligibility verification, denial management, and revenue analytics. Our transparent, HIPAA-compliant processes maximize reimbursements, reduce A R days, and deliver real-time insights to support your financial goals. Practices partnering with Greenhive achieve higher clean claims rates, faster collections, and demonstrable improvements in financial performance.
Continuous Improvement and Innovation
The healthcare revenue cycle analytics landscape evolves rapidly. Establish regular feedback mechanisms to refine analytics programs and update KPIs as business needs change.
Invest in ongoing staff education and upgrade technology to maintain a competitive edge. Monitor industry trends, such as those highlighted in U.S. Healthcare RCM Market Growth Projections, to proactively adapt strategies. Organizations that iterate and innovate consistently achieve year-over-year improvements in revenue cycle outcomes.
As you look ahead to 2026, mastering revenue cycle analytics isn’t just about keeping up—it’s about unlocking real improvements in your healthcare organization’s financial health. With the right insights, you can reduce denials, speed up collections, and drive sustainable growth, all while staying compliant and efficient. If you’re ready to take the next step and see how tailored analytics solutions can transform your revenue cycle, I invite you to connect with a team that truly understands the challenges and opportunities ahead. Let’s work together to maximize your outcomes—Book Your Free Consultation today.